
Right side sleeves
Introduction
Bronchial and vascular reconstructive procedures are demanding operations performed in case of infiltration of the bronchial tree and/or the pulmonary artery (PA) and its branches.
In the past these procedures were described for patients with lung tumors whose pulmonary reserve was judged inadequate to permit pneumonectomy. Since then, many clinical series confirm that these bronchoplastic/angioplastic procedures may provide as good as better results than pneumonectomy in selected cases of lung tumors involving the bronchial/vascular tree.
Nowadays, these lung-sparing reconstructive procedures are been widely adopted in many centers with good long-term outcomes above all if compared to the results reported after pneumonectomy (1-3).
The basic technique and the principles of broncho/vascular reconstructive procedures were well previously established (4-7). In every case, it is essential to recognize the surgical anatomy of the bronchial and vascular tree in order to safety perform bronchoplastic and angioplastic procedures and reduce the risks of complications.
Tracheal carina is located in correspondence of the IV dorsal vertebra. At this level, trachea bifurcates into mainstem bronchi (right and left). Right mainstem bronchus is in the same axis of the trachea and the distance between carina and the orifice of the right upper lobar bronchus varies between 1.5 and 2.0 cm. Distal to this latter, there is the bronchus intermedius whose length is about 2.0 cm. The greater length of the bronchus intermedius makes a bronchial sleeve resection easier and explains why bronchoplasties are frequently associated with right upper lobectomies. The bronchus for the middle lobe originates from the frontal aspect of the bronchus intermedius at the same level of the orifice of the superior segmental bronchus of the lower lobe. This one originates at the posterior portion of the bronchus intermedius. Sometimes, when a right upper sleeve lobectomy is performed, the distal bronchial resection may fall proximally to the origin of these two segmental bronchi: in this case, great attention should be taken to avoid their stenosis during bronchial reconstruction. There is sometimes a significant mismatch between the bronchi due to their different diameter: in these cases, a “telescopic” bronchial anastomosis may solve this problem.
Another important aspect is the bronchial vascularization anatomy in order to prevent anastomotic complications. Site of origin, number, and course of bronchial arteries is rather variable, sometimes originating from descending thoracic aorta or from intercostal arteries. On the right side, there is generally a single bronchial artery which originates from an intercostal artery. This artery runs in the posterior portion of the mainstem bronchus (membranous aspect), parallel to the azygous vein. Anyway, the bronchial circulation system has a wide anastomotic network connecting it with the pulmonary arterial circulation.
Very important is also the surgical anatomy of the PA. After its origin below the aortic arch, the right PA moves in a horizontal plane, posteriorly to the aorta and superior vena cava, below the carina, running for the majority of its course intrapericardially. Then, once it is left out the pericardium, PA passes anteriorly to the right mainstem bronchus. This is the place where a bronchovascular fistulas may occur after bronchoplasty and for this reasons a pedunculated flap should be always used to wrap the bronchial anastomosis. Then, from the PA rises the first arterial branch, the truncus anterior or Boyden trunk for the upper lobe. Then it runs inferiorly between the bronchus intermedium posteriorly and the superior pulmonary vein anteriorly. At this level, the PA is closely applied to the undersurface of the vein, and careless dissection may be hazardous.
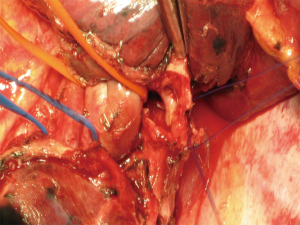
Indications for right sleeve resections are the presence of tumors which infiltrate usually the origin of the upper lobar bronchus (Figure 1), associated or not to invasion of PA or the origin of vascular branch. Moreover, a right sleeve resection may be indicated in case of presence of infiltration of the bronchial tree and/or the PA by a hilar lymph node. In some instances, the presence of fibrotic tissue or residual tumor after neoadjuvant treatments may also be another indication to perform broncho-angioplastic procedures.

Preoperative assessment has been largely reported in the Chapter of Left Side Sleeves. Briefly, preoperative evaluation includes computed tomography scan of the brain, chest, and upper abdomen, and PET scan. Bronchoscopy is always performed to evaluate the level of bronchial infiltration and for obtaining the diagnosis. EBUS is usually preoperatively performed for evaluating the mediastinal nodes involvement. Preoperative cardiologic and pneumologic evaluation is mandatory.
Operative technique
Preparation and exposition
Patient’s preparation and exposition has been reported in the Chapter of Left Side Sleeves. Briefly, after general anesthesia, a double-lumen endotracheal tube is placed in the left mainstem bronchus and confirmed by fiberoptic bronchoscopy. The intervention is performed with the patient in lateral position entering into the thorax through the 4th of 5th intercostal space (Figure 2).

Operation
When entering the chest, the right hemithorax is carefully examined for evidence of intrathoracic spread. Fissures are completely dissected. The right lower and middle lobes are carefully examined for evidence of second primaries or metastatic disease. The right mediastinal pleura are circumferentially incised around the hilum and the inferior pulmonary ligament is mobilized. The posterior hilum is examined for unexpected extension of the tumor into the mainstem bronchus or distal bronchus intermedius. Dissection of mediastinal and hilar nodes is performed avoiding to devascularise the bronchial tree at the level of the section line. The proximal main PA and superior pulmonary vein are fully dissected. The main PA is encircled with vascular tape which facilitates proximal clamping of the PA in case of an angioplastic procedure or vascular sleeve resection is required. Although angioplasty is unusual in right upper-lobe sleeve resections, mobilization of the entire PA is required for an adequate airway dissection. In addition, the vascular tape facilitates exposure of the airway with anterior retraction of the ongoing PA.
When the hilum is dissected, the truncus anterior artery is divided with a vascular stapler. The vascular stapler we typically use is a 30-mm thoracoscopic stapler that can also be used to transect the superior pulmonary vein. After transection of the proximal artery and vein, the posterior recurrent branch of the PA is readily exposed and divided. The PA should be fully mobilized to the level of the superior segmental artery.
The division of the posterior recurrent branch of the PA facilitates complete mobilization of the right upper-lobe major fissure. Whether sharp dissection, electrocautery, or a stapler is used to complete the fissure, care must be taken to minimize any potential air leaks. The minor fissure is usually completed with a stapler.
The right upper lobe is fully mobilized before transecting the airway. First, the right mainstem bronchus is mobilized by passing umbilical tape around in the airway. Similarly, the bronchus intermedius is mobilized and encircled with umbilical tape. The proximal and distal tapes permit a careful inspection of the potential surgical margins before transecting the airway. The relative size mismatch of the airways can also be evaluated.
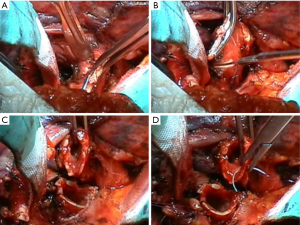
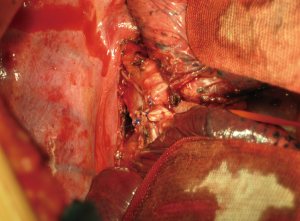
The bronchus is transected in a plane transverse to the axis of the airway. The perpendicular transection of the airway minimizes the size mismatch and facilitates the subsequent anastomosis. Figure 3 represents a schematic drawing of a right upper slleve bronchial resection and anastomosis while Figure 4A,B shows the intraoperative view of the bronchial transection. The oblique orientation of the airway cartilage can be misleading. The use of a needle-nose clamp to crush the cartilage in the appropriate orientation may be helpful in a teaching setting. When both the proximal and distal airways have been transected, the specimen is submitted to the pathology laboratory for frozen section evaluation of both the proximal and distal margins.

The orientation of the proximal and distal airways can be maintained with traction sutures. Although the orientation is more problematic in other sleeve lobectomies, we routinely place 3-0 monofilament traction sutures at the cartilaginous membranous junction. The sutures are placed in the cartilage to allow rotational traction in the airway and facilitate exposure for the anastomosis.
The cartilaginous portion of the anastomosis is constructed using two 3-0 monofilament (polypropylene) sutures. Stitches are anchored and knotted at the level of the cartilaginous wall (Figure 4C,D). Then, two running sutures are performed and a telescopic anastomosis is obtained; Figure 5A,B). At the end of the suture, stiches are well pulled by means of a hook (Figure 5C,D). Monofilament sutures provide additional strength for the first several months after airway reconstruction. The persistence of these sutures may help minimize the rotational deformation of the airway that can be bronchoscopically observed several years after sleeve resection. In addition, monofilament sutures are more convenient to use with a running technique.
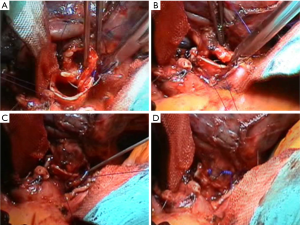
In some exceptionally cases, a right angioplasty is needed (Figure 6). The technical aspects of PA reconstruction have been largely reported in the Chapter of Left Side Sleeves.

After completion of the anastomosis, the remaining right lung is ventilated. The anastomosis can be tested for an air leak using saline irrigation. The care taken to prevent an air leak in the major and minor fissures is rewarded by the absence of air bubbles near the bronchial reconstruction. Because the completed major and minor fissures rotate toward the anastomosis with reinflation, the evaluation of the source of the air leak can be ambiguous. The remaining middle and lower lobes should reinflate easily. Intraoperative bronchoscopy can be useful to evaluate the anastomosis and remove any retained secretions.
Although uncomplicated anastomotic healing is the rule, any airway separation or perianastomotic infection can lead to a catastrophic bronchovascular fistula. Normal tissue can be interposed between the bronchial anastomosis and the PA to prevent this complication. We typically mobilize the right lobe of the thymus gland and wrap the thymic fat between the artery and airway.
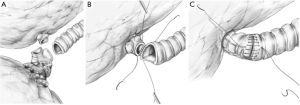
On rare occasions, a middle lobectomy with sleeve resection of the bronchus intermedius may be indicated (Figures 7,8). In this case an angled transection of the bronchus intermedius is performed resecting the origin of the middle bronchus and sparing the origin of the superior segment of the lower lobe (Figures 9,10). In this maneuver great attention should be taken in preserving the PA which is located posteriorly to the bronchus.
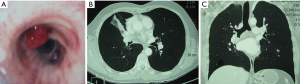
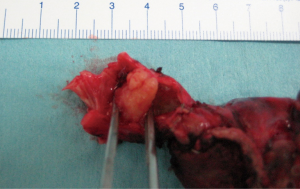
In case of endoluminal lesion in the bronchus intermedius, a sleeve bilobectomy may be required. The bronchial transection of the mainstem bronchus should be performed at the level of the upper bronchial origin while the resection of the bronchus intermedius should be performed just beneath the orifice of the upper bronchus. The bronchoplasty between mainstem bronchus and the upper right bronchus is then performed. In this case, due to the particular angle of the anastomosis and re-orientation of the bronchial axis, particular attention should be taken to avoid bronchial torsion (Figure 11).
Postoperative management of patients receiving bronchoplasty has been described in the Chapter of Left Side Sleeves.
Comments
Bronchial sleeve resection of the right upper lobe is the most common bronchoplastic procedure. The procedure should be considered in any patient with a proximal right upper-lobe tumor. Staging of the patient should include a bronchoscopic evaluation of the potential resection margin. Potential nodal metastases need to be carefully evaluated by endobronchial ultrasound. At the time of thoracotomy, additional nodal sampling is required to assess the feasibility of sleeve resection. The surgeon who methodically evaluates each patient for possible sleeve resection will often be rewarded with an operation that produces an acceptable oncological result while preserving lung tissue and improving the quality of their patients’ postoperative survival.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Deslauriers J, Gaulin P, Beaulieu M, et al. Long-term clinical and functional results of sleeve lobectomy for primary lung cancer. J Thorac Cardiovasc Surg 1986;92:871-9. [PubMed]
- Ludwig C, Stoelben E, Olschewski M, et al. Comparison of morbidity, 30-day mortality, and long-term survival after pneumonectomy and sleeve lobectomy for non-small cell lung carcinoma. Ann Thorac Surg 2005;79:968-73. [Crossref] [PubMed]
- Takeda S, Maeda H, Koma M, et al. Comparison of surgical results after pneumonectomy and sleeve lobectomy for non-small cell lung cancer: trends over time and 20-year institutional experience. Eur J Cardiothorac Surg 2006;29:276-80. [Crossref] [PubMed]
- Price Thomas C. Conservative resection of the bronchial tree. J R Coll Surg (Edinb) 1956;1:169-86. [PubMed]
- Johnston JB, Jones PH. The treatment of bronchial carcinoma by lobectomy and sleeve resection of the main bronchus. Thorax 1959;14:48-54. [Crossref] [PubMed]
- Vogt-Moykopf I, Frits TH, Meyer G, et al. Bronchoplastic and angioplastic operation in bronchial carcinoma: long-term results of a retrospective analysis from 1973 to 1983. Int Surg 1986;71:211-20. [PubMed]
- Vogt-Moykopf I, Fritz T, Bülzebruck H, et al. Bronchoplastic and angioplastic operation in bronchial carcinoma. Langenbecks Arch Chir 1987;371:85-101. [Crossref] [PubMed]
Cite this article as: Galetta D, Spaggiari L. Right side sleeves. Shanghai Chest 2017;1:33.


