Primary hyperhidrosis: an invalidating disease—patients management and surgical recommendations
Definition
Sweat is produced by eccrine glands present in the whole skin. Its physiological production is determined by emotional and thermic stimuli and mental activity.
Hyperhidrosis is a pathological condition consisting in extreme perspiration exceeding organism thermoregulation within a physiological range. It is not an eccrine glands disease. Hyperhidrosis is distinguished in primary and secondary. Primary hyperhidrosis (PH) usually affects palms, axillae, face and soles, singularly (focal hyperhidrosis) or together (generalized hyperhidrosis). Palmar hyperhidrosis is probably the most common and disturbing pattern, usually determining severe functional and social disadvantages with a negative impact on quality of life (QoL). HP presents in young people, affecting equally man and women, and interests a percentage ranging from 0.6% to 5% of entire population (1,2).
Etiology
Hyperhidrosis is divided into primary and secondary. Secondary hyperhidrosis is caused by many different underlying health conditions, such as obesity, gout, menopause, tumor, mercury poisoning, diabetes mellitus, or hyperthyroidism. Patients affected by secondary hyperhidrosis are not surgical candidates since hyperhidrosis disappears by treating the specific underlying disease with clinical therapies. Contrary, PH is idiopathic, that is to say “of unknown cause”, and may need surgical management. PH etiology is determined by any changes of the sweating pathway that comprises many neurological structures originating from hypothalamic sympathetic centers and descending through the sudomotor chain to the sweat glands. These changes should determine a huge disproportion between normal triggers and sweating response. Sometimes sweating is not even supported by any stimulus.
Some authors have identified anatomical and physiological characteristics particular to people with PH. A recent interesting review by Hashmonai et al. (3) have investigated and summarized these common characteristics. We briefly resume their findings in the different fields:
- Epidemiology: familial history of HP ranging from 34% to 50% of cases has been observed in many studies;
- Genetics: a disease allele has been identified in 5% of population and it seems to results in hyperhidrosis in 25% of times when present;
- Anatomy: patients affected by HP seem to be characterized by a higher number of ganglion cells and apoptotic cells in the ganglia that result larger in size. Moreover, thicker myelin sheath of HP axons has also been described;
- Pathophysiology and metabolic dysfunctions: neural tissue in HP patients is exposed to an enlarged functional stimulation. Some studies showed a higher expression of acetylcholine receptors and an oxidative damage in the sympathetic ganglia that could be involved in HP development;
- Neurology: PH should not be considered as an over function but rather as a regulatory complex disorder involving the entire autonomic pathway;
- Psychology: personality disorders or even personality traits such as temperament could influence biological mechanisms and be an etiological factor for HP.
Most of these data must be still confirmed by evidence, therefore, HP etiology is still considered unclear.
Clinical signs and diagnostic pathway
HP is characterized by specific findings. First, it is usually localized and bilateral. The areas usually affected by excessive sweating are hands (palms), axillae and foot (plants). Craniofacial hyperhidrosis is also described and sometimes is associated with facial blushing, but is infrequent.
Second, HP onset is in the first decade of life (childhood), especially for palmar hyperhidrosis. Then, during adolescence, symptoms become very annoying and badly impacting QoL. Family history is often positive.
Remarkably, symptoms are not related to atmospheric conditions or, at least, are excessively influenced. On the contrary, physical or emotional inputs significantly boost the sweating. Lastly, sweating never occurs during sleeping.
Therefore, diagnosis can be easily obtained by careful recording of patient clinical history and by routine clinical evaluation (assessment of the sweat stains of clothes or palmar sweating extension). However, despite rarely used; there are some tests to quantitatively asses the rate of excessive sweating. These are the gravimetric measurement, the vaporimetry, the Minor test and the use of a QoL and impairment of daily activities measurement (4).
Once excessive sweating has been found and diagnosis of HP is suspected, secondary hyperhidrosis must be excluded discarding clinical manifestations of possible underlying diseases. Apart of clinical and pharmacological history, the following tests should be always performed: thyroid function test, metabolic panel, 24-hour urine collection for catecholamines, metanephrines and normetanephrines, serum free metanephrines and normetanephrines, urine 5-hydroxyndolacetic acid.
Treatments
Several treatments for HP have been proposed and many of them are available in the most of countries. The main distinction is between surgical and non-surgical options. Non-surgical treatments are topical antiperspirants, iontophoresis and systemic medication, whereas surgical treatments are endoscopic thoracic sympathectomy (ETS) and excision of axillary tissue. Lastly, botulinum toxin injection it’s a “bridge” option between medical and surgical approach.
These options diverge by satisfaction rate, efficacy duration and collateral effects onset for each of the different anatomic affected areas.
Medical treatments
Medical treatments are several, ranging from topic to systemic approach with different characteristics. However, all medical treatments are unfortunately characterized by a common undesired feature: the expiration of their effects. Therefore, they have a palliative action on excessive sweating and every relief disappears as soon as therapy is stopped.
We just list current medical treatments with a summary of their results and side effects:
- Antiperspirants are the most diffuse topical treatments. Among these, aluminium salt solutions are the most successful. Aluminium chloride hexahydrate is cheap and non-toxic. It acts causing an obstruction of the distal sweat gland ducts. However, glands return with epidermal renewal. Antiperspirants are mostly effective for axillary hyperhidrosis, whereas in palmar hyperhidrosis efficacy is lower and higher concentrations are required. Side effects of aluminium chloride treatment are itching and stinging immediately after application and skin irritation, moreover sweating symptoms relief is rarely long-lasting (5);
- Systemic treatments are useful for diffuse or multifocal hyperhidrosis. Unfortunately, many of these drugs have not been controlled by clinical trials or have not been approved in many countries. Moreover, side effects are very annoying therefore their use is often limited to brief periods or specific events (wedding, speech, exams, etc.);
- Botulinum Toxic A: botulinum injection is a successful non-medical, minimal invasive treatment adopted for hyperhidrosis in all of the body areas affected. It is usually recommended in patients non responsive to medical treatments that prefer not to undergo straightly to surgery. It consists of Botulinum toxin A injections (Botox) and guarantees good control of excessive sweating. Botox has been shown to result in an 82–87% decrease in palmar or axillary sweating. Results are noticed about 2 to 4 days after treatment with the full results within 2 weeks. Unfortunately, it is afflicted by some disadvantages such as the need of many painful injections, high cost and above all the short lasting effect requiring new treatments every about 6 months (6);
- Iontophoresis is performed using a medical device to pass a mild electrical current through water (usually using shallow pans for hands or feet or specific pads for other body areas) and through the skin’s surface. It is particularly successful in hands and foot hyperhidrosis, with success rate ranging between 81% and 91% of cases. However, effects end in about 7 days; therefore the procedure should be repeated every week. No significant collateral effects are reported (7).
Surgical treatments
Surgery for hyperhidrosis is represented by ETS and underarms surgery.
Underarms surgery consists of sweat glands excision or curettage or liposuction with the aim to remove or reduce the number of glands so that they can no longer produce perspiration. It is specific for axillary hyperhidrosis. Its advantages are the absence of compensatory sweating and that is an awake office procedure. That should be always underlined that completed excision of underarm tissue containing sweating glands is not recommended because associated with serious complication of shoulder movements due to scary tissue. Curettage and liposuction usually obtain satisfying sweating reduction in 40–60% of cases. These techniques are barely widespread. On the contrary, ETS is the most diffuse and effective surgical approach for PH.
ETS
ETS consists of single or multiple surgical interruptions of sympathetic chain. This operation is usually called sympathectomy. Sympathectomy means, word for word, the interruption of the trunk by removal of a segment with a ganglia. This technique was diffuse at the time of thoracotomy surgery but it was time-consuming and, above all, invasive and dangerous. Nowadays, during video-assisted thoracic surgery (VATS) era, the removal of part of the trunk is rare but the name sympathectomy has remained worldwide. Today, trunk interruption is often obtained just with its simple transection. It is called sympathicotomy or sympathotomy.
Both sympathectomy and sympathicotomy are irreversible since the nerve trunk has been transected. If nerve interruption has been done without transection but by clipping, its integrity is preserved and therefore nerve impotence could be theoretically reversible. This could be an advantage in case of patients’ regrets from surgery, for example in case of excessive compensatory sweating. This kind of surgery is called endoscopic sympathetic block.
Patients selection
Good patients selection is the key for successful surgery also in ETS. Therefore, once diagnosis of HP has been done, surgery should be proposed based on some simple but essential mental and physical traits criteria.
First of all, since HP is a benign disorder not threatening to the lives of patients, we think that surgery should be referred only to adult people. The main reason is that patients must be able to seriously asses their discomfort and the impairment on QoL. Therefore, child should be excluded from ETS.
At the same way, patients should be well conscious of possible side effects associated with ETS, in particular compensatory sweating or compensatory hyperhidrosis (CH). It is recommended that patient decide for surgery only if highly motivated to defeat palmar, axillae or facial HP despite the risk of undesired effects.
Physical traits are important as well. Partial contraindications are past pneumonia, tuberculosis, pneumothorax (PNX), pleural effusion, thoracic surgery and all conditions predisposing adhesions. Pleurodesis could make thoracoscopy difficult, indeed. Lastly, absolute contraindications are obesity [desired body mass index (BMI) is <28], bradycardia (resting heart rate 55 beats per minute), neurologic and psychiatric diseases.
Preparation to surgery
Since these patients are usually in good general conditions, preparations are simple. It consists of basic blood exams, electrocardiography (ECG) and chest X-ray.
Surgical anatomy
Sympathetic chain appears like a white cord running beneath parietal pleura along the column. It crosses the ribs at the level of their neck before the vertebrae articulation. Usually it is easily recognizable, even in fatty people.
To distinguish a specific zone of the chain, the landmark established by Society of Thoracic Surgeons (STS) is the underlying rib; ribs are very easily recognizable. Therefore, each given chain level is named using the capitol letter “R” and the corresponding rib number (example: R2). Instead, ganglia as represented by the capitol letter G and usually are located at the intercostal space of every corresponding rib. For example, G3 is at the lower edge of the third rib, in front of the third intercostal space. However, it is useful to remind that descending the column; ganglia are a little bit more distant from the superior rib edge.
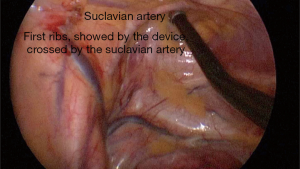
The best way to identify a specific rib and its corresponding trunk level is to count the ribs descending from the first one. First rib is recognizable since it is C-shaped, cranially positioned and very close to the pulsating subclavian artery. Remarkably, first rib is strictly closed to G1, a very crucial ganglion, difficult to identify and absolutely to be preserved.
Once a target level of the nerve trunk has been recognized, it is mandatory to find and preserve the neurovascular bundle under the lower rib edge and the other next vascular structure such as the superior vena cave or the aorta.
Lastly, Kuntz nerves are small fibers arising from the main trunk at every level and going to the sweating glands. Their anatomical route is variable however they usually pass 2 cm laterally from the sympathetic chain on the inner face of the rib leaning against the periosteum. These fibres are important since represent an alternative pathway that could determine persisting HP after ETS.
Peri-operative management
As concerns patient position during surgery, the main point to be addressed is the best way to perform surgery bilaterally. Therefore, patients are positioned in a semi-fowler position: dorsal decubitus and arms abducted at 90° (Figure 1). Patients should be secured on the bed avoiding slipping down. Then, the bed can be rotated during surgery to improve the mediastinum exposition.
Usually patients are intubated in general anaesthesia. Normal or double-lumen endotracheal tubes are available. Double-lumen tube guarantees an alternate selected ventilation of the contralateral lung. We usually prefer this technique. Otherwise, if normal tube is used, CO2 induced PNX or brief period of apnea are needed (8). CO2 insufflation, 10 mmHg maximum, it’s usually preferred in case of micro-surgery, when 2–3 mm instruments are used.
Surgical technique
Thoracic sympathetic trunk interruption is usually performed bilaterally for focal or generalized HP interesting palms, axillae or face. If no contraindications are present, the dominant side is treated first, in order to guarantee a significant result also in case of unexpected complication determining surgery abortion. Therefore, the right side is usually the first to be approached, except for left-handed cases.
Minimally invasive surgery is the routine gold-standard, but many different thoracoscopic approaches have been described.
The most common is the two-port VATS (9). Two 5-mm ports are placed at the anterior and middle axillary line at V and III intercostal space. Cosmetic motivations suggest using the mammary sulcus or areola to better cover scares. Anyway, port position can slightly change according to patient chest conformation or surgeon’s custom.
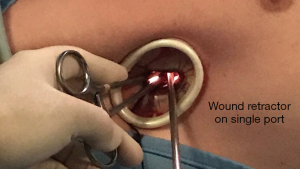
Uniportal VATS advent has been welcomed also for ETS. A 2 cm single port in the axillary fossa allows to enter the chest cavity with the camera (5 or 10 mm) and one or two endoscopic instruments (10) (Figures 2,3).
Once entered the pleural cavity, surgeon move and push down the lung to expose superior mediastinum, posterior chest wall and the spine. This step, except in case of adhesions, is simple and allows identifying the sympathetic trunk in front at the camera.
Once the chain has been recognized, the second step provides for the ribs count starting from the first one and descending along the columns. The first rib is recognizable due to its C-shape and proximity to subclavian artery (Figure 4). We usually mark each ribs at the periosteum with a thin cauterization descending from the second to the target rib. This simple trick allows saving time avoiding ribs re-count.
Once the target rib and the corresponding sympathetic chain level have been marked, nerve trunk interruption can be performed. It is obtained by nerve transection using electro cautery or harmonic scalpel.
Harmonic scalpel offers some advantages such as cut and coagulation with lower spread of heat. This is useful and safe since reduces smoke in the pleural cavity and thermal damage of intercostal vessels and next ganglia risk (especially for high transection close to the first ganglion).
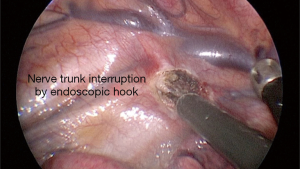
Anyway, we are comfortable with hook electro cautery because its particular shape allows isolating, picking up and cutting the chain without introduction of any other device (Figure 5). In case of sympathectomy, a double nerve transection is performed, including the corresponding ganglia. Then, the isolated specimen is removed with an endoscopic forceps.
To complete nerve interruption, Kuntz branches should be also cut off. Since these fibres are hardly identifiable, their resection is “blindly” obtained by parietal pleura cauterization, till periosteum, of the corresponding rib at 1–2 cm from the sympathetic chain.
Nerve trunk interruption is performed at a given level according to surgical strategy preoperatively established. Nerve interruptions can be multiple.
After review of the haemostasis and air leaks, a chest tube connected to water-seal level is introduced in each pleural cavity thorough the camera port in order to remove PNX. Chest tube could be removed just at the end of surgery, as soon as air leaks stop.
Complications
ETS is associated with minimal trauma and very low mortality; main series in literature report absence of mortality and an incidence of surgical complications ranging between 1–2% (11). Therefore, it is without fail a safe procedure. Concerning morbidity, bradycardia and Horner’s syndrome are the only two complications characteristics for ETS. Bradycardia is due to nerve interruption itself and is usually clinically irrelevant except for some categories such as professional athletes. It emerges as soon as the nerve is interrupted. Therefore, we suggest paying specific attention to cardiac rhythm as soon as the nerve has been resected and eventually interrupt surgery of the opposite side.
Horner’s syndrome is due to G1 damage. This complication is often due to a mistaken high nerve interruption. However, advent of harmonic scalpel and surgeon’s desertion of G2 resection make this complication rare.
Except for these two specific complications, other events are rare and obvious for every kind of thoracic surgery. They are lung injury, PNX, bleeding, chylothorax and phrenic nerve injury. These are often registered in case of stuck lung for pleural adhesion and consists of prolonged air-leak or bleeding. They are usually easily managed by chest tube delayed removal.
Postoperative pain is compliant with every VATS procedure lasting about 20/30 minutes. Despite bilateral approach, pain is well dominated.
Persistence of symptoms is not a true complication and should be ascribed to incorrect nerve interruption.
CH and complete dryness
CH is excessive sweating emerging in a new body area after ETS and usually affecting thorax, back or thighs. CH is an undesirable effect of sympathectomy rather than a complication. However, CH sometimes greatly affects patient’s QoL.
CH has a wide range of severity and its discomfort is subjective, therefore a clear diagnosis is hardly to be obtained. This could be one of the reasons why CH incidence varies from 3% to 98% in literature. Usually CH is classified in mild, moderate and severe (12). Unfortunately, severe CH can be embarrassing and QoL compromising such as former HP that required surgery.
Despite CH onset is unpredictable, some factors seems to be more likely responsible. These are obesity, cephalic nerve trunk interruption and numbers of interruptions. CH should be determined by sort of disturbance in the sympathetic system after surgical denervation. It has been suggested (13) that the interruption of the nerve reflex arch between the sympathetic trunk and hypothalamus was the main CH cause. From theory to practice, the more interruption level is high, the more CH risk is increased since that should preserve the negative afferent tone to hypothalamus itself (14).
Therefore, the best CH prevention is based on correct patients selection and meticulous nerve interruption level choice (see next paragraph).
Unfortunately, both surgical (clip removal or nerve reconstruction) and medical approach (diet, breathable clothes, antiperspirants, anticholinergic) to CH are unsuccessful. Therefore, patients must be warned with great care before ETS and made conscious of this risk. In our experience CH is better tolerated in patients who are suffered of severe palmar and axillary HP, since they experienced thorax or back excessive sweating less invalidating.
On the other side, complete dryness of the target body area is another side effect of ETS, considered and felt as an overdone result. CH and dryness degrees are inversely conditioned by denervation level.
Lastly, gustatory sweating is a rare side effect reported in some papers (15). If presents, it is usually experienced after eating spicy or acid foods. It is linked to denervation level too, with higher risk associated to R2 interruption.
Results
ETS main goal is excessive sweating of the target body area remission. This result, once reached, is noticed just at patient’s awakening and stabilizes in the first 30 postoperative days.
Many tests have been suggested to intra-operatively determine sympathectomy efficacy. In our experience, according with Jeng and co-workers (4), the pulse oximetry-derived perfusion index (PI) increasing was a good predictor of successful sympathectomy during ETS. Early and long terms outcomes measurements confirm that QoL improvement is immediate and last unchanged at 10 years as well.
ETS success rate is influenced by PH localization of symptoms and surgical technique adopted. For example, palmar PH management is more successful than cranium-facial indeed. As concerning surgery, nerve interruption level (or levels) is probably the main factor determining outcomes, in terms of both sweating remission and CH onset. Therefore, surgical strategy is based on the statements that high level and multiple nerve trunk interruption more likely determine dry skin whereas low interruption avoid CH onset (16).
Some series have been published in the last decade reporting ETS success rate for different location of symptoms based on nerve interruption level. At the same time CH onset rate was reported for each group.
These studies are hardly comparable since data are not uniform. Different Authors adopted different denervation level and technique (transection or clipping) obtaining different results. However, in 2011 the STS edited an expert consensus for surgical management of HP reporting some recommendations, based on patient’s distribution of sweating, about the level where to interrupt the sympathetic chain to obtain the best outcomes in terms of excessive sweating decrease and CH onset and intensity management (17).
In our experience, the best way to determine optimal denervation level is to comprehensively inform patients about ETS benefits and risks at preoperative time and let them follow their personal wish, balancing complete sweating reduction advantage and possible CH disadvantage. Then denervation will be performed at a higher or lower level based on who are willing to accept a higher risk of CH because they want complete dryness, or not. Once again, patients should be counselled about techniques and results differences and participate in the decision-making process.
Palmar hyperhidrosis. The most curative approach consists of two chain interruptions at R3 and R4. This approach guarantees dry hands inmate than 95% of cases but high risk of CH are present. As an alternative, R4 alone interruption may be acceptable for moderate PH because it limits CH risk and severity, although it may lead to moister hands. At the same time, R3 sympathectomy alone is recommended for patients with severe isolated palmar hyperhidrosis (18,19).
Patients with palmar and plantar hyperhidrosis represent a different challenge. Again, two operations can be performed. An R4 interruption alone may reduce the incidence of CH; alternatively, an R4 and R5 intervention is a reasonable option, but leads to drier feet.
Axillary hyperhidrosis. ETS for axillary hyperhidrosis is often less successful and has higher “regret rates” than for palmar hyperhidrosis. Therefore, before to suggest surgery, others approaches should be suggested or should have been already considered. Based on literature and our experience, for patients who have palmar-axillary, palmar-axillary-plantar, or pure axillary hyperhidrosis, an R4 and R5 transection is suggested. Success is reached in 70–90% of cases (19). R5 interruption alone avoids CH but do not guarantees excessive sweating successful management (20).
Craniofacial hyperhidrosis. Patients with cranial and facial sweating present a more complicated problem compared with patients affected by palmar or axillary hyperhidrosis. Successful rate is lower (60–80%) on complications rate higher (19). Patients should be always warned about CH high risk. Based on results of many series, R3 alone interruption is the best option, because it reduces the risk of CH and the risk of Horner’s when compared with R2 or an R2 and R3 transection. Surgical failure is rare and due to incorrect nerve trunk identification (21).
Conclusions
Excessive sweating is a serious medical condition that can be embarrassing, uncomfortable, anxiety-inducing, dangerous, and disabling. PH is idiopathic, whereas secondary hyperhidrosis is symptom of different underlying diseases.
There are many and different treatments for HP. Each therapy is characterized by benefits and undesired effects. Therapy efficacy is conditioned by PH severity and, over all, by sweating localization.
Usually, non-invasive treatments should be the first modalities of treatment. Correct medical treatment is decided case by case based on PH severity, localization and patient’s requirements.
In case of failure, surgery should be proposed. ETS is the most diffuse and effective surgical treatment. It is safe and successful but characterized by an undesired effect called CH. ETS efficacy and CH risk depend on sympathetic chain interruption level. Therefore, target level and numbers of interruption should be always decided weighting benefits and side effects in accordance with patient will.
To summarize, lower level and single interruption limit CH risk in every PH localization. However, in case of severe patient discomfort, cephalic or multiple interruptions should be considered if patient ask for satisfying dryness.
Acknowledgments
Funding: None.
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/shc.2018.04.05). FR serves as an unpaid editorial board member of Shanghai Chest from Jan 2018 to Dec 2019. MS serves as an unpaid Associate Editor of Shanghai Chest. The other authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Moraites E, Vaughn OA, Hill S. Incidence and prevalence of hyperhidrosis. Dermatol Clin 2014;32:457-65. [Crossref] [PubMed]
- Estevan FA, Wolosker MB, Wolosker N, et al. Epidemiologic analysis of prevalence of the hyperhidrosis. An Bras Dermatol 2017;92:630-4. [Crossref] [PubMed]
- Hashmonai M, Cameron AEP, Connery CP, et al. The Etiology of Primary Hyperhidrosis: A Systematic Review. Clin Auton Res 2017;27:379-83. [Crossref] [PubMed]
- Jeng EI, Gravenstein N, Klodell CT. Perfusion Index: An Indicator of Success During Endoscopic Thoracic Sympathectomy for Hyperhidrosis. Ann Thorac Surg 2017;104:426-30. [Crossref] [PubMed]
- Mehrotra S, Schmith VD, Dumitrescu TP, et al. Pharmacometrics-guided drug development of antihyperhidrosis agents. J Clin Pharmacol 2015;55:1256-67. [Crossref] [PubMed]
- He J, Wang T, Dong J. Effectiveness of botulinum toxin A injection for the treatment of secondary axillary bromhidrosis. J Plast Reconstr Aesthet Surg 2017;70:1641-5. [Crossref] [PubMed]
- Kim DH, Kim TH, Lee SH, et al. Treatment of Palmar Hyperhidrosis with Tap Water Iontophoresis: A Randomized, Sham-Controlled, Single-Blind, and Parallel-Designed Clinical Trial. Ann Dermatol 2017;29:728-34. [Crossref] [PubMed]
- Kaplan T, Ekmekçi P, Koçer B, et al. Bilateral sympathicotomy for hyperhidrosis without using single-lung ventilation. Turk J Med Sci 2015;45:771-4. [Crossref] [PubMed]
- Han PP, Gottfried ON, Kenny KJ, et al. Biportal thoracoscopic sympathectomy: surgical techniques and clinical results for the treatment of hyperhidrosis. Neurosurgery 2002;50:306-11; discussion 311-2. [PubMed]
- Rocco G. Endoscopic VATS sympathectomy: the uniportal technique. Multimed Man Cardiothorac Surg 2007;2007:MMCTS.2004.000323.
- de Andrade Filho LO, Kuzniec S, Wolosker N, et al. Technical difficulties and complications of sympathectomy in the treatment of hyperhidrosis: an analysis of 1731 cases. Ann Vasc Surg 2013;27:447-53. [Crossref] [PubMed]
- Dobosz L, Cwalina N, Stefaniak T. Influence of Body Mass Index on Compensatory Sweating in Patients after Thoracic Sympathectomy due to Palmar Hyperhidrosis. Thorac Cardiovasc Surg 2017;65:497-502. [Crossref] [PubMed]
- Cheng A, Johnsen H, Chang MY. Patient Satisfaction after Thoracoscopic Sympathectomy for Palmar Hyperhidrosis: Do Method and Level Matter? Perm J 2015;19:29-31. [PubMed]
- Lin CC, Telaranta T. Lin-Telaranta classification: the importance of different procedures for different indications in sympathetic surgery. Ann Chir Gynaecol 2001;90:161-6. [PubMed]
- Reisfeld R, Nguyen R, Pnini A. Endoscopic thoracic sympathectomy for hyperhidrosis: experience with both cauterization and clamping methods. Surg Laparosc Endosc Percutan Tech 2002;12:255-67. [Crossref] [PubMed]
- Sang HW, Li GL, Xiong P, et al. Optimal targeting of sympathetic chain levels for treatment of palmar hyperhidrosis: an updated systematic review. Surg Endosc 2017;31:4357-69. [Crossref] [PubMed]
- Cerfolio RJ, De Campos JR, Bryant AS, et al. The Society of Thoracic Surgeons expert consensus for the surgical treatment of hyperhidrosis. Ann Thorac Surg 2011;91:1642-8. [Crossref] [PubMed]
- Zhang W, Wei Y, Jiang H, et al. T3 versus T4 thoracoscopic sympathectomy for palmar hyperhidrosis: a meta-analysis and systematic review. J Surg Res 2017;218:124-31. [Crossref] [PubMed]
- Sternbach JM, DeCamp MM. Targeting the Sympathetic Chain for Primary Hyperhidrosis: An Evidence-Based Review. Thorac Surg Clin 2016;26:407-20. [Crossref] [PubMed]
- Sammons JE, Khachemoune A. Axillary hyperhidrosis: a focused review. J Dermatolog Treat 2017;28:582-90. [Crossref] [PubMed]
- Fukuda JM, Varella AYM, Teivelis MP, et al. Video-Assisted Thoracoscopic Sympathectomy for Facial Hyperhidrosis: The Influence of the Main Site of Complaint. Ann Vasc Surg 2018;46:337-44. [Crossref] [PubMed]
Cite this article as: Raveglia F, Rizzi A, Scarci M, Angeli MC, Baisi A. Primary hyperhidrosis: an invalidating disease—patients management and surgical recommendations. Shanghai Chest 2018;2:34.