
Transition from two-three port to uniportal approach in video-assisted thoracoscopic surgery lobectomy: a multicentre comparative study
Introduction
Minimal invasiveness is currently aimed in most surgical interventions. In thoracic surgery, Video-assisted thoracoscopic surgery (VATS) lobectomy for treatment of both benign and malignant diseases, has become a standard and is widely used in many centres. Transition from open surgery to VATS has a learning curve, like introduction of any new surgical technique, depending on the complexity of the procedure and previous experience of the operating surgeon (1-3).
A step further towards less invasiveness in thoracic surgery is using only one incision—the uniportal approach. Uniportal lobectomy is associated with a better cosmetic result, diminished postoperative pain (4-6), and it allows straight view to the operating field (7). However, having only one access to the thoracic cavity is in contradiction with the traditional understanding of triangular placement of instruments in minimally invasive surgery (8,9), and is therefore believed to be technically more challenging. Our impression was that conversion from two-three port VATS lobectomy to uniport VATS lobectomy was not too demanding. Therefore, we designed the current study to analyse the possible learning curve related to introducing the uniportal lobectomy technique.
The aim of the study was to compare the main indicators of VATS lobectomies performed before and after switching to uniportal approach in five European thoracic surgery centres with significant previous two-three port VATS lobectomy experience.
Methods
Five thoracic surgery centres (Tartu, Estonia; Riga, Latvia; Klaipeda, Lithuania; Budapest, Hungary and Istanbul, Turkey) participated in the study. Data were collected retrospectively from hospital medical records. All centres switched promptly from multiportal to uniportal lobectomy approach without any transition period. A single thoracic surgeon with previous experience of more than 100 VATS lobectomies performed all the operations in each centre.
In all the centres last 20 (consecutive) VATS lobectomies before implementing the uniportal approach were included—these 100 patients belonged to study group I. Study group II consisted of first 20 (consecutive) uniportal VATS lobectomies, performed in each of the five centres. Thus 40 consecutive VATS lobectomies from each study centre were included. It was considered optimal number to keep the study period short and to avoid any possible bias due to changes in practice during a longer period, albeit it should allow demonstrating changes related to implementation of uniportal approach. The study might be underpowered to reveal minor advantages of one or another approach.
General anaesthesia with double lumen intubation and single-lung ventilation was routinely used. Patient was placed in lateral decubitus position. The multiport approach consisted of 4–5 cm axillary utility incision and one or two additional ports for the camera and instruments. In uniportal approach, only the utility incision similar to the one in the multiport approach was made. No rib retractor was used in any of the patients. In majority of the patients a chest tube was left into pleural cavity through either the camera port or the utility incision (in case of the uniportal approach).
To characterize the study participants, the following data were extracted from medical records: patients’ age, gender, body mass index (BMI), main diagnosis and the lobe involved. The study groups were compared, based on the following data: duration of the operation, intraoperative blood loss, conversion to thoracotomy or to two-three port access (in case of uniportal approach), postoperative complications, blood transfusion(s), in-hospital mortality, duration of pleural drainage and hospitalization.
Student’s t-test and Mann-Whitney U test were used for statistical analysis. P value less than 0.05 was considered statistically significant.
Results
In study group I (100 conventional VATS lobectomies) two-port access was used in 30 cases and three-port access in 70 cases. Study group II consisted of 100 uniportal VATS lobectomies. The study groups did not differ in terms of age, gender, BMI, diagnosis, or the lobe removed (Table 1).
Table 1
| Characteristic | Multiportal VATS lobectomy | Uniportal VATS lobectomy | P |
|---|---|---|---|
| Age (years) (mean ± SD) | 61.7±10.9 | 64.1±11.0 | 0.13 |
| Gender | 0.14 | ||
| Male | 60 | 70 | |
| Female | 40 | 30 | |
| Body mass index (mean ± SD) | 26.9±5.3 | 26.5±4.0 | 0.57 |
| Diagnosis | 0.32 | ||
| Lung cancer | 81 | 76 | |
| Metastasis | 3 | 10 | |
| Tuberculosis | 4 | 5 | |
| Other | 12 | 9 | |
| Lobe | 0.67 | ||
| Right upper lobe | 34 | 33 | |
| Right middle lobe | 6 | 6 | |
| Right lower lobe | 15 | 22 | |
| Left upper lobe | 21 | 19 | |
| Left lower lobe | 24 | 20 |
VATS, video-assisted thoracoscopic surgery.
Lung cancer was the most common diagnosis in both study groups: 81 cases in group I and 76 cases in group II.
In nine cases (9%) the uniportal approach (group II) was converted to two-port approach. The main reason being difficulty of inserting a vascular stapler (seven cases), and in two cases either a centrally located or a large tumour, complicating dissection of hilar structures.
Conversion to thoracotomy was needed in six cases (6%) in both study groups (P=1.00). Reasons for conversion were: (I) in group I technically difficult dissection of lobar structures [3], large tumour [1], stapler malfunction [1], and bleeding [1]; (II) in group II technically difficult dissection of lobar structures [1], centrally located invasive tumour [1], patient unable to tolerate one-lung ventilation [1], and bleeding [3].
Duration of the operation and intraoperative blood loss did not differ in the two study groups (Table 2). Also, the postoperative complications: need for postoperative blood transfusion, rate of prolonged air-leak, postoperative pneumonia, atrial fibrillation and other complications did not differ in the two study groups (Table 3). Four patients in multi- and five patients in uniportal lobectomy group needed postoperative blood transfusion (P=0.52).
Table 2
| Characteristic | Multiportal VATS lobectomy | Uniportal VATS lobectomy | P |
|---|---|---|---|
| Duration of the operation (min) (mean ± SD) | 148±55 | 148±58 | 0.81 |
| Intraoperative blood loss (mL) (mean ± SD) | 134±161 | 113±143 | 0.46 |
| No. of patients needed conversion to thoracotomy [%] | 6 [6] | 6 [6] | 1.00 |
VATS, video-assisted thoracoscopic surgery.
Table 3
| Postoperative complications [n (%)] | Multiportal VATS lobectomy | Uniportal VATS lobectomy | P |
|---|---|---|---|
| Total | 36 [36] | 35 [35] | 0.95 |
| Postoperative prolonged air-leak (>5 days) | 11 [11] | 12 [12] | 0.83 |
| Postoperative pneumonia | 4 [4] | 7 [7] | 0.35 |
| Postoperative atrial fibrillation | 6 [6] | 4 [4] | 0.52 |
| Other complications | 15 [15] | 12 [12] | – |
VATS, video-assisted thoracoscopic surgery.
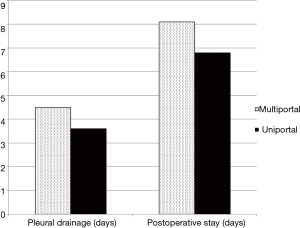
Mean duration of postoperative pleural drainage was 4.5 days in multi- and 3.6 days in uniportal lobectomy group (P=0.12) (Figure 1). Trend towards shorter duration of postoperative hospital stay was found in uniportal group (mean 8.1 vs. 6.8 days, P=0.059). No in-hospital mortality occurred in either of the groups.
Discussion
Uniportal VATS lobectomy was introduced by Dr. Gonzalez Rivas in 2011 (10). Although several thoracic surgery centres have gradually accepted this approach, it is not universally implemented. One of the reasons is probably the belief that uniportal approach makes the operation more difficult. Since the introduction of thoracoscopic surgery and VATS lobectomy, triangular placement of instruments has been advocated access to the thoracic cavity (8,9). Inserting all the instruments and the camera through the same small incision may result in interference between the instruments and is believed to make complex operations (like lobectomy) technically challenging. However, besides lobectomy recently even more complex operations like bronchial and vascular sleeve resections have been performed by uniportal approach (11).
The potential advantage of a single port access, compared to two or three ports in different intercostal spaces, is less trauma to the chest wall, resulting in diminished postoperative pain and paraesthesia (4-6), as well as a better cosmetic result. In uniportal approach, the camera and instruments are parallel, which gives to the surgeon a straight view to the operating field, as in open surgery (12).
There is no doubt that implementing a new surgical method has a learning curve, also seen in transition from open to VATS lobectomy (1). Transition from open to thoracoscopic lobectomy is usually stepwise, applied first in uncomplicated cases and then, after some experience, attempted in more complex cases (13). Several studies have demonstrated a gradual decrease in operation duration and intraoperative blood loss at the beginning of VATS lobectomy experience (2,3). Zhao et al. have suggested that 30–60 operations should be performed to achieve a stable level of surgical skills (3). According to a recent best evidence topic paper, VATS lobectomy learning curve was not eliminated by the extent of previous experience in open lobectomy (1).
However, there is very little information available about the learning curve when initiating a new thoracoscopic operation after considerable previous experience in minimally invasive surgery. Our multicentre study revealed that implementing the uniportal approach in VATS lobectomy is not related to a learning curve in case of previous experience with the multiportal approach. The duration of the operation, intraoperative bleeding, need to convert the VATS approach to an open approach and the rate of postoperative complications were similar in our study groups. After having implemented the uniportal approach, we used it in all the following cases when VATS lobectomy was indicated. Previously published opinions have been contradictory—both stepwise transition to uniportal approach (12) and prompt implementation have been preferred (14). Although in a study from Canada, Drevet et al. found a steep learning curve during first 180 uniportal VATS anatomic lung resections, they did not compare the results of these uniportal VATS operations with previous multiportal ones (15).
We chose a short time-period for our study (40 consecutive VATS lobectomies from each study centre—20 immediately before and 20 after implementing the uniportal approach) to avoid potential bias due to possible changes in practice in a longer period. In addition, all surgeons in our study already had considerable multiportal VATS lobectomy experience, and thus had already gone through the open to VATS lobectomy learning curve.
When comparing our data with previously reported either uni- or multiportal VATS lobectomy series, the results were similar. The duration of the operation was similar to previously reported durations of 144–181 and 121–200 min, respectively (2,4,13,15-17). The intraoperative blood loss and the rate of postoperative complications were also well in line with previously reported rates (13,15,17,18). Also, in a recent meta-analysis no difference between uni- and multiportal VATS lobectomy with regards to duration of the operation and intraoperative blood loss was found (19).
Conversion from VATS to thoracotomy is recommended when during the operation technical difficulties or complications (especially major uncontrollable bleeding) occur. Conversion rates vary between 4.3% to 21% (2,13,15,17,20). In our study, conversion to thoracotomy had same frequency in both study groups—6%. In uniportal approach, sometimes adding one port i.e., converting to two ports instead of converting to thoracotomy, could help. In our study the conversion rate from one to two ports was 9%. Previously, conversion rates between 7% to 24.4% have been reported (15,17). The main reason for making the extra incision has been inability to safely insert a vascular stapler. Newer staplers with better angulation and probably also the increasing experience will in the future likely reduce the need to convert due to this reason (7). In our study we saw only a few patients who we could not operate on by uniportal approach, but by just adding one additional port the thoracoscopic approach was still maintained. Thus, when evaluating the uniportal approach, conversion to open access and multiportal approach should be presented separately.
In our study, postoperative hospital stay was shorter in uniportal lobectomy cases. Similar findings have been reported in a few previous studies and a recent meta-analysis (17,19). A possible explanation for this phenomenon is reduced postoperative pain and thus faster recovery. Unfortunately, we did not systematically record post-operative pain scores, and thus the conclusion is only speculative. Two previous studies have demonstrated reduced postoperative pain after uniportal lobectomy compared to multiport access (4,14), however in one of the studies this difference remained significant only in the first postoperative hour (14).
The limitations of our study derive from some variation in practices between the study centres, however all centres provided equal number of uni- and multiportal VATS patients to balance this potential bias. For example, the retrospective study design did not allow us to predefine criteria when to remove the chest tube and when to discharge the patient from hospital. Tradition how long to keep a patient in hospital after the operation was somewhat different in study centres but each hospital included the same number of uni- and multiportal operations to balance this bias. Relatively long postoperative stay is related to the fact that the study centres received patients from all over the country. Thus, many patients had to travel long distances and were kept longer in hospital to be sure about any postoperative complications. Also, data on postoperative pain were not routinely registered, not allowing us to analyse the importance of pain in postoperative recovery. Although postoperative stay was shorter in the uniportal group, it was not statistically significant, probably related to the relatively small sample size in our study.
Conclusions
In summary, transition from two-three port to uniportal approach in VATS lobectomy did not prolong the operation, increase the rate of intra- and postoperative complications, and conversion rate to thoracotomy. Postoperative hospital stay after uniportal lobectomy was shorter compared to the multiport technique, although the difference did not reach statistical significance. There was no evidence of a learning curve while implementing uniportal VATS lobectomy after previous experience with the multiportal approach.
We encourage thoracic surgeons to implement uniportal VATS lobectomy—it may appear more challenging than it actually is, and it has potential benefits for patients.
Acknowledgments
Funding: None.
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/shc.2017.11.01). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). Institutional ethical approval and individual informed consent were waived due to the retrospective nature of the study.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Okyere S, Attia R, Toufektzian L, et al. Is the learning curve for video-assisted thoracoscopic lobectomy affected by prior experience in open lobectomy? Interact Cardiovasc Thorac Surg 2015;21:108-12. [Crossref] [PubMed]
- Ferguson J, Walker W. Developing a VATS lobectomy programme-can VATS lobectomy be taught? Eur J Cardiothorac Surg 2006;29:806-9. [Crossref] [PubMed]
- Zhao H, Bu L, Yang F, et al. Video-assisted thoracoscopic surgery lobectomy for lung cancer: the learning curve. World J Surg 2010;34:2368-72. [Crossref] [PubMed]
- Zhu Y, Liang M, Wu W, et al. Preliminary results of single-port vs. triple-port complete thoracoscopic lobectomy for non-small cell lung cancer. Ann Transl Med 2015;3:92. [PubMed]
- Jutley RS, Khalil MW, Rocco G. Uniportal vs standard three-port VATS technique for spontaneous pneumothorax: comparison of post-operative pain and residual paraesthesia. Eur J Cardiothorac Surg 2005;28:43-6. [Crossref] [PubMed]
- Tamura M, Shimizu Y, Hashizume Y. Pain following thoracoscopic surgery: retrospective analysis between single-incision and three-port video-assisted thoracoscopic surgery. J Cardiothorac Surg 2013;8:153. [Crossref] [PubMed]
- Gonzalez-Rivas D, Yang Y, Ng C. Advances in Uniportal Video-Assisted Thoracoscopic Surgery: Pushing the Envelope. Thorac Surg Clin 2016;26:187-201. [Crossref] [PubMed]
- Yim AP. VATS major pulmonary resection revisited - controversies, techniques, and results. Ann Thorac Surg 2002;74:615-23. [Crossref] [PubMed]
- McKenna RJ Jr, Houck W, Fuller CB. Video-assisted thoracic surgery lobectomy: experience with 1,100 cases. Ann Thorac Surg 2006;81:421-5; discussion 425-6. [Crossref] [PubMed]
- Gonzalez D, Paradela M, Garcia J, et al. Single-port video-assisted thoracoscopic lobectomy. Interact Cardiovasc Thorac Surg 2011;12:514-5. [Crossref] [PubMed]
- Huang J, Li J, Qiu Y, et al. Thoracoscopic double sleeve lobectomy in 13 patients: a series report from multi-centers. J Thorac Dis 2015;7:834-42. [PubMed]
- Gonzalez-Rivas D. VATS Lobectomy: Surgical Evolution from Conventional VATS to Uniportal Approach. ScientificWorldJournal 2012;2012:780842.
- Seder CW, Hanna K, Lucia V, et al. The safe transition from open to thoracoscopic lobectomy: a 5-year experience. Ann Thorac Surg 2009;88:216-25; discussion 225-6. [Crossref] [PubMed]
- French DG, Thompson C, Gilbert S. Transition from multiple port to single port video-assisted thoracoscopic pulmonary resection: early experience and comparison of perioperative outcomes. Ann Cardiothorac Surg 2016;5:92-9. [Crossref] [PubMed]
- Drevet G, Figueroa PU. Uniportal video-assisted thoracoscopic surgery: safety, efficacy and learning curve during the first 250 cases in Quebec, Canada. Ann Cardiothorac Surg 2016;5:100-6. [Crossref] [PubMed]
- Wang BY, Tu CC, Liu CY, et al. Single-Incision Thoracoscopic Lobectomy and Segmentectomy With Radical Lymph Node Dissection. Ann Thorac Surg 2013;96:977-82. [Crossref] [PubMed]
- Chung JH, Choi YS, Cho JH, et al. Uniportal video-assisted thoracoscopic lobectomy: an alternative to conventional thoracoscopic lobectomy in lung cancer surgery? Interact Cardiovasc Thorac Surg 2015;20:813-9. [Crossref] [PubMed]
- Gonzalez-Rivas D, Paradela M, Fernandez R, et al. Uniportal Video-Assisted Thoracoscopic Lobectomy: Two Years of Experience. Ann Thorac Surg 2013;95:426-32. [Crossref] [PubMed]
- Harris CG, James RS, Tian DH, et al. Systematic review and meta-analysis of uniportal vs. multiportal video-assisted thoracoscopic lobectomy for lung cancer. Ann Cardiothorac Surg 2016;5:76-84. [Crossref] [PubMed]
- Tam JK, Lim KS. Total muscle-sparing uniportal video-assisted thoracoscopic surgery lobectomy. Ann Thorac Surg 2013;96:1982-6. [Crossref] [PubMed]
Cite this article as: Laisaar T, Kocsis Á, Bagajevas A, Silins I, Batirel H. Transition from two-three port to uniportal approach in video-assisted thoracoscopic surgery lobectomy: a multicentre comparative study. Shanghai Chest 2017;1:52.


