Thoracic outlet syndrome: first rib resection
Introduction
Thoracic outlet syndrome (TOS) is caused by compression of neurovascular structures in the costoclavicular space. The symptoms of the patients depend on the anatomic structure that is being compressed. Therefore TOS is divided in three groups, neurogenic TOS (NTOS; which is most frequently encountered 90%–95%), venous TOS (VTOS; 5%) and, least commonly, arterial TOS (ATOS; 1%) (1).
Repetitive compression of the subclavian vein between the first rib, clavicle and associated muscles leads to vessel wall and intimal damage, stenosis and eventually thrombosis. Similarly the subclavian artery can be compressed leading to distal embolization, stenosis, aneurysmal degeneration or occlusion.
The objective diagnosis of NTOS is a challenge and generally accepted “golden” diagnostic criteria are lacking (1,2). The mainstay of management is nonsurgical in most patients; however, surgery is indicated for patients with persisting symptoms despite conservative management and when vascular structures are involved.
Surgical therapy consists of decompression of the thoracic outlet by performing a first rib resection with or without adjunctive vascular reconstructive procedures. First rib resection can be performed through a transaxillary (3), supraclavicular (4) and infraclavicular (5) approach. Thoracoscopic (assisted) procedures are also described in the recent literature but are beyond the scope of this book chapter.
Operative techniques
Transaxillary approach
Preparation & exposure
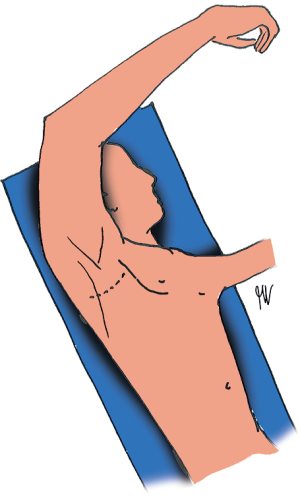
The patient is placed on a vacuum mattress in a 45 degrees posterolateral position on the operating table with the ipsilateral side facing upward. The hand, axilla, chest and back are scrubbed and draped to expose the axilla and the ipsilateral arm is draped in a sterile stockinet to allow manipulation by an assistant. The arm is abducted to 90 degrees and flexed at the elbow to allow positioning in a support (Figure 1). The operating surgeon stands on the dorsal side of the patient. Note that some surgeons prefer not to position the arm in a support to allow free manipulation by an assistant. The assistant can elevate the shoulder by applying subtle traction to increase exposure during the procedure. As long as this is performed with care the risk of injury to the brachial plexus is negligible. Due to the depth of the operating field and small working space, the use of a headlight is recommended.
It is also recommended to have two assistants available, one for manipulating the arm to improve exposure of the thoracic outlet and a second assistant to hold retractors/specula during the procedure.
Surgical technique
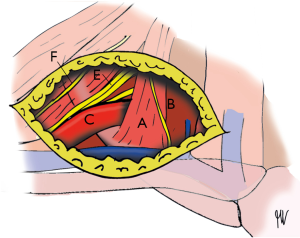
A transverse incision (6–8 cm is usually sufficient) is made in the skin lines along the inferior border of axillary hair (Figure 1, dashed line). This is usually at the level of the third rib if the patient is positioned as described above. The incision is carried directly toward the chest wall avoiding the layer of fatty tissue containing the axillary lymph nodes. The anterior border of the latissimus dorsi muscle and the dorsal border of the major pectoral muscle are released and care is taken to spare the thoracodorsal and long thoracic nerves. The dissection is carried upward directly along the chest wall to the first rib (Figure 2). From the second intercostal space the intercostobrachial nerve usually crosses the operating field. It may be sacrificed although frequently it can be readily retracted and spared. The first rib has a broader and flatter shape compared to the other ribs. A retractor can be placed at this point or exposure can be improved by using sympathectomy specula. To further expose the thoracic outlet and its vital structures the shoulder can be manipulated vertically by an assistant. It is important to apply careful hemostasis during the dissection because even relative small bleedings can significantly impair visualization in the operating field. The ventral aspect of the first rib can be exposed by blunt dissection and the brachial plexus is revealed posteriorly, the subclavian artery and anterior scalene muscle medially and the subclavian vein ventrally (Figure 2).
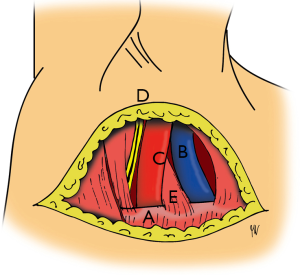
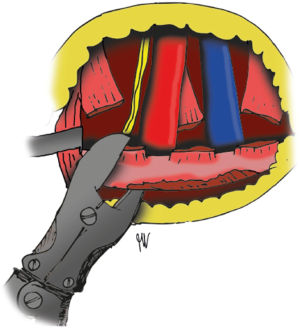
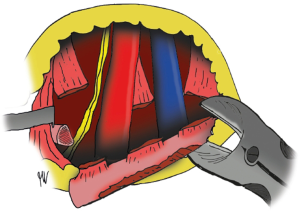
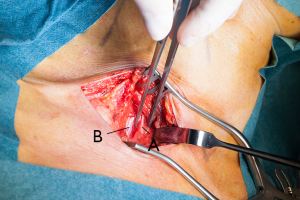
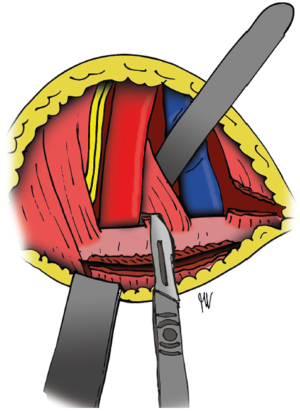
Before the first rib can be removed, attached structures must be dissected. The intercostal muscles can be dissected from the inferior border of the rib from the manubrium sterni anteriorly to the transverse process posteriorly using diathermia avoiding injury to the thoracodorsal and long thoracic nerves (Figure 3). Try to leave the parietal pleura intact, it can be digitally detached from the posterior aspect of the first rib after dissection of the intercostal muscles. Dorsal to the subclavian vein the anterior scalene muscle insertion is visualized. It can bluntly be freed from surrounding tissue on the posterior side using a dissecting forceps and divided through the insertion close to the first rib using scissors or a scalpel (Figure 4). Diathermia is avoided due to possible phrenic nerve injury. If present, the insertion of the scalenus minimus muscle can be detached from the posterior aspect of the first rib at this point, just dorsal to the insertion of the anterior scalene muscle insertion. In a similar fashion the middle scalene muscle insertion can be detached from the first rib, just posterior to the subclavian artery and brachial plexus. Anteriorly, the tendon of the subclavian muscle can be divided from the cartilaginous portion of the first rib taking care of the subclavian vein just posterior to this tendon. The posterior scalene muscle located more dorsally can remain in place. An angled rib cutter (45 or 90 degrees) is used to cut the first rib close to the transverse process posteriorly and the manubrium sterni anteriorly (Figures 5,6). Care is taken to avoid injury to the subclavian vein and brachial plexus while cutting the rib. If a cervical rib is present it is detached from the first rib, dissected posteriorly and cut close to the transverse process. Remaining sharp edges can be smoothened using the rongeur. The brachial plexus and subclavian vessels are inspected and any remaining fibrous strands are removed.
Completion
Wound suction drain is usually sufficient even to allow complete expansion of the lung if defects in the parietal pleura are caused during dissection. By relaxing the arm the surgical field collapses and the wound can be closed by placing a layer of subcutaneous sutures and a layer of intracutaneous sutures. A postoperative chest x-ray can be performed to rule out pneumo- or hematothorax, although this is usually unnecessary in uncomplicated procedures where the parietal pleura remained intact. Adequate postoperative pain relief and early mobilization are important for fast recovery and the drain is removed on the first postoperative day.
Supraclavicular approach
Preparation & exposition
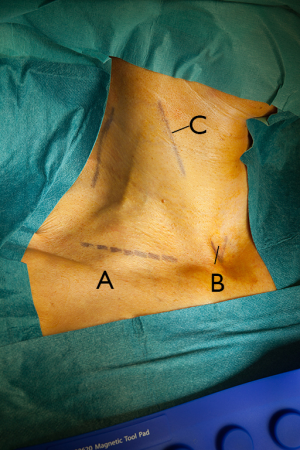
The patient is placed in a supine position with a small pillow under and between the scapulae. The head is turned facing the contralateral side. The neck, shoulder and chest are scrubbed and draped to expose the area around the clavicle (Figure 7).
Surgical technique
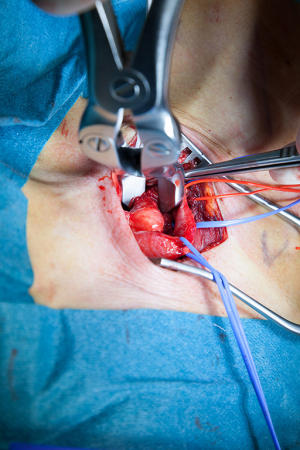
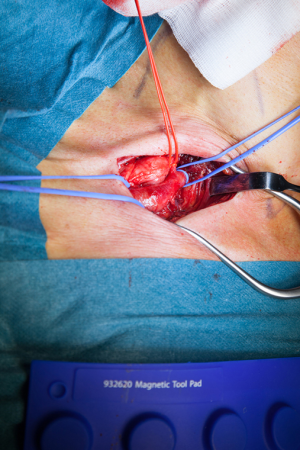
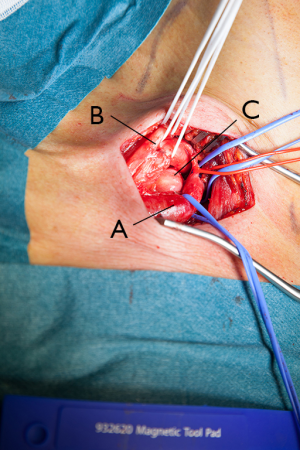
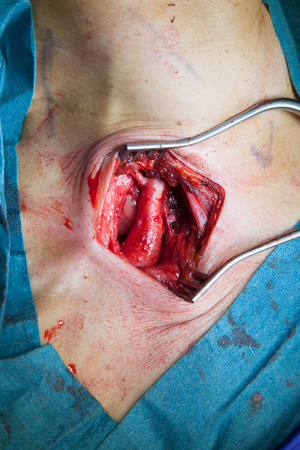
A transverse incision is made parallel to and 2 cm above the clavicle (Figure 7). Supraclavicular nerves are identified and retracted using vessel loops. The platysma is divided followed by the clavicular head of the sternocleidomastoid muscle. The omohyoid muscle is divided and the supraclavicular fat pad is elevated. The dissection is carried toward the anterior scalene muscle and the phrenic nerve can be seen on the anterior surface of this muscle (Figure 8). It can be isolated and retracted using a vessel loop to prevent injury. The brachial plexus is visible posterior to the anterior scalene muscle and the long thoracic nerve runs along the posterior aspect of the middle scalene muscle (Figure 9). The fascia is opened and the anterior scalene muscle is divided using diathermia, or scissors. This exposes the subclavian artery directly behind the divided muscle allowing arterial reconstruction if necessary. The artery is controlled by placing a vessel loop (Figure 10). The trunks of the brachial plexus are mobilized and carefully retracted avoiding traction injury (Figure 11). The middle scalene muscle can now be divided from the first rib avoiding injury to the long thoracic nerve that runs posterior to or even through the middle scalene muscle at this level. The C8 and T1 nerve roots are seen above and below the first rib. The brachial plexus is carefully retracted to allow maximum exposure of the first rib after which the rib is cut using an angled (45 or 90 degrees) rib cutter. The rongeur is used to completely remove remnants of the first rib from its attachment to the transverse process preventing new bone formation and potential recurrence of symptoms. The anterior segment of the first rib is also removed. In a similar fashion a cervical rib can be removed using the angled (45 or 90 degrees) rib cutter (Figures 12,13).
Completion
Careful hemostasis is applied and the clavicular head of the sternocleidomastoid muscle may be reinserted to the clavicle. The wound is closed over a wound suction drain. The platysma is sutured followed by intracutaneous sutures for the skin. A postoperative chest X-ray can be performed to rule out pneumothorax, although this is usually unnecessary in uncomplicated procedures where the parietal pleura remained intact. Postoperative early mobilization is advised and the drain is removed on the first postoperative day. Adequate pain relief is warranted.
Infraclavicular approach
Preparation & exposition
The patient is placed in a supine position with a small pillow under and between the scapulae. The head is turned facing the contralateral side. The ipsilateral arm is positioned cephalad. The neck, shoulder, chest and ipsilateral arm are scrubbed and draped to expose the area around the clavicle. The arm is draped in a sterile stockinet to allow manipulation by an assistant to improve exposure when necessary.
Surgical procedure
A transverse incision is made parallel to and 2 cm caudal to the clavicle from the medial part of the clavicle to the manubrium sterni. Fibers of the clavicular head of the major pectoral muscle are divided identifying the subclavius muscle and the subclavian vein. The subclavius muscle is divided at its insertion on the first rib and excised. The subclavian vein is mobilized freeing it from fibrous tissue on top of the vein. The first rib edges are mobilized bluntly. The insertion of the anterior scalene muscle on the first rib is located just dorsally to the vein. The phrenic nerve, running across the anterior scalene muscle, is isolated and retracted medially followed by division of the anterior scalene muscle insertion close to its attachment to the first rib. Now the subclavian artery and the brachial plexus are visualized and are retracted cranially. At this time exposure might be improved by elevation of the ipsilateral arm by the assistant. The first rib is now completely exposed. The rib is resected using an angled (45 to 90 degrees) rib cutter from its anterior attachment to the manubrium to the posterior attachment to the transverse process. The rib can be detached from the parietal pleura with blunt dissection without damaging the parietal pleura. Sharp bony remnants can be removed using the rongeur. To optimize release of the subclavian vein the costoclavicular ligament medial to the artery can be partially divided. At this point there is adequate exposure of the subclavian vein and distal part of the subclavian artery allowing vascular reconstruction of necessary.
Completion
The wound is closed over a wound suction drain. A postoperative chest X-ray can be performed to rule out pneumothorax, although this is usually unnecessary in uncomplicated procedures where the parietal pleura remained intact. Postoperative early mobilization is advised and the drain is removed on the first postoperative day. Adequate pain relief is warranted.
Comments
First rib resection for thoracic outlet syndrome can be performed through the three approaches described in this chapter. The transaxillary approach is preferred in the majority of cases because it’s safe, does not require division of important muscles and has a superior cosmetic result. Drawback of this approach is the relatively narrow and deep working space. A supraclavicular approach allows better exposure and control of the subclavian artery and is the preferred approach in ATOS, while an infraclavicular approach allows superior access to the subclavian vein and is preferred for the treatment of VTOS.
To optimize exposure during the transaxillary approach it is of vital importance to keep secure hemostasis from the beginning of the procedure, since even minor bleeding can impair vision and hamper identification of vital structures. Another way to importantly improve exposure is having an assistant elevating the shoulder as this opens the thoracic outlet and enlarges the operating field. Releasing the anterior border of the latissimus dorsi muscle and the posterior border of the major pectoral muscle further improves working space and exposure.
The presence of many vital structures travelling through a relatively small and deep operating field implies the risk of injury to any of these structures. Injury to the long thoracic nerve leads to a winged scapula due to denervation of the anterior serratus muscle. Thoracodorsal nerve injury leads to denervation of the latissimus dorsi muscle. The phrenic nerve can be at risk when the anterior scalene muscle is divided and injury causes paralysis of the ipsilateral diaphragm. The majority of patients with thoracic outlet syndrome are young and active patients and nerve deficits can lead to significant functional impairment. Less impairing is the numbness of the axilla and dorsomedial aspect of the upper arm after sacrificing the intercostobrachial nerve. After a supraclavicular approach, injury to the supraclavicular nerves causes a sensible loss of the skin around the clavicle, anteromedial area of the shoulder and the proximal thorax.
The loose tissues in the axilla often fail to tamponade bleeding which therefore can cause significant hematoma formation. If the parietal pleura is damaged during dissection a hemothorax can develop. If there is accidental damage to the visceral pleura or lung parenchyma, a pneumothorax can occur and in these cases a standard wound suction drain is insufficient. Postoperative pain can be significant and adequate pain relief is important. An effective option is a preoperatively placed scalenus nerve block. Clinical success of surgical treatment for thoracic outlet syndrome is obtained in the majority of patients with vascular forms of TOS, with 90% of patients that report improvement of symptoms (1,2). For NTOS results are slightly worse with 60%–80% of patients reporting improvement of symptoms after surgery (1). This difference is in part explained by the lack of a reliable diagnostic modality to confirm the diagnosis of NTOS. Complication rates described in the literature vary between 5%–40%, with pneumothorax, nerve injury and wound infection as the most commonly occurring complications. Severe complications and death are extremely rare and therefore surgical treatment for TOS seems safe (1,2).
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editors (Marco Scarci, Alan D.L. Sihoe and Benedetta Bedetti) for the series “Open Thoracic Surgery” published in Shanghai Chest. The article has undergone external peer review.
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/shc.2017.05.03). The series “Open Thoracic Surgery” was commissioned by the editorial office without any funding or sponsorship. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Peek J, Vos CG, Ünlü Ç, et al. Outcome of Surgical Treatment for Thoracic Outlet Syndrome: Systematic Review and Meta-Analysis. Ann Vasc Surg 2017;40:303-26. [Crossref] [PubMed]
- Povlsen B, Hansson T, Povlsen SD. Treatment for thoracic outlet syndrome. Cochrane Database Syst Rev 2014;CD007218 [PubMed]
- Roos DB. Transaxillary approach for first rib resection to relieve thoracic outlet syndrome. Ann Surg 1966;163:354-8. [Crossref] [PubMed]
- Mackinnon S, Patterson GA, Colbert SH. Supraclavicular approach to first rib resection for thoracic outlet syndrome. Oper Tech Thorac Cardiovasc Surg 2005;10:318-28. [Crossref]
- Molina JE. Surgery for effort thrombosis of the subclavian vein. J Thorac Cardiovasc Surg 1992;103:341-6. [PubMed]
Cite this article as: Vos CG, Ünlü Ç, Voûte MT, van de Mortel RHW, de Vries JPPM. Thoracic outlet syndrome: first rib resection. Shanghai Chest 2017;1:3.