
Open repair of pectus deformities
A variety of malformations of the chest wall may be identified in childhood. The most common are the pectus excavatum and pectus carinatum deformities. Pectus excavatum is approximately 6 times more common than pectus carinatum and males are afflicted 5 times more often than females.
Pectus excavatum
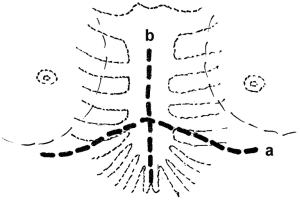
Pectus excavatum, or funnel chest or sunken chest, is a congenital anomaly of the anterior chest wall characterized by a prominent posterior depression of the body of the sternum (Figure 1). The lower costal cartilages bend posteriorly to form a curvature. The first two ribs and the manubrium are usually normal. The most common configuration is a symmetric deformity involving the lower half of the sternum, together with costal flaring on both sides. Asymmetric deformities are common with the concavity deeper on one side and the sternum rotated to that side (1).
The pathogenesis of pectus deformities remains unclear. It has been hypothesized that the deformity results from unbalanced growth in the costochondral regions. This theory may explain the asymmetric deformity in some cases and also the development of pectus carinatum, a completely opposite type of deformity (1,2).
Pectus excavatum can be inherited through either parents, although not clearly as a recessive trait. It is believed to occur in as many as 1 in 300 to 400 live births (2,3). Other malformations may coexist, especially musculoskeletal anomalies like scoliosis—in 11% to 25% of the patients—and Marfan’s syndrome (1,3). Generally the deformity is apparent soon after birth, progresses during early childhood, and becomes even more prominent in early adolescence (1-4). Regression rarely may occur spontaneously.
Most of the children are either asymptomatic in the early years, or shy and are unwilling to expose chest, especially while swimming. During adolescence easy fatigability can be seen. When the deformity is severe, the heart is displaced into the left thoracic cavity (5). Most of the patients have an asthenic habitus and poor posture. Although it was previously believed that only a few patients had respiratory or cardiac insufficiency, several recent studies have provided evidence that both cardiac and respiratory functions tend to show values that are slightly below normal. Electrocardiographic abnormalities are attributed to the abnormal configuration of the chest wall and the displacement and rotation of the heart into the left thoracic cavity (2). Mitral valve prolapse can be seen in some patients, especially with Marfan’s syndrome. Conventional pulmonary function tests while at rest are mostly within normal limits or borderline, in some patients though, they can show a restrictive pattern. In general, it is difficult to obtain valid measurements in young patients (1).
Several methods and indices of quantifying the degree of the severity of pectus deformities have been proposed, although none has been widely accepted. Welch and Haller indices are the most popular ones (6,7). The distance between these two lines is the sagittal measurement. A normal chest has a Haller index of 2 or less. A Haller index between 2 and 3.2 is considered a mild deformity; between 3.2 and 3.5, moderate; 3.5 or greater, a severe deformity. Both moderate and severe deformities can be considered for corrective surgery (8).
Treatment
As most patients with pectus excavatum are asymptomatic, the selection of patients for surgical repair requires good clinical judgement. The primary indication for repair is a cosmetic one. The negative self-image these patients have becomes notable especially when they go to school. They become embarrassed with the attitude of their friends about their deformity, and become withdrawn. Most are shy and have a reserved social life. Therefore, the presence of pectus excavatum in such children is an indication, especially if they have moderate to severe deformity (1,4). Surgical repair of pectus excavatum is indicated also in patients with evidence of respiratory insufficiency, especially dyspnea on exertion.
Surgical repair
Surgical repair of pectus excavatum was first reported by Meyer and Sauerbruch in 1911 and 1920, respectively (9,10). Ochsner and Brown summarized their early experience with surgical repair of this deformity, both in 1939 (11,12). Ravitch in 1949 reported his surgical repair technique, similar to Brown’s, that involved excision of all deformed costal cartilages with their perichondriums, division of the xiphoid from the sternum, division of the intercostal muscle bundles from the sternum, and displacing the sternum anteriorly after transverse sternal osteotomy, using Kirschner wires or silk sutures for stabilisation (13). Current open surgical repair of pectus excavatum encompasses various modifications of the original procedure described by Brown and then modified by Ravitch. In 1958, Welch reported his modification and recommended the preservation of the perichondriums and intercostal muscle bundles (14). Shamberger added a retrosternal steel strut fixation, especially for older children with severe deformities whom complete correction is difficult to achieve by suture fixation of the sternum alone and reported that Rehbein struts could also be used for sternal fixation (2,3).
Although surgical repair of pectus excavatum is technically easier in a younger child as the chest wall is more flexible, the risk of long-term recurrence can be higher in these patients, so the operation can be delayed until the age of ten, as the chest will grow relatively less after that age and the risk of recurrence will be reduced.
Open repair technique
The preferred surgical technique uses general endotracheal anesthesia, with the patient in supine position and the arms abducted slightly. A transverse inframammary incision within the nipple lines is preferred for cosmetic reasons, especially in female patients, to avoid breast deformity, but a midline incision can also be performed (1-4) (Figure 2). The transverse incision is arched slightly towards the body of the sternum like a chevron in the midportion to provide better exposure of the whole sternum. Skin flaps and pectoral muscles are mobilized by electrocautery and are elevated to expose the depressed portion of the sternum and the costal cartilages. With the midline approach, the incision is extended to the periosteum of the sternum, and the pectoral muscle flaps are then elevated laterally, exposing all the costal cartilages (4).
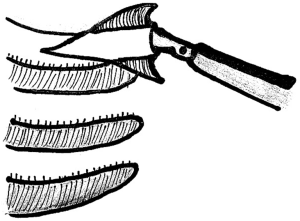
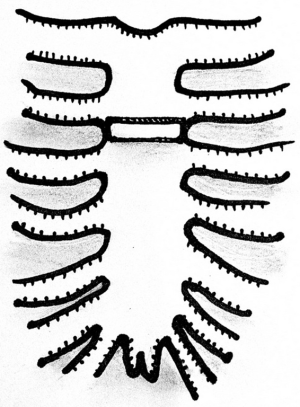
The lateral extent of muscle elevation is the costochondral junction of the third to fifth ribs. The lower four or five costal cartilages are resected subperichondrially for the full length of the deformed segments to the costochondral junctions (Figures 3,4). Limited wedge chondrotomies and osteotomies to release and reshape the anterior chest wall can be preferred instead, especially in milder deformities (15,16). Longer segments of the sixth and seventh cartilages are resected to the point where they join the costal arch. Perichondriums can be resutured when possible to create a tunnel for the new costal cartilages to regenerate within. The xiphoid is divided from its attachment to the sternum and removed if projects too forward, and the mediastinal tissues are bluntly dissected digitally behind the sternum. The attachments of the costal cartilages and intercostal muscles to the sternum can be divided in order to free the lower portion of the sternum and reduce the tension especially if the deformity is too deep, but in general this step can be avoided.

A transverse wedge osteotomy is performed using an oscillator blade through the anterior table of the sternum at the level of superior transition from the normal to the depressed sternum (Figure 5). The posterior table of the sternum is partially fractured, and the lower sternum is then elevated to the desired position, preferably with some overcorrection, and it is secured either with interrupted nonabsorbable sutures or steel wires (Figure 6) (1-4). Titanium bars, titanium or absorbable copolymer plates can also be used for sternal fixation (Figure 7) (15,17,18).
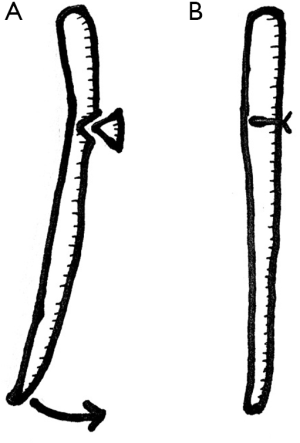

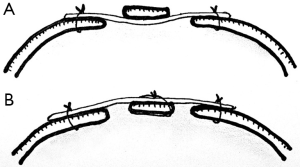
Additionally, a retrosternal steel strut can be placed to hold the sternum forward. The strut is placed transversely behind the sternum, where it is attached on each side to the rib just lateral to the costochondral junction (Figure 8A). When extensive costal cartilage resection is performed and a long segment of sternum is mobilized below the osteotomy line a retrosternal support strut should be used to avoid recurrent sternal depression (1). Alternatively an anterior support strut with a large wire holding the sternum to the strut can be placed (Figure 8B). Struts are also helpful when there is extensive sternal rotation or a severe depression (2,3). Retrosternal support with struts is also required in patients with Marfan syndrome as the risk of recurrence is higher in them (19).
An alternative material for retrosternal support can be a Marlex mesh. A sheet of Marlex mesh is spread tightly behind the sternum like a drum and attached laterally to the most anterior areas of the residual costal cartilages with nonabsorbable sutures, letting the sternum rest on the mesh in a corrected position (20).
The wound should be filled with warm saline to check if the pleural cavities were entered or not. Air can be evacuated with a small-bore suction catheter if needed. A single limb aspirative drain is then brought through the inferior skin flap and placed over the sternum and the costal cartilages. The pectoral muscle flaps are sutured to the sternum in the midline, advancing the flaps inferiorly to cover the underlying sternum. The rectus muscle flap is sutured to the tip of the sternum also, to cover the mediastinum completely. Absorbable subcuticular sutures are used in preference to skin sutures in children (Figure 9). The aspirative drain is removed when the drainage is less than 50 mL for 24-hour period. At the time of discharge the patients are advised to avoid body-contact sports for 3 to 6 months or until after the retrosternal steel strut is removed, if placed. New cartilage or bone regeneration within the perichondriums is usually complete within 2 months after the surgical repair and it provides a rigid support for the anterior chest wall.
Complications
Complications of open surgical repair of pectus excavatum are few and relatively unimportant. Pneumothorax may require aspiration and rarely tube thoracostomy. Wound infection can be overcome by perioperative antibiotic usage. The most important complication is the recurrence of the deformity. It is difficult to predict which patients will have a major recurrence, but mostly patients with asthenic or marfanoid habitus having poor muscle development and a narrow anteroposterior chest wall diameter are under greater risk (2,3).
The patients should be followed to full growth, until 16 years of age for girls and 19 for boys, not to miss any recurrence. The rate of recurrence is less then 2%, especially when prosthetic sternal supports are used in the repair (21).
Pectus carinatum
Pectus carinatum, or pigeon breast or keel chest, is the anterior protrusion of the sternum and it is less common than pectus excavatum (1-3). An upward curve in the lower costal cartilages results with the moving forward of the sternum (4). Pectus carinatum is more variable than pectus excavatum in subtypes. Two principal types are chondrogladiolar and chondromanubrial pectus carinatum. Chondrogladiolar type is more common and it has the greatest prominence in the lower portion of the sternum (Figure 10). In chondromanubrial type, also called as pectus arcuatum, the protuberance is more prominent in the upper portion of the sternum and the lower portion is short and relatively depressed (Figures 11,12) (1-3). Asymmetric deformities with a tilted sternum are common. Associated disorders like scoliosis, Marfanoid habitus and congenital heart diseases are more frequent than in patients with pectus excavatum (1). The deformity is generally mild in childhood and becomes prominent in early adolescence. It is often obvious and can be seen through the clothing. Symptoms are present in some patients and may include cardiac arrhythmias and dyspnea on exertion. Inability to sleep prone or pain from local trauma to the protruding deformity are the most common symptoms (3). The physiologic problem is related to the reduced flexibility of the chest wall by the anteriorly displaced sternum and deformed cartilages causing difficulty in chest wall expantion during inspiration (1,4).


Treatment
The primary indication for repair is a cosmetic one in general as in pectus excavatum. Surgical repair is indicated also in patients with evidence of progressive symptoms of dyspnea, reduced endurance and tachypnea on exertion. Adolescents with severe pectus carinatum are often more likely to seek surgical treatment than patients with severe pectus excavatum (22).
Surgical repair
The first repair of pectus carinatum was done by Ravitch in 1952 on a chondromanubrial type deformity (23). He resected multiple costal cartilages as in open repair of pectus excavatum, and performed a double sternal osteotomy. Robicsek reported his open repair technique for pectus carinatum in 1963 (24). He resected the costal cartilages subperichondrially, performed a transverse sternal osteotomy and displacement, and resection of the protruding lower portion of the sternum. Considerable variations in surgical treatment are necessary because of the diversity of pectus carinatum.
Open repair technique
Open repair technique for pectus carinatum is more or less a variation of the open repair technique for pectus excavatum. It can be done with either a midline or a transverse submammary incision. The same exposure through the skin and muscle flaps is used with resection of the involved costal cartilages subperichondrially, leaving the perichondriums intact. Multiple reefing sutures can be placed to remove the redundancy in the perichondrial beds (4). A transverse osteotomy across the anterior table of the upper sternum is done using an oscillator blade and it is filled with a wedge of costal cartilage to secure it in an orthotopic position. Occasionally a second osteotomy may be required to displace the lower portion of the sternum posteriorly. Interrupted nonabsorbable sutures, steel wires, titanium or absorbable copolymer plates can be used for sternal fixation over the osteotomy line (16,24-26). The remainder of the repair is similar to that is done for pectus excavatum, including the closure and postoperative drainage. A retrosternal steel strut is helpful for temporary chest wall stabilization in severe deformities. Alternatively an anterior support strut with a large wire holding the sternum to the strut can be placed to avoid opening of the pleural spaces (16). Asymmetric pectus carinatum may require unilateral costal cartilage resection with transverse wedge shaped resection of the sternum only on that side, allowing anterior displacement and rotation of it (1-3). The sternal support strut can be removed 6 months after repair (Figure 13).
Chondromanubrial type pectus excavatum must be managed with a slightly different technique. The costal cartilages must be resected starting from the second cartilage, mostly together with third and fourth cartilages on both sides. A wide wedge osteotomy is performed at the point of maximal protrusion of the sternum, generally at the level of the second costal cartilage. Sometimes a second wedge osteotomy is needed to provide a better shape of the sternum. The superior segment of the sternum can then be displaced posteriorly, and advancing the inferior fragment anteriorly the osteotomy is stabilized. Different materials can be used for this stabilisation also, such as interrupted steel wires, absorbable copolymer plates or titanium plates (Figures 14,15) (18,27,28).
Complications
Complications after open repair of pectus carinatum are rarely seen and they are similar to the ones seen after repair of pectus excavatum, such as pneumothorax and wound infection. Recurrence of the deformity is the most important complication again and it is less frequent than in pectus excavatum.
Conclusions
Although minimally invasive repair of pectus excavatum and carinatum has become quite popular in recent years, open repair of pectus deformities are successfully performed in many centers around the world with low morbidity, low cost, short limitation of activity and a good quality of life improvement. The optimal age for surgical treatment of pectus deformities is during adolescent years as surgery is technically easier, but adult patients should also be considered as candidates for surgical treatment if they are symptomatic.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Fonkalsrud EW. Chest wall abnormalities. In: Baue AE, Geha AS, Hammond GL, et al. editors. Glenn’s Thoracic and Cardiovascular Surgery. Stamford: Appleton & Lange, 1996:581-92.
- Shamberger RC. Chest wall deformities. In: Shields TW. editor. General Thoracic Surgery. Malvern: Williams & Wilkins, 1994:529-57.
- Shamberger RC, Hendren WH 3rd. Congenital deformities. In: Pearson FG, Deslauriers J, Ginsberg RJ, et al. editors. Thoracic Surgery. New York: Churchill Livingstone, 1995:1189-209.
- Sabiston DC Jr. Disorders of the sternum and the thoracic wall. Congenital deformities of the chest wall. In: Sabiston DC Jr, Spencer FC. editors. Gibbon’s Surgery of the Chest. Philadelphia: WB Saunders Company, 1990:418-37.
- Ravitch MM. Pectus excavatum and heart failure. Surgery 1951;30:178-94. [PubMed]
- Welch KJ. Chest wall deformities. In: Holder TH, Ashcraft K. editors. Pediatric Surgery. Philadelphia: WB Saunders Company, 1980:162-82.
- Haller JA, Kramer SS, Lietman A. Use of CT scans in selection of patients for pectus excavatum surgery: a preliminary report. J Pediatr Surg 1987;22:904-6. [Crossref] [PubMed]
- Sidden CR, Katz ME, Swoveland BC, et al. Radiologic considerations in patients undergoing the Nuss procedure for correction of pectus excavatum. Pediatric Radiology 2001;31:429-34. [Crossref] [PubMed]
- Meyer L. Zur chirurgiscen behandlung der angeborenen Trichterbrust. Verh Berl Med Ges 1911;42:364-73.
- Sauerbruch F. Die Chirurgie der Brustorgane. J. Springer, 1920.
- Ochsner A, DeBakey M. Chone-chondrosternon: report of a case and review of the literature. J Thorac Surg 1939;8:469-511.
- Brown AL. Pectus excavatum (funnel chest). J Thorac Surg 1939;9:164-84.
- Ravitch MM. The operative treatment of pectus excavatum. Ann Surg 1949;129:429-44. [Crossref] [PubMed]
- Welch KJ. Satisfactory surgical correction of pectus excavatum deformity in childhood: a limited opportunity. J Thorac Surg 1958;36:697-713. [PubMed]
- Wihlm JM. Open repair of pectus excavatum and pectus carinatum. In: Kuzdzal J, Asamura H, Detterbeck F, et al. editors. ESTS Textbook of Thoracic Surgery. Cracow: Medycyna Praktyczna, 2015:67-85.
- Jaroszewski DE, Fonkalsrud EW. Repair of pectus chest deformities in 320 adult patients: 21 year experience. Ann Thorac Surg 2007;84:429-33. [Crossref] [PubMed]
- Genc O, Gurkok S, Gözübüyük A, et al. Repair of pectus deformities: experience and outcome in 317 cases. Ann Saudi Med 2006;26:370-4. [Crossref] [PubMed]
- Yuksel M, Bostanci K, Eldem B. Stabilizing the sternum using an absorbable copolymer plate after open surgery for pectus deformities: New techniques to stabilize the anterior chest wall after open surgery for pectus excavatum. Multimed Man Cardiothorac Surg 2011;2011:mmcts.2010.004879. [PubMed]
- Scherer LR, Arn PH, Dressel DA, et al. Surgical management of children and young adults with Marfan syndrome and pectus excavatum. J Pediatr Surg 1988;23:1169-72. [Crossref] [PubMed]
- Robicsek F. Marlex mesh support for the correction of very severe and recurrent pectus excavatum. Ann Thorac Surg 1978;26:80-3. [Crossref] [PubMed]
- Fonkalsrud EW, Salman T, Guo W, et al. Repair of pectus deformities with sternal support. J Thorac Cardiovasc Surg 1994;107:37-42. [PubMed]
- Fonkalsrud EW. Surgical correction of pectus carinatum: lessons learned from 260 patients. J Pediatr Surg 2008;43:1235-43. [Crossref] [PubMed]
- Ravitch MM. Unusual sternal deformity with cardiac symptoms—operative correction. J Thorac Surg 1952;23:138-44. [PubMed]
- Robicsek F, Sanger PW, Taylor FH, et al. The surgical treatment of chondrosternal prominence (pectus carinatum). J Thorac Cardiovasc Surg 1963;45:691-701. [PubMed]
- Robicsek F, Watts LT, Fokin AA. Surgical repair of pectus excavatum and carinatum. Semin Thorac Cardiovasc Surg 2009;21:64-75. [Crossref] [PubMed]
- Scarci M, Bertolaccini L, Panagiotopoulos N, et al. Open repair of pectus carinatum. J Vis Surg 2016;2:50-3. [Crossref]
- Brichon PY, Wihlm JM. Correction of a severe pouter pigeon breast by triple sternal osteotomy with a novel titanium rib bridge fixation. Ann Thorac Surg 2010;90:e97-9. [Crossref] [PubMed]
- Kim SY, Park S, Kim ER, et al. A case of successful surgical repair for pectus arcuatum using chondrosternoplasty. Korean J Thorac Cardiovasc Surg 2016;49:214-7. [Crossref] [PubMed]
Cite this article as: Bostanci K, Stamenovic D. Open repair of pectus deformities. Shanghai Chest 2017;1:18.








