Preliminary experience in uniportal video-assisted thoracoscopic surgery (VATS)
Introduction
In recent years, technical evolution in the field of minimally invasive thoracic surgery has allowed a progressive reduction of invasiveness in performing lobectomies, leading to fewer post-operative complications, less post-surgical pain, eventually fostering a shorter hospital stay. According to recent international guidelines on management of non-small lung cancer, minimally invasive surgery should be considered the preferred approach to pulmonary lobectomy in early stages (1,2).
Within the framework of minimally invasive approaches, the uniportal technique [uniportal video-assisted thoracoscopic surgery (VATS) lobectomy, UVL] aims to decrease surgical trauma to a minimum, while ensuring a correct oncological procedure (3-5). In detail, it seems to provide some advantages compared to multiportal approaches. These advantages can be summarized as follows:
- Less post-operative pain. The uniportal approach involves only one intercostal space, although the incision is longer than in multiportal approach, entailing a limited engagement of the intercostal nerves the main responsible of post-operative pain. Furthermore, the uniportal approach, unlike multiportal approaches, does not require the use of rigid metallic trocars squashing in the intercostals space and causing compression of the intercostal nerves. In particular, in UVL only a soft tissue retractor which does not cause intercostal nerve compression of the access space is used (6).
- The uniportal approach determines an ergonomic improvement for the surgeon, who stands in the front of both the surgical target and the screen. This “global continuity” (surgeon-target-screen), underlined by Martin-Ucar (5), prevents undue trunk rotation and promote a straightforward management of space (no rotation angle between vision vector and force vectors is produced) (7).
Learning curve dynamics are still to be clarified. However, general perception is that the amount of experience needed for development of competency is similar to multiport approaches (8). Given these perceived advantages, we decided to progressively introduce uniportal VATS as part of our technical armamentarium as described below.
Methods
A consultant (A Viti) with previous experience in multiport VATS and a brief exposure to uniportal wedge resections in another hospital attended as visiting fellow a tertiary referral centre in UK (Sheffield Northern General Hospital) with a long and wide experience in UVL and subsequently participated in the Uniportal VATS Training Program at the Shanghai Pulmonary Hospital (SPH) (June 2016). Both these experiences allowed huge exposure to the technique. Another Consultant (P Bertoglio) attended the Fourth International Uniportal VATS course, Berlin, 2016. A step-by-step introduction to uniportal VATS was planned. First of all, the technique was applied to simpler procedures (wedge resections, in some cases associated with nodal sampling). In this phase we employed standard (i.e., straight) VATS instruments.
This first stint of procedures was particularly useful since some technical issues were raised (correct port placement, need for further instrumentation to enhance dissection). After attending another specialized course (Second Roman Tips and Tricks in Thoracic Surgery, The Great Potential of Uniportal VATS, Rome, 2017), the following issues were addressed:
- Correct patient placement (tips in patients’ arms positioning);
- Localization of the optimal intercostal space according to the planned procedure;
- Exposure of the hilum and efficient traction on the lung;
- Importance of dedicated instrumentation and different features of high energy devices available.
Dedicated instrumentation was made available in our hospital in January 2017 and included tools for hilar dissection (Dennis and Gonzalez-Rivas Dissectors) as well as a dedicated uniportal suction device. After this further step, we started performing major lung resections with a standardized instrumentation and technique (9).
We evaluated the employment of the technique in the period between March 2017 and June 2018, describing procedure type, conversion rate to multiportal or thoracotomy, post-operative complications and hospital stay.
Results
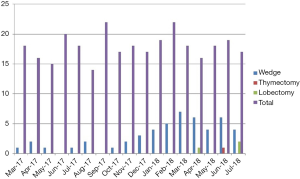
Patients’ characteristics are summarized in Table 1. An incremental adoption of the procedure was observed over time (Figure 1). We performed 52 procedures (49 minor resections, 1 thymectomy for thymic hyperplasia, 2 lobectomies). Conversion to multiportal VATS was required in 15 cases (14 wedge resections, and 1 thymectomy). No major complications occurred intraoperatively. Median post-operative stay was 3 days for wedge resection (range, 2–5 days) and 6 and 7 days for lobectomies.
Table 1
| Patient characteristics | Total population (n=52) |
|---|---|
| Age (years, mean ± SD) | 67.05±9.80 |
| Male gender, n [%] | 33 [61] |
| BMI (mean ± SD) | 28.23±4.50 |
| Thoracoscore (mean ± SD) | 1.98±0.60 |
| FEV1 (%, mean ± SD) | 83.12±25.00 |
| Positive smoking history, n [%] | 44 [59] |
| Wedge resections | 49 |
| Upper | 28 |
| Lower | 21 |
| Lymphnode sampling | 12 |
| Lobectomies | 2 |
| Mediastinal procedures | 1 |
Discussion
Previous expertise in multiportal VATS
Competency appraisal for UVL and its relationship with previous multiport expertise has been evaluated by Martin-Ucar and colleagues (10). They compared the first 50 lobectomies performed through the single-port VATS approach by three surgeons who completed at least 50 cases of multiport VATS with three “VATS naïve” surgeons, who didn’t. The authors concluded that, although there was no noticeable difference in terms of outcomes, naïve surgeons applied uniportal more frequently to lower lobectomies and had a major incidence of conversions. Complication rate was similar. These results show that Uniportal VATS did not require previous multiport VATS experience. According to our experience, we perceived some substantial differences between multiportal and uniportal approach (11). The loss of triangulation imposes a paradigm shift towards a more direct approach to target lesions, similar to open surgery (7). If the loss of triangulation may prove sometimes frustrating in case wedge resection of peripheral lesions, as previously demonstrated (11), it allows more natural dissection lines of hilar structures. To sum up, we think that previous expertise in multiportal VATS lobectomy although helpful is not mandatory.
Mentoring
Although an extensive experience in multiport VATS should not be considered mandatory in order to set up an uniportal VATS program, preliminary exposure to the technique, by attending to a specific course, should be strongly encouraged. A unique opportunity for an extraordinary exposure to uniportal VATS is now available.
In the last decade, together with the introduction of uniportal VATS, we witnessed the development of “ultra-high-volume centers (UHVCs)” in thoracic surgery (12). The SPH is a notable example of this relatively new organizational facility. These centers, mostly voted to minimally invasive surgery, provide the possibility of exposure to a gargantuan number-per-day of thoracic procedures to small groups of surgeons (on average 60–80 surgeries daily at SPH, mostly uniportal major lung resections), defining a new paradigm in training (13).
To date, also many international and national-based meetings have been organized by experts in the field. Some of these meetings are now well established in Europe: the “Roman Tips and Tricks in Thoracic Surgery” Rome (Italy), Internal Uniportal VATS Course, Postdam (Germany) and International VATS symposium, London, UK. These courses provide state-of-the-art lectures, hands-on sessions and live surgeries. We experienced a “two-step” exposure to the technique: visiting a high-volume facility, which provided exposure to a variety of uniportal interventions providing general overview and a big deal of information, so that we were able to start practicing uniportal VATS in lesser procedures. In this early phase, we have been dealing with some technical problems so that we decided to join two well established and internationally recognized courses. The participation to these focused events helped fixing the issues we have been encountering during the very first period. For instance, we changed the way of positioning the patient (from a multiport-like setup to a “dedicated” uniport setup). The importance of a complete dedicated kit was underlined as well.
Dedicated instrumentation
Since the first groundbreaking reports (14,15), the need for dedicated instrumentation was strongly advocated. Now, the steep rise in number and range of uniportal procedures has prompted manufacturers to develop a specific instrumentation. Smaller, curved, double-hinged instruments have been produced (9). They prevent excessive torque on the chest wall, overcrowding of the single access point and a more natural posture of the surgeon’s arms. We soon understood the need for a dedicated set while performing the first procedures with standard instruments. In particular, we found some difficulties in performing hilar dissection and mediastinal node sampling due the lack of short curved instruments. Once these instruments were made available, they allowed a more straightforward vascular dissection thanks to narrow shaft and the specific angles of the tips (Figure 2). We do believe that dedicated instruments are very important, and we strongly suggest their adoption from the very beginning of a structured uniportal VATS program. A variety of specialized instrument are now manufactured, so that a certain degree of personalization of kits has been made possible.
Conclusions
Uniportal VATS represents both a challenge and an opportunity. Unlike other minimally invasive approaches, given its differences in spatial perception and loss of triangulation, it forces the surgeons to initially change their approach, fostering the development of specific skills. This will result in a more intuitive approach, enhanced ergonomics, as clearly shown for wedge resections (11), besides the obvious benefits for patients. Further studies, focused on major lung resections and learning mechanisms, may provide a better understanding on how to overcome the difficulties encountered by surgeons who approach the technique for the first time. In the meanwhile, we believe that dedicated courses, intensive training and specific instrumentation may help overcoming the initial difficulties.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editors (Stefano Margaritora, Roberto Crisci and Elisa Meacci) for the series “The Second Roman Tips and Tricks in Thoracic Surgery - the Great Potential of Uniportal VATS” published in Shanghai Chest. The article has undergone external peer review.
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/shc.2019.07.07). The series “The Second Roman Tips and Tricks in Thoracic Surgery - the Great Potential of Uniportal VATS” was commissioned by the editorial office without any funding or sponsorship. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the institutional ethical committee (No.1860) and written informed consent was obtained from all patients.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Vansteenkiste J, Crinò L, Dooms C, et al. 2nd ESMO Consensus Conference on Lung Cancer: early-stage non-small-cell lung cancer consensus on diagnosis, treatment and follow-up. Ann Oncol 2014;25:1462-74. [Crossref] [PubMed]
- Falcoz PE, Puyraveau M, Thomas PA, et al. Video-assisted thoracoscopic surgery versus open lobectomy for primary non-small-cell lung cancer: a propensity-matched analysis of outcome from the European Society of Thoracic Surgeon database. Eur J Cardiothorac Surg 2016;49:602-9. [Crossref] [PubMed]
- Wang L, Liu D, Lu J, et al. The feasibility and advantage of uniportal video-assisted thoracoscopic surgery (VATS) in pulmonary lobectomy. BMC Cancer 2017;17:75. [Crossref] [PubMed]
- Ismail M, Swierzy M, Nachira D, et al. Uniportal video-assisted thoracic surgery for major lung resections: pitfalls, tips and tricks. J Thorac Dis 2017;9:885-97. [Crossref] [PubMed]
- Martin-Ucar AE, Socci L. Why perform uniportal video-assisted thoracic surgery?-multiple considerations. J Vis Surg 2016;2:108. [Crossref] [PubMed]
- Abouarab AA, Rahouma M, Kamel M, et al. Single Versus Multi-Incisional Video-Assisted Thoracic Surgery: A Systematic Review and Meta-analysis. J Laparoendosc Adv Surg Tech A 2018;28:174-85. [Crossref] [PubMed]
- Bertolaccini L, Rocco G, Viti A, et al. Geometrical characteristics of uniportal VATS. J Thorac Dis 2013;5:S214-6. [PubMed]
- Bedetti B, Bertolaccini L, Solli P, et al. Learning curve and established phase for uniportal VATS lobectomies: the Papworth experience. J Thorac Dis 2017;9:138-42. [Crossref] [PubMed]
- Ng CS, Rocco G, Wong RH, et al. Uniportal and single-incision video-assisted thoracic surgery: the state of the art. Interact Cardiovasc Thorac Surg 2014;19:661-6. [Crossref] [PubMed]
- Martin-Ucar AE, Aragon J, Bolufer Nadal S, et al. The influence of prior multiport experience on the learning curve for single-port thoracoscopic lobectomy: a multicentre comparative study†. Eur J Cardiothorac Surg 2017;51:1183-7. [Crossref] [PubMed]
- Bertolaccini L, Viti A, Terzi A. Ergon-trial: ergonomic evaluation of single-port access versus three-port access video-assisted thoracic surgery. Surg Endosc 2015;29:2934-40. [Crossref] [PubMed]
- Sihoe ADL, Han B, Yang TY, et al. The Advent of Ultra-high Volume Thoracic Surgical Centers in Shanghai. World J Surg 2017;41:2758-68. [Crossref] [PubMed]
- Sihoe ADL, Gonzalez-Rivas D, Yang TY, et al. High-volume intensive training course: a new paradigm for video-assisted thoracoscopic surgery education. Interact Cardiovasc Thorac Surg 2018;27:365-71. [Crossref] [PubMed]
- Rocco G, Martin-Ucar A, Passera E. Uniportal VATS wedge pulmonary resections. Ann Thorac Surg 2004;77:726-8. [Crossref] [PubMed]
- Gonzalez D, Paradela M, Garcia J, et al. Single-port video-assisted thoracoscopic lobectomy. Interact Cardiovasc Thorac Surg 2011;12:514-5. [Crossref] [PubMed]
Cite this article as: Viti A, Bertoglio P, Terzi A. Preliminary experience in uniportal video-assisted thoracoscopic surgery (VATS). Shanghai Chest 2019;3:43.