
ERAS prior to minimally invasive esophagectomy
Enhanced recovery after surgery (ERAS) was first proposed and practiced by the Danish surgeon Kehlet in 1997 (1,2). As a new concept and therapeutic rehabilitation model, ERAS refers to the application of a series of optimization measures with evidence-based medical indications during the perioperative period. These measures are intended to reduce the physiological and psychological traumatic stress in patients who undergo surgery and to accelerate rehabilitation. The benefits of the ERAS concept are reflected in the following: (I) improvement in the physical and psychological efficacy of the treatment; (II) reduction in postoperative complications; (III) acceleration of rehabilitation; (IV) shortening of the hospital stay; (V) reduction in medical expenses; (VI) reduction in social and family burdens. To date, ERAS has been successfully applied in surgeries for colorectal surgery (3-5). Moreover, several large esophageal cancer centers in China and other countries have also gradually applied the ERAS to esophagectomy (6-10). Currently, minimally invasive esophagectomy (MIE), which is represented by thoracoscopic laparoscopic esophagectomy (TLE), has been widely used in clinical practice. In addition, robotic assisted minimally invasive esophagectomy (RAMIE) has also been gradually introduced and performed to further optimize the minimally invasive surgical approach of MIE. It is believed that in the near future, the combination of ERAS and MIE will greatly reduce the occurrence of surgical trauma and accelerate the rehabilitation of patients after esophagectomy.
Section I: preoperative considerations of ERAS for esophagectomy
For esophagectomy, perioperative ERAS mainly focuses on the preoperative, intraoperative and postoperative periods. This study uses MIE as an example to describe the details of the preoperative preparation and the features that are assessed in perioperative MIE-ERAS, as described below.
Preoperative education
Enhanced preoperative evaluation for patients, which includes an assessment of the surgical risk and tolerability, is conducive to postoperative rehabilitation. Preoperative education is a non-independent predictor of the successful implementation of accelerated rehabilitation (11,12). Preoperative education should focus on the introduction of the treatment process and surgical plan to facilitate cooperation among patients with respect to postoperative rehabilitation and the development of an early discharge plan. The patients should be informed of their important role in this plan, including in postoperative posture, early nasogastric enteral nutrition, early ambulation, postoperative feeding methods, and for patients with neck anastomosis, the precautions of applying pressure on the neck incisions during cough and expectoration.
Preoperative nutrition and other risk assessment
Patients with esophageal cancer often experience concomitant preoperative malnutrition due to the limited food intake and tumor depletion, which may directly affect postoperative recovery. Studies have shown that preoperative malnutrition increases the incidence of postoperative complications (13,14). Therefore, patients with severe malnutrition should receive nutritional support therapy, and the operation should be rescheduled. Patients who receive preoperative radical radiochemotherapy, neoadjuvant radiochemotherapy, and those with severe diabetes have an increased risk of postoperative anastomotic leakage. These patients should therefore undergo cautious, accelerated rehabilitation.
Preoperative fasting
As a traditional concept, food intake should be prohibited the night before surgery to reduce the risk of mis-aspiration during anesthesia. However, no evidence supports the idea that long-term fasting before esophagectomy can prevent mis-aspiration. Eating can reduce catabolism, psychological stress and potential insulin resistance. The consumption of liquid foods 6 hours before surgery is safe and can reduce preoperative thirst, hunger and irritability, as well as postoperative muscle loss; this can also reduce the symptoms of nausea and vomiting and can significantly reduce the incidence of postoperative insulin resistance (15). Patients with severe esophageal obstruction should avoid eating 6 hours before surgery to avoid anesthesia-related aspiration.
Preoperative bowel preparation
Preoperative enema may cause stress in the patient and may lead to dehydration and electrolyte imbalances, especially in frail elderly patients. Therefore, preoperative bowel preparation for esophagectomy is only recommended for patients with severe constipation; in these cases, laxatives such as lactulose oral solution and phenolphthalein tablets are recommended.
Preoperative anesthetic medication
Sedative medication given the night before the surgery may help relieve patient stress.
Use of prophylactic antibiotics
Antibiotic prophylaxis is beneficial for the reduction of infection in patients undergoing esophageal cancer surgeries. Antibiotics should be given half an hour before the start of surgery. If the operation time is more than 3 hours, antibiotics can be given again during surgery.
Section II: preoperative clinical approach of MIE-ERAS in the Esophageal Center of Shanghai Chest Hospital
Preoperative education
Psychological guidance
The patients are encouraged to face their own illness with open-mindedness and positivity.
Dietary guidance
The preoperative diet should consist of high-protein and high-calorie foods, which should also be rich in vitamins and low in fiber. Coarse, hard, pickled, and spicy food should be avoided. Alcohol, including beer, rice wine, and liquor is prohibited. Food in liquid form along with post-meal liquid (1% streptomycin) rinsing and administration of metronidazole (one tablet of po bid after a meal) should be provided to the patients with obvious obstructions.
Sanitation guidance
Patients should brush their teeth at least twice a day and rinse with warm boiled water after meals. Patients with oral diseases should be treated promptly.
Preoperative preparation
Respiratory tract preparation
- The patients with a history of smoking should have completely quit smoking for at least 2 weeks and should not smoke during their hospitalization;
- Terbutaline Sulfate Injection 2 & Pulmicort 2 (inhalation bid): Mucosolvan 60 mg (po tid); Theophylline 0.1 g (po Qn)
Cardiopulmonary exercise
- Climbing stairs: the patient is asked to continuously walk upstairs without any break based on the individual’s strength, for 5 floors 3–4 times/day;
- Deep breathing exercises: abdominal breathing, deep breathing, and coughing are performed under the guidance of a doctor 400 times.
Special preoperative preparation
- For patients with hypertension, blood pressure should be monitored daily, and preoperative oral antihypertensive drugs should be administered to maintain a stable blood pressure;
- For patients with diabetes, blood sugar should be tested before each meal and at bedtime to ensure a stable level of preoperative blood glucose;
- For patients whose medical status is complicated by other systemic diseases, experts in the relevant departments should be consulted if necessary;
- All self-administered drugs and supplements (such as aspirin) should be discontinued under the guidance of a physician;
- For patients with severe eating obstructions, severe malnutrition, and those who cannot eat, preoperative nutritional support should be provided (oral ENSURE or parenteral nutrition support);
- For patients with suspected supraclavicular lymphadenopathy, lymph node biopsy should be performed.
Preoperative examination
Examination of cardiopulmonary function
- Blood test: routine blood/urine/fecal tests, liver/kidney function/electrolyte, blood glucose/glycosylated hemoglobin, coagulation function, blood type, hepatitis/syphilis/AIDS;
- Assessment of cardiac function: electrocardiogram, dynamic electrocardiogram (for patients with a history of arrhythmia), treadmill exercise test (for those >60 years of age), heart echocardiography (for patients >60 years of age), coronary angiography (for patients with a history of coronary heart disease);
- Pulmonary function assessment: lung function, blood gas analysis, breath-holding test, and stair climbing test.
Tumor examination
- Blood tumor markers;
- Esophagoscopy/EUS: biopsy;
- Gastrointestinal (GI) tumors: general classification and location of tumors;
- Neck ultrasound, chest-enhanced CT, abdomen-enhanced CT, PET-CT (selective);
Staging assessment and therapeutic strategies
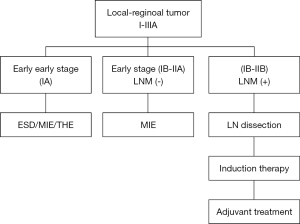
According to the preoperative examination, a cTNM staging assessment was performed, and a treatment plan was individually developed according to the guidelines for the diagnosis and treatment of esophageal cancer (Figure 1).
Acknowledgments
Funding: None.
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/shc.2018.06.07). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Kehlet H. Multimodal approach to control postoperative pathophysiology and rehabilitation. Br J Anaesth 1997;78:606-17. [Crossref] [PubMed]
- Kehlet H, Wilmore DW. Multimodal strategies to improve surgical outcome. Am J Surg 2002;183:630-41. [Crossref] [PubMed]
- Basse L, Hjort Jakobsen D, Billesbølle P, et al. A clinical pathway to accelerate recovery after colonic resection. Ann Surg 2000;232:51-7. [Crossref] [PubMed]
- Basse L, Jacobsen DH, Billesbølle P, et al. Colostomy closure after Hartmann's procedure with fast-track rehabilitation. Dis Colon Rectum 2002;45:1661-4. [Crossref] [PubMed]
- Basse L, Jakobsen DH, Bardram L, et al. Functional recovery after open versus laparoscopic colonic resection: a randomized, blinded study. Ann Surg 2005;241:416-23. [Crossref] [PubMed]
- Sun HB, Liu XB, Zhang RX, et al. Early oral feeding following thoracolaparoscopic oesophagectomy for oesophageal cancer. Eur J Cardiothorac Surg 2015;47:227-33. [Crossref] [PubMed]
- Shewale JB, Correa AM, Baker CM, et al. Impact of a Fast-track Esophagectomy Protocol on Esophageal Cancer Patient Outcomes and Hospital Charges. Ann Surg 2015;261:1114-23. [Crossref] [PubMed]
- Zhao G, Cao S, Cui J. Fast-track surgery improves postoperative clinical recovery and reduces postoperative insulin resistance after esophagectomy for esophageal cancer. Support Care Cancer 2014;22:351-8. [Crossref] [PubMed]
- Cao S, Zhao G, Cui J, et al. Fast-track rehabilitation program and conventional care after esophagectomy: a retrospective controlled cohort study. Support Care Cancer 2013;21:707-14. [Crossref] [PubMed]
- Pan H, Hu X, Yu Z, et al. Use of a fast-track surgery protocol on patients undergoing minimally invasive oesophagectomy: preliminary results. Interact Cardiovasc Thorac Surg 2014;19:441-7. [Crossref] [PubMed]
- Aarts MA, Okrainec A, Glicksman A, et al. Adoption of enhanced recovery after surgery (ERAS) strategies for colorectal surgery at academic teaching hospitals and impact on total length of hospital stay. Surg Endosc 2012;26:442-50. [Crossref] [PubMed]
- Younis J, Salerno G, Fanto D, et al. Focused preoperative patient stoma education, prior to ileostomy formation after anterior resection, contributes to a reduction in delayed discharge within the enhanced recovery programme. Int J Colorectal Dis 2012;27:43-7. [Crossref] [PubMed]
- Kunisaki C, Shimada H, Nomura M, et al. Immunonutrition risk factors of respiratory complications after esophagectomy. Nutrition 2004;20:364-7. [Crossref] [PubMed]
- Nozoe T, Kimura Y, Ishida M, et al. Correlation of pre-operative nutritional condition with post-operative complications in surgical treatment for oesophageal carcinoma. Eur J Surg Oncol 2002;28:396-400. [Crossref] [PubMed]
- Brady M, Kinn S, Stuart P. Preoperative fasting for adults to prevent perioperative complications. Cochrane Database Syst Rev 2003;CD004423 [PubMed]
Cite this article as: Guo X, Ding C, Luo C, Yang Y, Li B, Hua R, Ye B, Gu H, Sun Y, Mao T, Li Z. ERAS prior to minimally invasive esophagectomy. Shanghai Chest 2018;2:50.


