Rib fracture repair
Introduction
Blunt chest wall trauma and the resultant fracture of ribs is exceedingly common and is the source of significant morbidity and potential mortality. Surgical repair for markedly displaced rib fractures, particularly in the setting of flail chest has been attempted sporadically for over 50 years. In the last decade, rib-specific plating systems have been introduced. These have helped to usher in the era of modern rib repair and have made surgical stabilization of rib fractures (SSRF) technically easier, safer, and arguably more effective. In the United States, the procedure is increasingly utilized by trauma, orthopedic, and thoracic surgeons.
Two recently published consensus statements have attempted to codify the indications, contra-indications, timing, and technical aspects of SSRF (1,2). In brief, patients with three or more severely displaced rib fractures or flail chest (two or more contiguous ribs fractured in two or more places) should be considered for repair whether they require mechanical ventilation or not. Other candidates may include patients who fail optimal non-operative management regardless of fracture pattern, and patients with rib fractures who require thoracotomy for another reason. Severe traumatic brain injury and unstable spine fracture are absolute contraindications to immediate SSRF. The role of pulmonary contusion in the decision to repair the unstable chest wall remains controversial, but in general is not a contraindication.
Operative techniques
Preparation
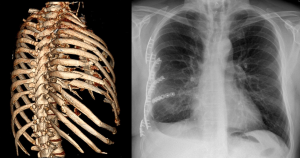
Once the trauma patient has been satisfactorily resuscitated, hemodynamic stability has been achieved, and a thorough evaluation of all injuries completed, a decision to proceed with operative fixation of rib fractures can be made. Three-dimensional reformatted images of the chest CT scan (Figure 1), while not mandatory, are extremely helpful in delineating the true extent of fractures, chest wall deformity/instability, and in incision planning. Pre-operative patient optimization must include aggressive multi-modal pain control, pulmonary hygiene, and an assessment of pulmonary function, i.e., spirometry. Pre-operative bronchoscopy can clear bronchial secretions and blood, and assist in placement of a double-lumen endotracheal tube, if necessary. Many surgeons utilize VATS routinely (3). These authors do so selectively to assist in evacuation of hemothorax, localize fractures, and to rule-out diaphragm laceration.
Operation
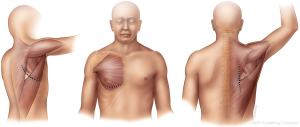
Lateral decubitus positioning provides access to the majority of rib fractures. Supine position with a bump will provide ideal exposure for anterior and antero-lateral fractures. Many patients will have multiple fracture lines and may benefit from dual incisions. Prone positioning with 90-degree abduction of the ipsilateral arm will rotate the scapula laterally and optimize exposure to posterior and subscapular fractures (Figure 2).
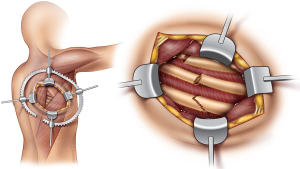
Proper placement of the surgical incision(s) should minimize incision length and soft–tissue trauma. We have increasingly adopted non-traditional incisions, such as oblique or vertical, and avoid muscle transection whenever feasible. “Splitting” (without dividing) the latissimus dorsi is routine and provides excellent exposure to most lateral and posterior fractures. The triangle of auscultation affords the surgeon reliable access to the subscapular space (Figure 3).
Following skin incision, sub-cutaneous flap development will allow access to multiple fractures through the same incision. Fractures are generally easily palpable through the musculature and should be exposed individually. Self-retaining retractors such as the Bookwalter or Thompson type retractor can aid in this exposure. Fracture reduction is usually quite simply accomplished with lifting of the depressed rib segment with a right-angle clamp or finger and the fracture ends can be “perched” in proper reduction. Reduction of multiple adjacent fractures in sequence prior to fixation will help maintain chest wall contour and aid in hardware placement.
Clearing the rib of its anterior soft tissue envelope is necessary for 3 centimeters on either side of the fracture to facilitate precise matching of rib prosthesis to the rib surface. Aggressive exposure of the fractured rib ends is unnecessary and undesirable.
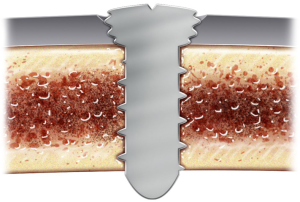
Several rib-specific plating systems are now commercially available. They share multiple design features; notably, semi-rigid fixation with anterior plate positioning and locking screws. The flexible nature of ribs makes locking screws critical to minimize failure. Additionally, these systems are low profile, made from titanium, and easily shapeable (Figure 4).
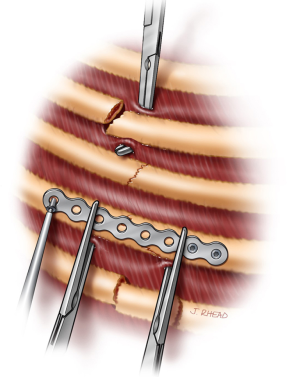
Rib thickness is variable. Thus, prior to plating, in most systems, rib thickness is measured with a caliper to determine optimal screw length. Bi-cortical screw purchase of the rib is considered the standard at this time, but one commercially-available system utilizes shorter uni-cortical screws with non-parallel orientation. The surgeon will assess the obliqueness of the fracture line to determine how many screw holes to leave open in the middle of the plate. One should strive for a minimum of 3 cm of plate fixation on each side of the fracture (Figure 5). The plate should be shaped to the precise contour of the anterior rib surface with no gaps and with minimal tension. Plate holding forceps or right angle clamps will hold the plate in position and the rib in reduction for screw placement. Current systems utilize either pre-drilling or self-tapping screws.
Ribs have complex shapes and precise matching of plates to ribs will often require bending and twisting in two or more planes. All of the available systems have “low profile” or right angled drill and screwdriver instruments to accommodate fixation at the extremes of exposure, i.e. underneath the scapula or close to the spine.
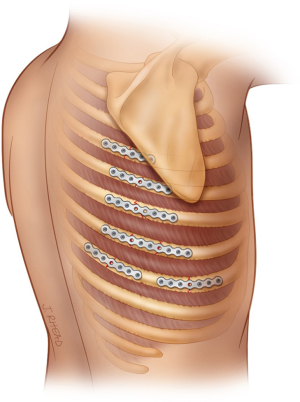
It is unnecessary to repair every broken rib. In general, ribs 1,2,11, and 12 should be avoided. Chest wall stability increases with each rib stabilized and it is reasonable to fix all rib fractures that are readily approachable through the index incision. One should make a concerted attempt to repair both fracture lines in the setting of flail (Figure 6).
Completion
Closure is made easier with muscle sparing approaches. Absorbable sutures in a running or interrupted fashion, are used to close muscular “windows”. The decision to place a closed suction drain in the sub-cutaneous space is based on host factors and surgeon preference. Chest tube placement is optional but strongly suggested by these authors. We utilize soft, fluted tubes of 24Fr diameter. This is an excellent opportunity to lavage the pleural space with 1 or 2 liters of warm saline. These authors use this blind lavage technique and have had excellent results with minimal incidence of retained hemothorax (4). Placement of a regional analgesia catheter or intercostal rib blocks complete the procedure (Figure 7).
Comments
Rib fracture repair, like any other procedure, has a definite learning curve. Those new to SSRF should select patients with lateral fracture patterns, avoiding the more difficult fractures at the extremes of exposure. Length of incision will naturally diminish as one gains experience and confidence in adequate exposure and reduction of fractures. Most rib repairs in the US are performed by trauma or thoracic surgeons, although this varies from center to center. Surgeons new to the principles of osteosynthesis may wish to enlist the help of an orthopedist colleague as they navigate their early experience.
Acknowledgments
We would like to thank Jill Rhead as our talented and generous Medical Illustrator for the chapter.
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editors (Marco Scarci, Alan D.L. Sihoe and Benedetta Bedetti) for the series “Open Thoracic Surgery” published in Shanghai Chest. The article has undergone external peer review.
Conflicts of Interest: Both authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/shc.2017.05.07). The series “Open Thoracic Surgery” was commissioned by the editorial office without any funding or sponsorship. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Pieracci FM, Majercik S, Ali-Osman F, et al. Consensus statement: Surgical stabilization of rib fractures rib fracture colloquium clinical practice guidelines. Injury 2017;48:307-21. [Crossref] [PubMed]
- Kasotakis G, Hasenboehler EA, Streib EW, et al. Operative fixation of rib fractures after blunt trauma: A practice management guideline from the Eastern Association for the Surgery of Trauma. J Trauma Acute Care Surg 2017;82:618-26. [Crossref] [PubMed]
- Pieracci FM, Lin Y, Rodil M, et al. A prospective, controlled clinical evaluation of surgical stabilization of severe rib fractures. J Trauma Acute Care Surg 2016;80:187-94. [Crossref] [PubMed]
- Majercik S, Vijayakumar S, Olsen G, et al. Surgical stabilization of severe rib fractures decreases incidence of retained hemothorax and empyema. Am J Surg 2015;210:1112-6; discussion 1116-7. [Crossref] [PubMed]
Cite this article as: White TW, Majercik S. Rib fracture repair. Shanghai Chest 2017;1:11.