
The Minimally Invasive Esophagectomy (MIE) App: a novel teaching tool for minimally invasive esophagectomy
Introduction
Minimally invasive esophagectomy (MIE) is a complex surgical procedure for resection of the esophagus. The technique was initially developed in the early 1990s and was based on the same principles as open esophagectomy (1-3). Since then minimally invasive techniques have been shown to reduce perioperative complications and hospital stay in patients with resectable esophageal disease (4,5). High-volume centres have continued to publish favorable outcomes associated with totally MIE techniques (6-9).
Despite these promising results, widespread acceptance of MIE has remained slow. Mastering the procedure is challenging given its complex nature and relatively low case volumes in many centres. The concept of simulation in surgical education may help to overcome these difficulties by providing opportunities for high-yield experiences which supplement traditional intra-operative learning (10).
Simulation in the form of smart-device applications has previously been validated in other surgical domains (11,12). The goal of this project was to overcome the challenges associated with learning MIE by creating a smartphone- and web-based surgical teaching application. “The MIE App” was designed to systematically teach port placement, instrument utilization, and the dynamics of the procedure—training that is currently only available through specialized fellowships or expensive labs.
Methods
The primary objective of The MIE App’s design was to simplify a highly complex surgical procedure into succinct learning modules and resources. In doing so we hope to expedite operative success by optimizing learning outside of the operating room. We aim to deliver an in-depth learning experience by focusing on three areas:
- An interactive simulation section for improving operative set-up, focusing on strategic port placement, instrument utilization and operative flow;
- A descriptive atlas and surgical videos to provide comprehensive teaching on MIE;
- Self-assessment tool for evaluation of information retention.
A member of the Surrey Thoracic Surgery Group at Surrey Memorial Hospital in Surrey, British Columbia, Canada planned and designed application to teach Ivor-Lewis MIE.
Descriptive atlas
A literature review pertaining to MIE was carried out. A text atlas was compiled to describe the background of the procedure, along with procedural steps to act as a companion to the surgical video and simulation components of the app.
Operative video
Operative videos were captured, with full patient consent, during Ivor-Lewis MIE. All surgery was performed at our institution in Surrey, British Columbia, Canada. The video was edited to illustrate the fundamental steps of the operation.
3-dimensional (3D) modelled simulation
The entire list of specialized tools and instruments involved in Ivor-Lewis MIE was compiled. These apparatuses, including a mannequin model and operating room equipment, were photographed and modelled using industry standard 3D modelling software Maya 3D (Maya 3D, Alias Systems Corporation, Toronto, ON, Canada). The 3D models were then imported and utilized in various components of the App, which was edited, compiled, and built using Unity 3D (Unity Technologies, San Francisco, CA, USA).
App design
The entire MIE procedure was sub-divided into two major sections: the laparoscopic phase and the thoracoscopic phase. These major sections were then further sub-divided into their fundamental steps. The descriptive text atlas, surgical videos and simulation components of the app were designed to review each of these steps. An interactive objective competency assessment tool was developed to test learner’s retention.
Results
The application was designed in Surrey, British Columbia and is compatible with multiple platforms including PC, Mac, Android, and iOS. When the user opens the app, they are presented with three main menu items: Descriptive Atlas, Surgical Video or Simulation (Figure 1). This allows the user to explore various components of the procedure through multiple media platforms (Figure 2).


Descriptive atlas section
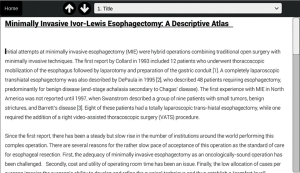
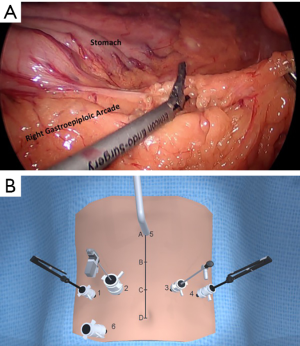
Users begin with the descriptive atlas in which they are presented with a section on the background of Ivor-Lewis MIE (Figure 3). Using the drop-down menu bar or page navigation buttons they can choose to explore various fundamental components of the operation. The text contains embedded intra-operative images as well as corresponding animated still images showing port placement and utilization during each phase. Figure 4 shows an example of this during the laparoscopic phase and Figure 5 shows the thoracoscopic phase.
Surgical video section
The surgical video section allows users to view high-definition intra-operative video. These videos are again organized according to the fundamental steps involved in Ivor-Lewis MIE. Users can play/pause or toggle video content within the app’s build-in media player. The high-definition videos are accompanied by an in-set 3D animation showing which instruments and ports are utilized during each phase. Figure 6 shows a screenshot of surgical video with animation in-set depicting dissection of the hiatus during the laparoscopic phase of the operation.

Simulation section
The simulation section of the app contains the objective assessment tool. This includes a series of evaluations to test content retention of the user. The assessment focuses on text assimilation along with port placement and instrument utilization during each sub-section of the operation. The interactive 3D model allows users to practice the operation stage-by-stage and provides real-time feedback and error count. Figure 7 shows a screenshot of the simulated assessment tool testing the user on stage 1 of the laparoscopic phase: exploration of the gastroesophageal junction. Figure 8 shows and example of the simulation to assess the user’s understanding of stage 1 of the thoracoscopic phase: mobilization of the esophagus.


Validation
Validation of the MIE App remains in the early stages. Implementation has occurred only at the local level within Surrey Memorial Hospital Thoracic Surgery Centre at this time. Trainees rotating through the Thoracic Surgery service as well as multiple visiting Thoracic Surgeons from across Canada have derived measurable benefit from utilizing the application. Plans for formal validation study are currently underway.
Conclusions
Surgeons are under significant pressure to continually improve by delivering better outcomes with less invasive techniques. As procedures improve, their complexity tends increase. This is certainly true of MIE. With the MIE App, challenging multi-cavitary surgery is distilled into manageable modules enabling an out-of-OR learning experience for all components of the procedure. Junior trainees learn the steps of operative progression and eventually can effectively assist in an anticipatory manner. Anxiety-reduction is achieved by permitting thorough review and preparation in non-stressful spaces at home or elsewhere. Fellows and staff surgeons, already facile with esophagectomy, derive important benefit from familiarization with operative set-up; strategic multi-port placement and optimal sequences of dynamic port and instrument utilization. Ideal angles and instrument trajectories are critical for precise dissection and enabling accurate reconstruction. The MIE App versatility is demonstrable with the ability to project the video and port placements on screens in the OR for real-time guidance. Cost savings may be predictable given current hospital resource constraints.
Available videos and other surgical online libraries do not reveal the complete landscape of MIE, tending to leave out influential features of port placement and set up. The MIE App fills a gap between currently available surgical simulation/video education systems by offering a comprehensive, medically-accurate and pragmatic review of MIE through text descriptions, 3D animation and corresponding live surgical video of important surgical maneuvers within the operation. We hope that this application will be widely used by trainees and surgeons to accelerate learning in MIE. The next phase of our work involves a formal validation study of this product.
Acknowledgments
Funding: None.
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/shc.2018.08.03). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). All patient-related media (images and videos) were obtained with written informed consent. Institutional ethical approval was waived.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Swanstrom LL, Hansen P. Laparoscopic total esophagectomy. Arch Surg 1997;132:943-7; discussion 947-9. [Crossref] [PubMed]
- DePaula AL, Hashiba K, Ferreira EA, et al. Laparoscopic transhiatal esophagectomy with esophagogastroplasty. Surg Laparosc Endosc 1995;5:1-5. [PubMed]
- Collard JM, Lengele B, Otte JB, et al. En bloc and standard esophagectomies by thoracoscopy. Ann Thorac Surg 1993;56:675-9. [Crossref] [PubMed]
- Verhage RJ, Hazebroek EJ, Boone J, et al. Minimally invasive surgery compared to open procedures in esophagectomy for cancer: a systematic review of the literature. Minerva Chir 2009;64:135-46. [PubMed]
- Mariette C, Meunier B, Pezet D, et al. Hybrid minimally invasive versus open oesophagectomy for patients with oesophageal cancer: A multicenter, open-label, randomized phase III controlled trial, the MIRO trial. J Clin Oncol 2015;33:5. [Crossref]
- Meng F, Li Y, Ma H, et al. Comparison of outcomes of open and minimally invasive esophagectomy in 183 patients with cancer. J Thorac Dis 2014;6:1218-24. [PubMed]
- Noble F, Kelly JJ, Bailey IS, et al. A prospective comparison of totally minimally invasive versus open Ivor Lewis esophagectomy. Dis Esophagus 2013;26:263-71. [Crossref] [PubMed]
- Zingg U, McQuinn A, DiValentino D, et al. Minimally Invasive Versus Open Esophagectomy for Patients With Esophageal Cancer. Ann Thorac Surg 2009;87:911-9. [Crossref] [PubMed]
- Luketich JD, Pennathur A, Awais O, et al. Outcomes after minimally invasive esophagectomy: review of over 1000 patients. Ann Surg 2012;256:95-103. [Crossref] [PubMed]
- Zevin B, Aggarwal R, Grantcharov TP. Surgical Simulation in 2013: Why Is It Still Not the Standard in Surgical Training? J Am Coll Surg 2014;218:294-301. [Crossref] [PubMed]
- Sugand K, Mawkin M, Gupte C. Training effect of using Touch SurgeryTM for intramedullary femoral nailing. Injury 2016;47:448-52. [Crossref] [PubMed]
- Tulipan J, Miller A, Park AG, et al. Touch Surgery: Analysis and Assessment of Validity of a Hand Surgery Simulation “App”. Hand (N Y) 2018; [Epub ahead of print]. [Crossref] [PubMed]
- Percy ED, Hafizi A, Ojah J, et al. Video demonstration of the MIE App showing all features of this multi-platform application for teaching MIE. Asvide 2018;5:747. Available online: http://www.asvide.com/article/view/27190
Cite this article as: Percy ED, Hafizi A, Ojah J, Sundaresan RS, Ashrafi AS. The Minimally Invasive Esophagectomy (MIE) App: a novel teaching tool for minimally invasive esophagectomy. Shanghai Chest 2018;2:72.


