Carinal resection
Introduction
Carinal resection is a challenging procedure that is rarely performed and which requires both strict attention to technical details and good patient selection. Most patients who undergo carinal resection have lung or airway cancer; squamous cell carcinoma, carcinoids, and adenoid cystic carcinoma are the most frequent. However, less often, it can also be indicated in benign cases as tuberculosis associated strictures or post-pneumonectomy fistula.
Patient selection is critical; therefore, in patients with lung cancer thorough staging is mandatory, since patients with N2 disease usually have a dismal prognosis. Since carinal resection is a major thoracic procedure, pre-operative functional evaluation is also very important to select the candidates adequately. All cases should undergo detailed anatomic assessment including imaging and bronchoscopy. Such exams will help to define the access route, the extension of the resection, and the need for associated procedures (1,2).
Operative technique
The carina may be accessed by right thoracotomy or median sternotomy. Carinal resection through left thoracotomy, even though feasible, is difficult and implies extensive mobilization of the aortic arch (2,3).
Tumors that involve the carina but do not require lung resection might be approached either by right thoracotomy or by sternotomy. Tumors that extend more distally in the left main stem bronchus are more easily approached through median sternotomy since this route allows both reimplantation of the right bronchus in the trachea and resection of the left lung. When resection of the right lung or of the right upper lobe is anticipated, the better access is through a right thoracotomy (1).
Preparation
With the patient in the OR, it is advisable to perform a bronchoscopy in order to confirm the extension of the resection and the planned reconstruction.
Anesthesia for patients undergoing carinal resection can be very challenging due to ventilation issues. There are three options for intra-operative ventilation support: jet-ventilation, intermittent cross-field ventilation, or in selected cases veno-venous extracorporeal membrane oxygenation (ECMO). Close cooperation with the anesthesia team is extremely important for a successful procedure (1,2).
As for patient positioning, patients undergoing median sternotomy should be in dorsal decubitus with a small cushion placed horizontally in the scapular region to elevate the sternum. Patients undergoing right thoracotomy should be in left lateral decubitus with an axilar cushion and a pillow between the legs. We prefer to use a support to hold the right arm.
Exposition
The access to the carina varies according to the access route chosen, sternotomy or right thoracotomy.
Sternotomy
After preparation, a skin incision is made in the anterior chest midline extending from the sternal notch to the xiphoid process. Then, the subcutaneous tissue is incised until the anterior sternal periosteum. The interclavicular ligament is cut and the periosteum divided and cauterized. Following this, the sternum is separated in the midline with a pneumatic sternal saw and a retractor applied to expose the mediastinal structures.
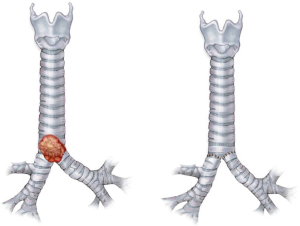
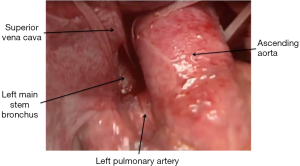
After removal of thymic and fat tissue covering the pericardium, the great vessels are exposed and the pericardium opened. Left brachiocephalic vein is encircled and retracted superiorly, superior vena cava is encircled and retracted laterally, ascending aorta is encircled and retracted laterally, and finally, left pulmonary artery encircled and retracted inferiorly. These maneuvers allow for exposure of the distal trachea and carina. The space is pretty tight with this approach and aorta retraction can be particularly challenging in older patients; these aspects should be kept in mind when selecting the access route. Another point is that, a good mobilization of the left pulmonary artery exposes the left main bronchus very well (Figure 1).
Right thoracotomy
After preparation of the patient, a muscle-sparing lateral thoracotomy is performed over the fifth intercostal space. After dividing the skin and subcutaneous tissue and retracting the latissimus dorsi and anterior serratus muscles, the fifth intercostal space should be identified and opened but with careful dissection of the intercostal muscle and its vascular pedicle since it will be used later as muscular flap to cover the airway anastomosis.
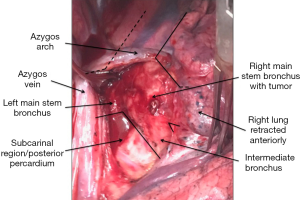
After entering the chest, it is very important to inspect and evaluate the extension of the disease particularly looking for vena cava invasion and compromise of the right lung hilar structures. The next step is to open the mediastinal pleura below the azygos arch and remove the subcarinal lymph nodes. Following this, the azygos arch is divided exposing the posterior aspect of the distal trachea and carina (Figure 2).
Operation
Release maneuvers
A very important aspect of the carinal surgery is to assure that airway reconstruction is tension-free to reduce the possibility of complications as dehiscence or stenosis. Therefore, there are some maneuvers that should be done in order to release the involved structures and facilitate the approximation of the two-ends of the anastomosis.
The most frequently used release maneuver is the development of a pretracheal plane, similarly to what is done in tracheal surgery. One must be cautious, though, in avoiding dissecting the lateral wall of the trachea to prevent devascularization. Pretracheal dissection alone provides distal mobilization of the trachea of up to 2 cm without compromising lateral blood supply and can be performed when the access route is either through thoracotomy or sternotomy (2,3).
Another release maneuver that can be used when the access route is thoracotomy is the hilar release. Significant anastomotic tension reduction can be achieved by, after division of the inferior pulmonary ligament, performing a U-shaped incision in the pericardium beneath the inferior pulmonary vein and intrapericardial division of the raphe extending from the inferior pulmonary vein to the inferior vena cava (2,3).
Carinal resection associated or not to lung resection
After carinal exposure, the trachea, the right and left main bronchus should be encircled and tapes should be placed around these structures. Gentle dissection is critical to avoid devascularization and to prevent injury to the recurrent laryngeal nerve that runs parallel to the trachea. Paratracheal lymphadenectomy should be limited.
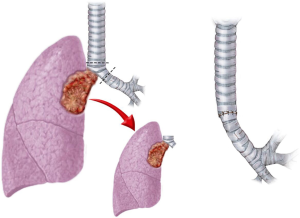
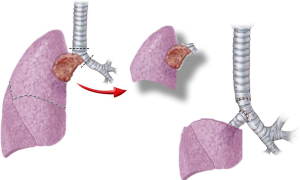
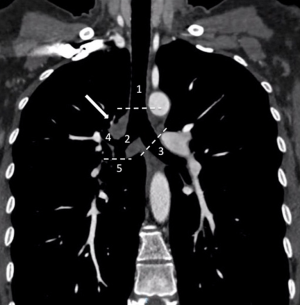
The extension of airway resection should be planned before the procedure and revised intraoperatively by the means of frozen-section analysis of the margins. Lesions restricted to the distal trachea and carina do not require lung resection and involve only the resection of the carina. Lesions extending to distal left main stem bronchus may require left pneumonectomy. Lesions extending to the right main bronchus may require upper lobectomy (when restricted to the right upper lobe and right main stem bronchus) or right pneumonectomy (when the lesion extends to the bronchus intermedius or involves more lobes) (Figure 3).
Reconstruction
After removal of the specimen, it is necessary to reconstruct the airway and the reconstruction varies a lot depending on the resection performed. Nevertheless, some basic principles should be followed in all anastomosis.
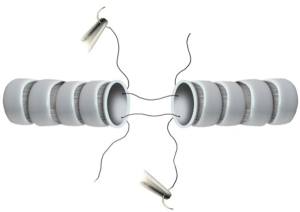
First, repair sutures (PDS 3.0) should be applied in the transition between the cartilaginous and membranous wall bilaterally. These sutures should be made so that the knot is tied in the external surface of the airway (Figure 4). Second, avoid trauma of the airway mucosa through gentle handling of the tissue. Third, perform a PDS 4.0 continuous suture approximating the cartilaginous walls of the two ends and starting from the portion deepest in the mediastinum (if the access was through a sternotomy, start with the membranous wall). The suture should involve all airway layers and be placed 3 to 4 mm from the cut edge. Size mismatch is extremely frequent and should be corrected with adequate spacing between stiches. Fourth, repeat this last step in the membranous wall (or cartilaginous wall, if membranous wall was already sutured). Fifth, approximate the two ends and tie the deeper knots. Sixth, finish the suturing of both walls and tie the knots in the more superficial extremity of the anastomosis. Finally, test for air leaks (1-3).
The peculiarities of the most frequent reconstructions are detailed below.
- “Neocarina”: patients who undergo limited resection of the carina may have their airway reconstructed by the means of a “neocarina” (Figure 5). In this technique, the right and left main bronchus are sutured together and then attached to the distal trachea. It is important to suture the medial cartilaginous wall of the two bronchi with interrupted sutured and be aware that the left main bronchus mobility is usually limited by the aortic arch; therefore, longer resections of this bronchus may preclude this type of reconstruction. The anastomosis to the distal trachea follows the principles previously enumerated (1).
- Right sleeve pneumonectomy: the most frequent situation involving carinal resection is the right sleeve pneumonectomy. In these cases, patients have large tumors involving more than one lobe, extending to the bronchus intermedius, and/or invading the pulmonary artery. The resection of the right lung altogether with the carina, makes it necessary an end-to-end anastomosis of the left main stem bronchus to the distal trachea (Figure 6) (1,2).
- Anastomosis of the carina to the left bronchus and reimplantation of the bronchus intermedius: patients in which the carina was resected altogether with right upper lobe sparing the middle and lower lobes undergo a more complicated reconstruction. In such cases there are some options, but the most popular is end-to-end anastomosis of the left main bronchus to the trachea and an end-to-side anastomosis of the intermedius bronchus to an opening in the left main bronchus (Figure 7). The end-to-end anastomosis follows the same principles previously described, but the end-to-side anastomosis has additional issues. First, the ovoid opening in the left main bronchus should be at least one cm away from the anastomosis of the trachea to reduce problems related to devascularization of the tissue. Second, the opening must performed at the medial cartilaginous wall avoiding the membranous wall to provide rigidity and avoid collapse of the anastomosis (1,2).
Completion
After completing the reconstruction, the anastomosis should be tested for air leaks and then the intercostal muscle flap prepared at the beginning of the procedure placed around the anastomosis to protect it.
A 28 Fr chest tube is placed in the mediastinum (sternotomy) or pleural space (thoracotomy) and the chest closed.
Comment
Tips, tricks and caveats
One of the most challenging issues of carinal surgery is intraoperative ventilation. Discuss the strategy thoroughly with the anesthesia team before the procedure either the option be jet ventilation, cross-field intermittent ventilation, or ECMO.
The most feared complication of carinal surgery is anastomotic dehiscence, and, in fact, mortality associated to this complication is extremely high. Besides the release maneuvers and the gentle handling of the tissues, other actions could decrease the risk of anastomotic complications. First, avoid extensive dissection of the trachea and bronchus, try not dissect more than 2 cm away from the cut edge. Second, tailor the suturing to accommodate for the ends size mismatch, avoid cutting wedges of the bronchi or trachea or using other similar strategies because they usually compromise vascularization of the anastomosis line. Finally, the length of airway resection should not exceed 4 cm, otherwise the tension will too high and increase the risk of dehiscence (3,4).
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editors (Marco Scarci, Alan D.L. Sihoe and Benedetta Bedetti) for the series “Open Thoracic Surgery” published in Shanghai Chest. The article has undergone external peer review.
Conflicts of Interest: Both authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/shc.2017.07.03). The series “Open Thoracic Surgery” was commissioned by the editorial office without any funding or sponsorship. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Gonfiotti A, Jaus MO, Barale D, et al. Carinal resection. Thorac Surg Clin 2014;24:477-84. [Crossref] [PubMed]
- Lanuti M, Mathisen DJ. Carinal resection. Thorac Surg Clin 2004;14:199-209. [Crossref] [PubMed]
- Tapias LF, Ott HC, Mathisen DJ. Complications Following Carinal Resections and Sleeve Resections. Thorac Surg Clin 2015;25:435-47. [Crossref] [PubMed]
- de Perrot M, Fadel E, Mercier O, et al. Long-term results after carinal resection for carcinoma: does the benefit warrant the risk? J Thorac Cardiovasc Surg 2006;131:81-9. [Crossref] [PubMed]
Cite this article as: Terra RM, Salati M. Carinal resection. Shanghai Chest 2017;1:17.