
A guide to open surgical tracheostomy
Introduction
Tracheostomy is recognised to be one of the oldest surgical procedures and references to the creation of a surgical airway in the neck can be dated back to 3600BC with pictures being depicted on Egyptian artisanry. Chevalier Jackson established the principals of the tracheostomy operation in the beginning of the twentieth century and these have grossly remained unchanged till present date (1). The term tracheostomy refers to the creation of a stoma at the skin surface leading to the trachea whereas a tracheotomy refers to the proper surgical opening in the trachea. A surgical tracheostomy can be performed under local or general anaesthesia, the scenario can be either elective or emergency setting and it can be either temporary or permanent in nature. There are multiple indications for such procedure. Upper airway obstruction can be caused by a multitude of processes including neurological, neoplastic, infective or inflammatory causes. A tracheostomy can be used to bypass the level of obstruction. In cases of prolonged mechanical ventilation, a tracheostomy replaces the endotracheal intubation to wean off anaesthetised patients, decrease the rate of subglottic stenosis, decrease the dead space and work of breathing and providing better control on secretions of the lower respiratory tract (2). A tracheostomy may also be performed as part of another surgical procedure, mostly for airway protection. An ‘end’ tracheostomy may be formed in associations with certain procedures such as a laryngectomy. Other variants of the classical surgical tracheostomy are the minitracheostomy insertion through the cricothyroid membrane and the percutaneous tracheostomy technique where the trachea is punctured from the anterior neck and the tract is serially dilated until the insertion of a standard tracheostomy tube is enabled (1,2). The latter may or may not be performed under direct vision using flexible endoscopy. A combination of such techniques may also be useful in certain selected cases.
In the elective setting, it is essential to obtain adequate consent prior to performing a tracheostomy. It is important for the patient to understand the rationale behind the decision and to understand that postoperatively there will be a variable period of communication difficulty due to lack of vocalisation. The patient should also be informed about the various complications that may arise and that a tracheostomy could end up being a permanent solution. It is imperative for the surgeon to check the relevant preoperative investigations with special reference to coagulation studies. One should consider positioning issues in the planning phase. Making sure the patient does not have an unstable cervical spine is a must as this would preclude neck extension. Children should not be hyperextended due to the higher risk of damage to the thoracic inlet vessels. A good practice in the intensive care setting is to check the endotracheal tube positioning on the latest chest X-ray. In case the patient presents with difficult anatomy such as tracheal deviation due to neck masses or a suspicion of abnormal major vessel passage or ectasia in the neck arises, the surgeon should ask for additional radiological investigations and decide regarding where is the optimum location to perform the procedure. Preoperatively, the surgeon should have familiarised himself with the selection of tracheostomy tubes available and decided which one to use according to the indication. A tube of a size above and a size below the one chosen should be readily available. Occasionally special tubes with extra length or reinforcement may be needed and a tracheostomy procedure should not be started until these are available.
Operative technique
Preparation and exposition
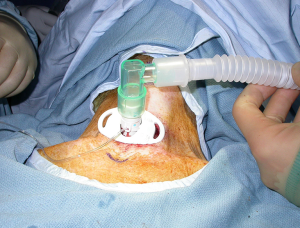
The procedure should, whenever possible, be carried out in an operating theatre with adequate lighting and stocked with a large selection of tracheostomy tubes. The patient should be placed in supine position. The neck is to be fully extended by placing a shoulder roll underneath the upper back area and the head is stabilised on a head ring. The shoulders should be at symmetrical level so the midline neck structures are not skewed to one side. Local antiseptic solution is applied and sterile conditions should be maintained throughout the procedure. Intravenous antibiotics are given according to hospital protocols. Key landmarks are marked on the skin and the incision site is placed halfway between the lower border of the cricoid and the suprasternal notch. This is then infiltrated with 5 to 10 mL of 0.25% bupivacaine solution mixed with 1:200,000 adrenaline. The chosen tracheostomy tube should be available on the operating trolley and checked by one of the surgical team for any cuff leaks (Figure 1).

Operation
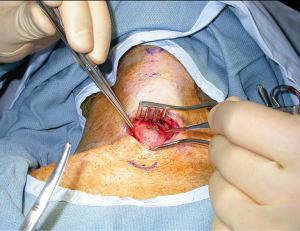
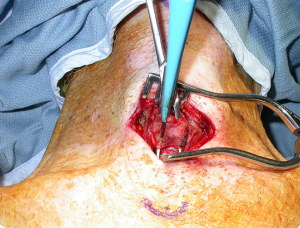
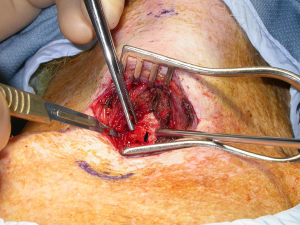
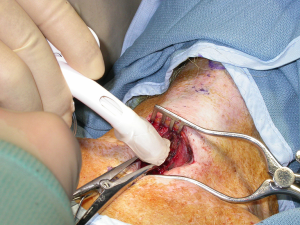
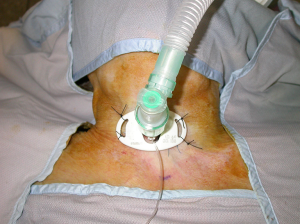
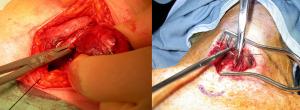
This description applies to adults having a tracheostomy under general anaesthesia. A transverse incision through skin is made half way between the inferior border of the cricoid cartilage and the sternal notch. The size is usually 3 cm but may be extended as necessary if adverse anatomical conditions are encountered. Once skin has been incised, dissection continues through subcutaneous fat. Thinned platysma fibers and the superficial investing layer of deep cervical fascia are entered and strap muscles are identified. A self-retaining retractor will be helpful at this point. Blunt dissection in the midline through the linea alba is carried out and the strap muscles are retracted laterally using Langenbeck retractors. The thyroid isthmus comes into view and this can have a variable position and size. It is skeletonised and can be divided either using clamps and transfixion sutures or using monopolar or bipolar diathermy. The anterior tracheal wall is identified and cleaned. It is useful to identify the cricoid cartilage so to be able to assess the entry point for the tracheotomy. Larger retractors are used to clear the tissues laterally so to ensure adequate exposure. The tracheotomy is usually carried out in the 3rd or 4th tracheal rings and the area is marked with bipolar diathermy. Tracheostomy tube check is reconfirmed and sterile connecting equipment should be available. The anaesthetist is alerted and a square tracheal window is created, being as conservative as possible. Careful incision of the membranous tissue between the rings is carried out with the aim not to rupture the endotracheal tube cuff. Generous suction of any secretions is ensured. A blunt cricoid hook is inserted at the top of the tracheotomy and gentle superior retraction is applied. The anaesthetist should be instructed to withdraw the tube under the direction of the surgeon. When the tip is immediately above the tracheotomy, the withdrawal is stopped and the tracheostomy tube is inserted from one of the sides and gently rotated in place. The tracheostomy cuff is then inflated and the position is checked by confirming bilateral chest expansion and carbon dioxide trace uptake on the anaesthetic machine. Only then the cricoid hook is removed from the tracheotomy. The incision is closed loosely and the tracheostomy tube is secured in position with sutures and ties or Velcro tapes. Tracheostomy dressing is finally applied (Figures 2-12).




Completion
One of the first things to check for, in the immediate postoperative period, is the presence of bleeding for the tracheostomy site. The tracheostomy site is also checked for audible air leak, in which case further air is inflated in the tracheostomy cuff. The neck is palpated for surgical emphysema to check if the skin sutures have been placed too tight around the tracheostomy tube. On the other-hand, if too loose, there may be fluid leaks and subsequent infections. A chest X-ray should be ordered to exclude any lung complications such as pneumothorax. The patient is usually nursed in a reverse trendelenburg position and it is ensured that the tracheostomy tube is not pulled laterally by the ventilator tubing system. The various components of the tracheostomy tube kit that are not being used by the patient, such as insertion trocars and spare inner tubes, should be sealed in a bag and given during a proper handover to the nursing staff taking care of the patient. These nurses should be experienced in the care of tracheostomy patients and knowledgeable about the potential complications (3). It is ensured that appropriate humidification and nebulisers are given and regular suctioning is administered. Instructions to deflate the cuff should be given only once the risk of aspiration passes.
Comments
Although there are many variations in performing a classical open surgical tracheostomy, these are all based on a standard technique composed of few fundamental steps. It is a safe procedure in experienced hands or where there is adequate supervision. It can also be associated with significant morbidity and mortality if not performed in a logical systematic way, especially when patients present with abnormal features.
Tips and tricks
A large neck always presents a challenging case for tracheostomy insertion. One should maximise the exposure by doing a generous incision. An extra assistant is usually very useful to help in retraction. It is obligatory to have adequate lighting. One should not rush and all the necessary time is taken to identify anatomy systematically. Subcutaneous and peri-thyroid fat can be removed if necessary. Adequate tracheostomy tubes should be available, preferably those with an adjustable flange. In the postoperative period, it would be worthwhile to do the first tube change over a guide-wire as in a deep neck the formation of the tracheostomy tract is delayed and there is the higher risk of false passage formation.
Incisions can be wrongly placed, either too high or too low. This can make it difficult to identify the key anatomical structures and make proper placement of the tracheotomy window challenging. The thyroid isthmus should always be dealt with and ensured that there is no bleeding afterwards. When the isthmus is large, one should perform an isthmusectomy and send this excised part for histological analysis. Otherwise one can consider suturing the divided isthmus to the strap muscles so it does not fall in the way and does not occlude the tracheotomy window.
The tracheotomy can be performed in a number of ways, including horizontal incisions, vertical incisions, various shapes of window excisions and the usage of a Bjork flap. If it is done too high there is a significant risk of subglottic stenosis formation; if done too low it will make tube change very challenging. The same happens if the window is made too small, whereas if made too large there can be a significant leak and a higher risk of tube dislodgement. Roughened edges of the tracheotomy have a higher tendency for persistent bleeding. The Bjork flap technique is a double-edged sword as it can make tube change more easy but is technically more difficult and may cause airway obstruction if incorrectly performed and difficult closure of the tracheostomy if the patient is decannulated (1). Whatever technique is used, one has to perform this step in a systematic manner to ensure the best outcome for the patient.
The tracheostomy tube choice should to be correct on the first attempt. In the stage of forming a new fresh tracheostomy, the tube has to be cuffed to protect the patient’s airway and provide a seal for ventilation. We prefer to use double lumen tubes as they are easier to take care of on the wards and pose less problems with blockage. If the patient is going to restart using his voice in the postoperative period, it would be worthwhile to insert a fenestrated tube and use a non-fenestrated inner tube until necessary. The right insertion technique is of paramount importance as one can easily create a false passage and end up with airway obstruction either during the procedure or worse later on in the postoperative period. Whatever tube is used, this must be secured in multiple ways so to prevent dislodgement or false tract formation (3).
Caveats
Intraoperative complications may result when the surgeon deviates from working in the midline. This can result in damage to the contents of the carotid sheath, perforation of the oesophagus and damage to the recurrent laryngeal nerves. The safest way to avoid these complications is to identify key anatomical structures in a stepwise manner, have adequate exposure and haemostasis. The position of the cricoid and other key structures should be checked frequently by digital manipulation. If the cricoid cartilage is inadvertently damaged, the tracheotomy should be sited lower and the damage repaired. The most common source of bleeding is the thyroid isthmus and the inferior thyroid veins. There should be a low threshold for re-exploration of the tracheostomy wound if bleeding persists (4). Air embolism resulting from open large inferior thyroid veins is extremely rare and should be prevented by adequate ligation of such vessels. Superior mediastinal vessels may be pulled above the suprasternal notch whereas pleurae may be in a higher position in patients with emphysema and other chronic obstructive lung pathology. Careful dissection prevents such injuries.
An early postoperative complication may be accidental extubation (3). If there is a suspicion one should confirm the tube position by passing a flexible endoscope down the tube. If it is displaced one should replace the tube or change it to a longer one, preferably in a safe environment with adequate instrumentation. Tube blockage by crusting or dried blood may occur and should be prevented by regular suctioning. Local infection may be prevented by meticulous surgical technique and proper placement of the tube together with administration of antibiotics according to the local hospital policy. Tracheoesophageal fistulae may develop due to persistent pressure from a tracheostomy tube on the posterior wall of the trachea. Recurrent aspirations despite the tube cuff being inflated would be a sign for this. If the tube position is pushing excessively anteriorly, one may run the risk of causing a fistula between the trachea and the innominate artery especially if it is running an anomalous high passage. It may be rarely heralded by sentinel bleeds but usually presents with massive uncontrollable haemorrhage (4). Tracheal stenosis, tracheomalacia and a persistent tracheocutaneous fistula are late complications that may need surgical intervention to be managed.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editors (Marco Scarci, Alan D.L. Sihoe and Benedetta Bedetti) for the series “Open Thoracic Surgery” published in Shanghai Chest. The article has undergone external peer review.
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/shc.2017.05.05). The series “Open Thoracic Surgery” was commissioned by the editorial office without any funding or sponsorship. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Pracy JP, Rogers M. Tracheostomy. In: Watkinson J, Gilbert RW. eds. Stell & Maran's textbook of head and neck surgery and oncology. CRC Press, 2012:273-280.
- Cheung NH, Napolitano LM. Tracheostomy: epidemiology, indications, timing, technique, and outcomes. Respir Care 2014;59:895-915; discussion 916-9. [Crossref] [PubMed]
- McGrath BA, Bates L, Atkinson D, et al. Multidisciplinary guidelines for the management of tracheostomy and laryngectomy airway emergencies. Anaesthesia 2012;67:1025-41. [Crossref] [PubMed]
- Bradley PJ. Bleeding around a tracheostomy wound: what to consider and what to do? J Laryngol Otol 2009;123:952-6. [Crossref] [PubMed]
Cite this article as: Muscat K, Bille A, Simo R. A guide to open surgical tracheostomy. Shanghai Chest 2017;1:4.


