Resection of superior sulcus cancers (anterior approach)
Introduction
Tumors of superior sulcus are defined as primary lung cancers involving one or more structures of the apex of the thoracic cavity. They are frequently referred in the eponymous of Pancoast HK who described in 1932 the clinical and radiological findings associated with tumors arising in the region. Invasion of one or more of the following structures is frequent: lower roots of brachial plexus, stellate ganglion and sympathetic trunk, upper thoracic ribs or vertebrae, subclavian vessels. Since the work of Tobias J. W. the constellation of symptoms related to these tumors is also referred as the Pancoast-Tobias syndrome.
Up to Fifties these tumors deemed as inoperable, but thanks to the work of Shaw R. R. irradiation followed by resection became the standard treatment for a long while, whereas multimodality approach including radiotherapy, surgery and chemotherapy, pre and/or post-operatively has been variously explored in recent years (1).
Surgical access to apical tumors has been classically achieved in the rules of Paulson D. L. and Shaw R. R. through a posterior thoracic incision (1). This access is fully satisfactory when dealing with posteriorly located tumors, but may be inadequate in the presence of involvement of anterior structures. For this reason, several anterior approaches have been developed, including the cervico-sterno-thoracotomy, the hemiclamshell, and the transcervical-transthoracic approach with resection of the clavicle.
During last twenty years, however, the transmanubrial approach (2), which will be described in details in the present chapter, has gain large favor as the first-choice approach for anterior forms of the superior sulcus tumors. In our opinion (3), main indications for an anterior approach are represented by proven or suspected infiltration of cervico-mediastinal vascular structures or infiltration of anterior arch of first/second ribs. More infrequent indications include: presence of a palpable supraclavicular mass, clinical involvement of C7 and/or C8 root, Horner syndrome. In these last three cases, first-line surgery is rarely indicated and patient is generally operated after induction.
Operative techniques
Single lung ventilation is mandatory for this operation, especially if lung resection is performed through the anterior approach. Thus, general anesthesia and double-lumen intubation are necessary. For anterior approach, supine position is adopted, with patient positioned on the operative table with the arms are abducted at 90° and the neck hyperextended with the head turned toward non-operated side to expose the homolateral sterno-cleido-mastoid region and the sternal notch. We use to put a vertical roll under the spine to allow shoulder gentle fall of the shoulder of the operated side. The whole homolateral neck and thorax are included in the operative field and skin preparation and draping is extended some centimeters away from the midline.
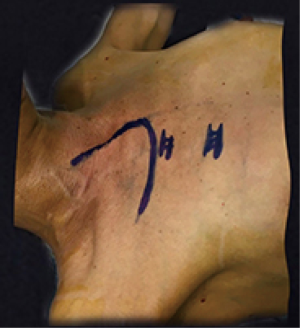
The skin incision includes a vertical presternocleidomastoid incision which is prolonged over the upper the sternal manubrium and then horizontally two transverse fingers below the clavicle up to the delto-pectoral groove (Figure 1).
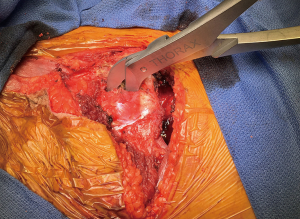
The anterior margin of the sternomastoid muscle is freed and the lower portion of the internal jugular vein is dissected, manubrium and upper portion of the second rib are exposed. The first intercostal space is opened, thus allowing finger exploration of the pleural cavity and anticipation of further technical aspects of the operation (Figure 2).
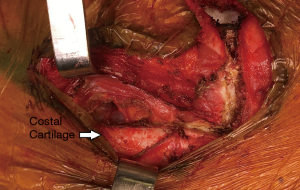
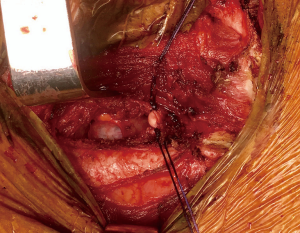
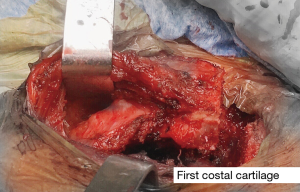
Internal thoracic vessels are subsequently dissected and sectioned at the first intercostal space level (Figure 3). This allows exposition of the lateral aspect of the sternal manubrium which can be now sectioned by an oscillating saw in an L-shaped (dextro or laevorotatory) fashion: midline vertical, and horizontal from the lateral aspect to the midline (Figure 4). This allows preservation of the sterno-clavicular joint. The sternoclavicular flap may be elevated only after division of the first rib cartilage at its sternal insertion and provided that no tumour invasion is present at this level (Figure 5). The upper portion of the major pectoral muscle is now elevated to expose the cartilage of the first rib that could be sectioned with a costotome (Figure 6) , a hand manoeuvred (Gigli), or an electrical saw ( Figure 7) .


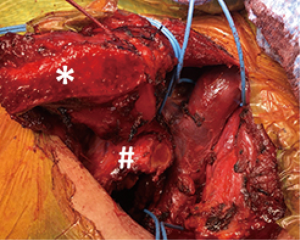
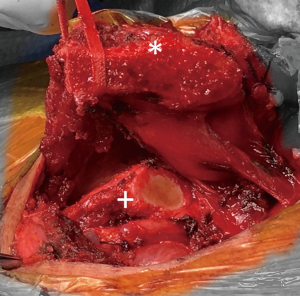
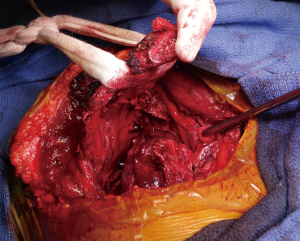
In parallel with flap elevation, section of the costo-clavicular ligament is carried out (Figure 8), thus providing increasing amplitude to the operative field (Figure 9). Exposure of the whole cervico-thoracic junction is now achieved. Further dissection depends on the extent of tumours and infiltration of different structures: upper ribs, especially in their anterior portion, subclavian vessels, apical pleura, sympathetic chain, and/or brachial plexus. The section of the internal jugular vein may be seldom necessary in order to allow a better access to posterior plans. Subclavian vein is dissected and spared if free, or easily resected without need of subsequent revascularization (contralateral venous axis can be preserved in almost all the instances). Dissection of the subclavian vein encompasses the visualization of the phrenic nerve which in cervical region lies anteriorly to anterior scalene muscle and behind the subclavian vein, whereas in its thoracic portion is placed on the antero-lateral aspect of the venous axis.

Thus anterior scalene muscle can be safely freed from its insertion on the first rib tubercle, allowing exposition of the subclavian artery. Sacrifice of its branches may be required and care should be taken to spare, if possible, the vertebral artery. In case of tumors infiltrating the wall of the artery a dissection in the subadventitial plane should be attempted and is generally successful; deeper infiltration requires resection and reconstruction. End to end anastomosis or interposition of a (6-8 mm in diameter) polytetrafluoroethylene graft can be performed, depending on the extent of resection. Behind the arterial plane, vertebral bodies and the nerves root coming from the intervertebral foramina are accessible. Of note anteriorly to nerve roots of brachial plexus lay the stellate ganglion and sympathetic chain.
In case of tumours invading the chest wall en bloc resection is to be planned. As previously described (Figure 2) the invasion of the parietal wall is first explored when performing the thoracotomy at the first intercostal space. In case of involvement of first intercostal space or of the second rib a lower anterior thoracotomy at the second or third intercostal space must be performed. Once L-shaped section of the manubrium is performed the inspection of its posterior aspect is performed and especially of the cartilage of the first rib which is sectioned to finally elevate the osteomuscolar flap. Posterior control of the parietal wall infiltration through the anterior approach is possible for the first rib. When parietal involvement concerns the ribs posteriorly, below the second or the third one, the transmanubrial approach is carried out as described, and posterior rib resection is performed through an associated posterior approach. After dissection and/or resection of chest wall and remaining structures of cervico-thoracic junction (apical pleura, sympathetic chain, brachial plexus), the osteomuscular flap is returned in its position, sternal manubrium is sutured by two metallic stitches and soft tissues are closed as usually. Motility of shoulder is thus completely preserved.
Comments
In case of surgery for primary lung cancer lobectomy should constitute the standard pulmonary resection and it has to be associated to mediastinal lymph nodes dissection. Obviously the access to the hilar pulmonary structures is restraint through the thoracic inlet even in case of a wide elevation of the manubrium-clavicular flap. Unless in some cases (thin patients with limited tumours not involving hilar structures nor posterior chest wall) lobectomy can be carried out through the anterior approach, in the most cases, after completion of the surgical manoeuvres through the anterior approach, the patient should be turned in the full lateral position to perform a second incision, generally a postero-lateral thoracotomy, which allows standard lung resection, mediastinal lymph nodes dissection and eventually the completion of posterior chest wall resection. In order to avoid a second installation and a second incision, the use of a “modified hemi-clamshell” approach can be planned. In this technique a standard hemiclamshell approach in the third or fourth intercostal space is associated to the section of the first cartilage and opening of the costoclavicular ligament (7). Thanks to the lower anterior thoracotomy and to the possibility to rotate the osteomuscolar flap, a full mediastinal vascular control is possible, as well as an easy access to the structure of the pulmonary hilum (Figure 10).
Our experience on surgical management of superior sulcus tumor has been previously reported (3). We employed an isolated posterior approach in 49% of cases, whereas in the remaining patients (with the exception of a single case who had an isolated anterior approach) a combined anterior and posterior approach was carried out. Complete resection was achieved in 82% of cases. Operative mortality was 8.9%. This percentage is relatively high but probably explained by the extent of resection in a subset of lung cancer patients presenting frequently important associated illness. Overall survival rates (including non-cancer-related deaths) were 54% and 36.2 at 2 and 5 years, respectively. Study of prognostic factors showed, at multivariate analysis, that T status, R0 resection, and the presence of associated comorbidities, were independent prognostic factors. Patients with T3N0 tumors experienced a 5-year survival as high as 47.7%.
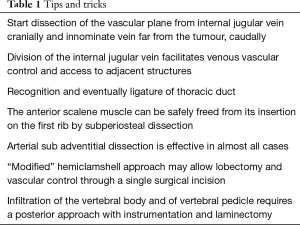
Surgery of the thoracic inlet is challenging because of the presence of several leading vascular and nervous structures, in any case a precise knowledge of the anatomy of the first rib is crucial. A list of tips and trick is in Table 1. After elevation of the osteomuscular flap, the mediastinal venous net is first encountered (Figure 11). A smart tip is to not hesitate to divide the internal jugular vein which facilitates mobilization of the innominate vein and raises visualization of the surrounding structures. It should be noted that right or left interruption of the innominate vein can be performed without the need of vascular continuity reconstruction, unless the occurrence of a temporary (1-2 months) arm oedema in the postoperative period. During the dissection of the venous axis, we recommend the recognition of the lymphatic thoracic duct on the left side but also detection of either a right-sided thoracic duct, or the right cervico-thoracic lymphatic duct (Figure 12), in order to avoid post-operative leaks. It should be reminded that the phrenic nerve originates from the 4th cervical nerve and receives contributions from the 5th and 3rd cervical nerves (C3-C5). In the cervical region the nerve lies behind the venous axis in front of the anterior scalene muscle. The anterior scalene muscle can be safely freed from its insertion on the first rib by subperiosteal dissection, if not directly infiltrated by the tumor allowing extrathoracic control of the subclavian artery.
Full table
In case of arterial infiltration proximal and distal control of subclavian artery is performed, and, in this objective, ligature of one or several of its branches (vertebral artery, internal thoracic artery, thyreocervical artery, costocervical trunk, dorsal scapular artery) may be necessary. We generally attempt dissection of subclavian artery itself in the sub-adventitial plane and this maneuver is often successful; otherwise resection and reconstruction is performed by end to end anastomosis or by prosthesis interposition.
In case of tumors infiltrating the posterior mediastinum, the dorsal sympathetic chain and the stellate ganglion can be involved as well as the lower nerve root of the brachial plexus. These structures can be resected by the anterior approach. This is generally done after dissection of the vascular structures. In case of deeper infiltration involving the spine, anterior approach is in most cases unsatisfactory and a second step by posterior approach is generally necessary. Infiltration of prevertebral fascia may be resected by the anterior approach as well as limited infiltration of the periosteum of vertebral body, but more extensive infiltration of the vertebral body and, a fortiori, of vertebral pedicle requires a posterior approach with instrumentation and laminectomy. In these cases after a dissection as complete as possible, the anterior approach is closed, the patient repositioned either in Paulson or ventral decubitus (according to the team experience) and the operation continued by the posterior approach allowing en –bloc vertebral resection.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Shaw RR, Paulson DL, Lee JL. Treatment of Superior Sulcus Tumor by Irradiation Followed by Resection. Ann Surg 1961;154:29-40. [Crossref] [PubMed]
- Grunenwald D, Spaggiari L. Transmanubrial osteomuscular sparing approach for apical chest tumors. Ann Thorac Surg 1997;63:563-6. [Crossref] [PubMed]
- Alifano M, D'Aiuto M, Magdeleinat P, et al. Surgical treatment of superior sulcus tumors: results and prognostic factors. Chest 2003;124:996-1003. [Crossref] [PubMed]
- Bobbio A, Strano S, Alifano M. Division of the sternal manubrium. Asvide 2017;4:250. Available online: http://www.asvide.com/articles/1559
- Bobbio A, Strano S, Alifano M. Division of the first cartilage with electric saw. Asvide 2017;4:251. Available online: http://www.asvide.com/articles/1560
- Bobbio A, Strano S, Alifano M. Division of the costoclavicular ligament. Asvide 2017;4:252. Available online: http://www.asvide.com/articles/1561
- Rusca M, Carbognani P, Bobbio P. The modified “hemi-clamshell” approach for tumors of the cervicothoracic junction. Ann Thorac Surg 2000;69:1961-3. [Crossref] [PubMed]
Cite this article as: Bobbio A, Strano S, Alifano M. Resection of superior sulcus cancers (anterior approach). Shanghai Chest 2017;1:12.