
Economic assessment in minimally invasive oncological surgery: a high European volume center experience
Introduction
Robotic surgery records very important annual growth rates, especially for certain surgical specialties. Many surgeons indicate the intervention carried out with the help of a ROBOT as preferable with respect to the same intervention carried out with the OPEN methodology or even VATS. The health structures who have to chase an economic balance must clearly understand the differential costs between alternative methods of intervention in order to consciously and more appropriately and ethically choose where to allocate the increasingly limited economic/financial resources (1).
In this article, we analyze the differential costs between three different methods of surgical treatment of lung cancer (NSCLC), traditional open surgery, vats and robotics.
Materials and methods
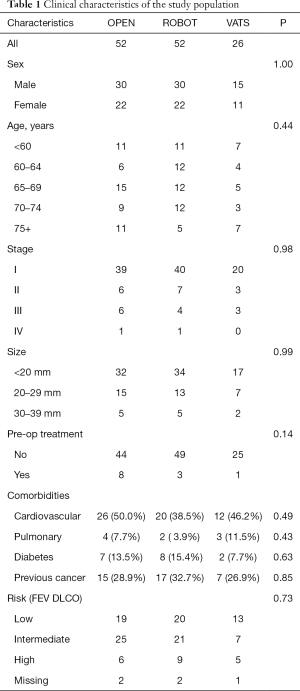
In order to perform an effective comparative analysis, we selected three groups of patients operated on in the period between January 2017 and July 2018 who had the same clinical and pathological characteristics, so that the choice for one method instead of another was not linked to them. The clinical characteristics of the population are reported in Table 1. We selected three groups of patients that were homogeneous by age, sex, tumor stage (TNM classification 8th edition), comorbidity (cardiovascular, pulmonary, diabetes, previous tumor) as well as for the outcome of spirometry (FEV1-DLCO). Furthermore, we have considered only patients whose intervention cost has been supported by the Italian National Health System. For these patients we have found the costs incurred by the Institute and which are partly linked to the recorded purchase prices, partly linked to the operating times and partly to the Hospital production costs. Given the limited time span and the homogeneous distribution over almost two years, an analysis of variance of the purchase or production cost will not be carried out but the average costs for the period (purchase or production) will be considered, on all patients evaluated.
Full table
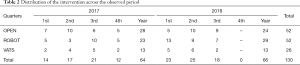
The interventions are distributed, in the period considered, as shown in Table 2 and were all operated with reimbursement charged to the National Health System; of these, 40% OPEN was resident in the Lombardy Region at the date of intervention that is the same region where the Hospital is, 37% for ROBOT operations and 42% for VATS.
Full table
Results
The costs of 52 patients operated with the help of ROBOT were analyzed, 52 patients operated on OPEN and 26 patients on VATS.
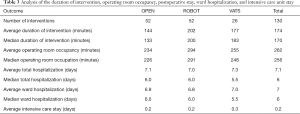
The median duration (skin-skin) of the ROBOT intervention was equal to 3 hours and 1/4 of an hour longer than the OPEN intervention (2 h 1/4) and a quarter of an hour longer than the VATS (3 h). The operating room was occupied, in the median survey, for 4 hours and 3/4 for the ROBOT intervention, 3 hours and 3/4 for the OPEN intervention and 4 hours and 1/4 for the VATS. The average and median wards detected are, overall, very comparable between the methods (Table 3).
Full table
Regarding cost analysis, we have considered the costs for laboratory tests, diagnostic imaging and pathological anatomy as a hospital cost to provide each service (full costing methodology); the cost for room materials and drugs we considered the weighted average cost of purchase and per unit dose of the drug. Weighted average purchase cost also for medical devices used, the cost of personnel for surgeons, anesthesiologists, nursing staff, technicians and health workers was calculated as normal cost per minute for each specialty (market cost for each professional figure, considering a seniority of more than 3 years); Depreciation and maintenance were considered in relation to the effective duration of the operating room occupation, the daily hospitalization costs are the specific hospital costs of the ward and of intensive care, compared to the total days of the period for the days of stay on the specific beds.
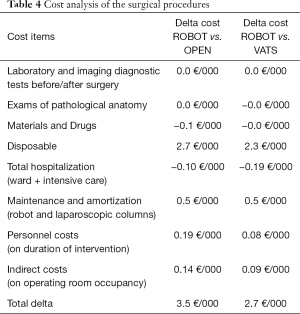
As can be seen in Table 4, we recorded overall costs for the ROBOT intervention noticeably higher both in comparison with the OPEN intervention (+3.5 thousand Euros), and in resemblance to the VATS intervention (+2.7 thousand Euros). The differential cost towards the OPEN methodology is due for 79% to the cost for the robotic kits used, while a further 15% is due to amortization and maintenance of the robot itself. Compared to the VATS technique, 83% of the higher costs recorded are linked to robotic kits and the residual difference to the maintenance and depreciation of robotic equipment.
Full table
In both comparisons there were no differences in costs for laboratory tests, pathological anatomy or diagnostic imaging, for the methodology followed these would be attributable solely to the number of services required before and after the intervention, which instead resulted the same in the three methodologies investigated.
Discussion
The results obtained on homogeneous patients thus confirm the widespread idea that robotic surgery is more expensive. If the higher cost towards OPEN surgery may be justified mainly by less invasive, then less pain for the patient and faster recovery times, to justify the difference in cost towards VATS surgery we should probably refer to the surgeon’s propensity and the greater ability that the robot allows to control against possible faults.
In the case of lung cancer, the main differential cost, we have seen, is linked to the robotic kit that, over time, does not register downward variations linked to lack of competitive pressures. So also the purchase, then the depreciation and maintenance of the robot itself.
Data concerning room occupation time we obtained are comparable with the results obtained from other studies (2-5). On the other hand, as regards the hospital stay, the cited study detects a hospitalization for patients operated OPEN (3) one day longer, which we did not find on the patients we examined (the median value for OPEN and ROBOT patients is the same, for VATS patients there is a median value of half a day less).
The cost of the robotic intervention can therefore be reduced, verifying the real need for hospitalization of the patients and transferring to subsequent moments the additional control needs, with a patient who is no longer hospitalized. Even the interval of intervention and room occupancy could be slightly diminished with the increasing experience but, as was evident from the analysis of differential costs (Table 4), the elements of expenditure related to the robot (kit, depreciation and maintenance) fully explain the differences of cost both to OPEN and VATS, so other reductions may only impact slightly.
Acknowledgements
A special thanks goes to Patrick Maisonneuve and to Daniela Brambilla for their precious contribution with statistical analysis and data management.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Gaskin DJ, Richard P. Relieving Pain in America: A Blueprint for Transforming Prevention, Care, Education, and Research. Appendix C The Economic Costs of Pain in the United States. Washington (DC): National Academies Press (US); 2011.
- Turchetti G, Palla I, Pierotti F, et al. Economic evaluation of da Vinci-assisted robotic surgery: a systematic review. Surg Endosc 2012;26:598-606. [Crossref] [PubMed]
- Cools-Lartigue J, Park BJ. Economic assessment in minimally invasive thoracic oncological surgery—USA experience. Shanghai Chest 2018;2:89. [Crossref]
- Novellis P, Alloisio M, Vanni E, et al. Robotic lung cancer surgery: review of experience and costs. J Vis Surg 2017;3:39. [Crossref] [PubMed]
- Turchetti G, Pierotti F, Palla I, et al. Comparative health technology assessment of robotic-assisted, direct manual laparoscopic and open surgery: a prospective study. Surg Endosc 2017;31:543-51. [Crossref] [PubMed]
Cite this article as: Di Filippo A, Galetta D, Spaggiari L. Economic assessment in minimally invasive oncological surgery: a high European volume center experience. Shanghai Chest 2019;3:14.


