
Life-threatening central air-way obstruction caused by misdiagnosed migration of silicone tracheal stent
Introduction
Insertion of silicone stent is a palliative treatment of airway stenosis in patients unfit for surgery (1). Follow up is mandatory for a prompt diagnosis and treatment of complications related to stent insertion (2). Herein, we reported a case of dislocated stent that remained undiagnosed 15 years after the insertion and caused a life-threatening obstruction of central air-way (carina, left and right main bronchus).
Case presentation
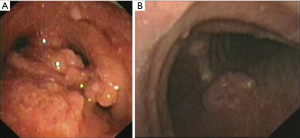
A 85-year old man was referred to our attention for the management of severe respiratory failure. He underwent 15 years before endoscopic dilation and Dumon stent insertion for the management of post-intubation tracheal stenosis; then, he was lost in the follow up. In the last five years, patient experienced recurrent episodes of pneumonia, treated with medical therapy until the last year, when a progressive increase of dyspnea was observed. The subsequent development of severe respiratory failure needed the emergent recovery at local hospital. A chest CT scan was performed, showing migrated Dumon stent that obstructed central airway. Patient underwent an emergent extraction of the stent through rigid bronchoscope (Figure 1). The lack of the elasticity of silicone stent and the presence of tenacious adhesions made particularly challenging this procedure (Figure 2). Following, granulomas were resected with laser to reassure air-way patency. Dyspnea immediately disappeared and improvement of clinical condition was obtained. Endoscopy check performed three months later showed normal patency of central airway with no recurrence of stenosis (Figure 3). At last follow-up, the patient was in good clinical condition with normal air-way patency.


Discussion
Insertion of silicone stent is a palliative treatment to maintain air-way patency after endoscopic dilation of benign tracheal stenosis. Migration, plugging, and granulations are complications related to stent insertion (2,4-6) that can cause life-threatening air-way obstruction if they are misdiagnosed and not promptly treated, as in present case. The dislocation of Dumon stent remained undiagnosed for several years. Despite stent is a temporary treatment of benign airway stenosis and it should be removed 1–2 years after insertion, in this case the stent remained in site for 15 years. The patient lived in a rural country, distant more than 200 km from threatening centers and he did not perform any control after endoscopic treatment. Yet, the recurrent episodes of pneumonia did not let the family doctor to plan additional exams to check the stent position. The dislocated stent at level of carina favored the progressive formation of granulomas that additionally obstructed central airway. The emergent extraction of the stent and the resection of granulomas resolved the life-threatening obstruction. Despite the extraction of stent is generally a simple procedure, in this case it was particularly challenging. In fact, the lack of elasticity of silicone did not allow to easily turn the stent on its position after that its proximal edge was grabbed by the rigid forceps. Yet, tenacious adhesions firmly fixed the stent to the airway, making difficult the extraction.
The present paper showed that stent complications can occur also several years from insertion. Because the patient often back under the care of their family doctor and endoscopic treatment of tracheal stenosis is performed in tertiary center, establishing a link with minor hospitals should be encouraged to allow the early transfer of the patient to the threatening expert center for prompt diagnosis and treatment of complications.
Acknowledgments
Funding: None.
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/shc.2018.07.05). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Wood DE. Airway stenting. Chest Surg Clin N Am 2001;11:841-60. [PubMed]
- Fiorelli A, Mazzone S, Mazzone A, et al. The digital AcuBlade laser system to remove huge vocal fold granulations following subglottic airway stent. Interact Cardiovasc Thorac Surg 2013;17:591-3. [Crossref] [PubMed]
- Carlucci A, Messina G, Cascone R, et al. Video showed the main steps of the procedure as the diagnosis of dislocated stent, the extraction through the rigid bronchoscopy, and the endoscopic follow-up. Asvide 2018;5:676. Available online: http://www.asvide.com/article/view/26367
- Tsakiridis K, Darwiche K, Visouli AN, et al. Management of complex benign post-tracheostomy tracheal stenosis with bronchoscopic insertion of silicon tracheal stents, in patients with failed or contraindicated surgical reconstruction of trachea. J Thorac Dis 2012;4:32-40. [PubMed]
- Ko PJ, Liu CY, Wu YC, et al. Granulation formation following tracheal stenosis stenting: influence of stent position. Laryngoscope 2009;119:2331-6. [Crossref] [PubMed]
- Mitsuoka M, Sakuragi T, Itoh T. Clinical benefits and complications of Dumon stent insertion for the treatment of severe central airway stenosis or airway fistula. Gen Thorac Cardiovasc Surg 2007;55:275-80. [Crossref] [PubMed]
Cite this article as: Carlucci A, Messina G, Cascone R, Ingenito M, Capaccio D, Santini M, Fiorelli A. Life-threatening central air-way obstruction caused by misdiagnosed migration of silicone tracheal stent. Shanghai Chest 2018;2:63.


