
Valve-sparing versus valve-replacing aortic root operations in patients with Marfan syndrome
Introduction
Aortic root dissection and rupture are the leading causes of death in patients with Marfan syndrome (1,2). Marfan syndrome is a heritable connective tissue disorder with autosomal dominant inheritance; it is caused by an FBN1 gene mutation that results in irregular development and cellular handling of the fibrillin-1 protein, a crucial component of the extracellular aortic matrix. The syndrome affects approximately 1 in 10,000 individuals (3). The disease is detected using the revised Ghent-2 guidelines, which base the diagnosis on clinical symptoms, family history, and genetic testing (2).
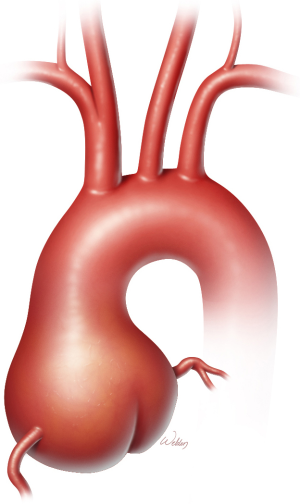
Approximately 80% of patients with Marfan syndrome have annuloaortic ectasia (Figure 1), a distinctive form of aortic root dilation that often leads to aortic or mitral valve regurgitation, congestive heart failure, or aortic dissection or rupture (2-4). Any of these factors can shorten life expectancy in these patients (5,6). Before surgical intervention became common, median survival in Marfan syndrome was approximately 48 years, and most premature deaths were due to aortic pathology (6). With the availability of appropriate cardiovascular surgery to minimize the risk for aortic complications, life expectancy for Marfan patients is now similar to that of the general population.
Evolution of aortic root surgery
The cornerstone of care for preventing and managing aortic complications related to Marfan syndrome is the surgical treatment of the aorta. The procedures undertaken to address the risk for aortic dissection have evolved gradually since 1968, when Bentall and De Bono recorded their first aortic root replacement (ARR) at Hammersmith Hospital (7). This initial ARR, performed in a 33-year-old man with suspected Marfan syndrome, involved the insertion of a mechanical Starr-Edwards valve hand-sewn into a Teflon tube graft, in which the coronary orifices were sutured directly into the graft without separation from the aortic wall, and the native aorta was then wrapped around the root replacement. Two decades later, Kouchoukos et al. (8) modified this approach by mobilizing the coronary arteries on tissue buttons, thereby obviating the need for the inclusion technique and reducing the risk for late pseudoaneurysm.
ARR methods have undergone numerous adaptations over time, largely in response to late complications. Now that ARR-related perioperative risk is low and long-term survival is expected, long-term effects and surgical durability have emerged as important considerations. Although excellent results were obtained with ARR using a mechanical valve-replacement procedure, it committed younger patients to a lifetime risk for valve-related thromboembolism and an associated fear of bleeding from the anticoagulation needed to reduce that risk. This limitation engendered interest in developing an alternative approach, leading Yacoub et al. (9) and David et al. (10) to pioneer native aortic valve preservation during ARR.
Indications for aortic root surgery in Marfan syndrome
For more than 40 years, patients with Marfan syndrome have undergone elective replacement of the aortic root (11). For those aged 20 to 50 years, elective ARR is usually performed on the basis of patient-specific factors, as stated in current guidelines. Guidelines for asymptomatic patients with Marfan syndrome recommend elective ARR for patients with any of the following: aortic root aneurysm ≥50 mm in diameter, aortic root aneurysm ≥45 mm and a family history of aortic dissection, rapid aneurysm expansion (>3 mm per year), extreme aortic or mitral valve regurgitation, or pregnancy plans (12).
In contemporary practice, there are two competing ARR approaches in patients with Marfan syndrome: valve replacement surgery (VRARR) with either a mechanical or tissue prosthetic aortic valve, and valve-sparing surgery (VSARR) (Figure 2). VRARR with a mechanical valve requires lifelong anticoagulation; the durability of bioprosthetic (tissue) valves is unclear. VSARR methods include the scalloped remodeling approach developed by Yacoub and colleagues (9), multiple variations of the reimplantation and other techniques introduced by David and colleagues (10), and most recently the Florida sleeve (13), which failed to pass the long-term durability check (14). Notably, the Yacoub remodeling method tended to leave the annulus unsupported and prone to dilatation over time, frequently resulting in late regurgitation of the aortic valve and eventual need for reoperation (15); this has generally limited the use of the Yacoub approach to VSARR, although it may be considered in older patients.
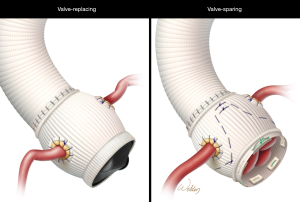
Today, reimplantation approaches, as led by David, are the widely preferred VSARR method; notably, these techniques vary considerably among experienced centers (11,16).
The what, who, when, where, why, and how of ARR in Marfan syndrome
The question for people with Marfan syndrome, their families, and their surgeons is whether to choose VSARR or VRARR, a decision that must take into account these techniques’ competing risks; the evidence provided advises the choice but does not promote it.
Because patients with Marfan syndrome can expect an almost normal life span nowadays, the risk for thromboembolic and bleeding events resulting from lifelong oral anticoagulation after mechanical ARR is increasingly a concern, and VSARR appears to be an attractive option for minimizing these risks. Nonetheless, VSARR carries some risk for adverse outcomes. In a study of 1385 patients with Marfan syndrome who underwent ARR, Benedetto et al. (17) calculated a 0.7% per year thromboembolic hazard estimate associated with a mechanical valve, compared with a 1.3% per year risk for native valve failure requiring reoperation.
Accurately assessing an individual patient’s risk for stroke versus the likelihood of reoperation can be difficult. The choice between VSARR and VRARR is often made intraoperatively; whether VSARR is feasible and durable is ultimately determined on the basis of the native aortic valve’s performance. For patients with substantial leaflet fenestration, excessive tissue, annular dilation, or free margin elongation, VSARR is a poor choice in the hands of most surgeons (18).
In 1999, Gott et al. (19) published a landmark multicenter report showing that ARR can prolong life in patients with Marfan syndrome. Ten surgical centers, including our own, contributed data for this study. The benefit of ARR in Marfan syndrome patients was clear: with low risk for surgical death (3.3%), prophylactic repair dramatically changed these patients’ prognosis from a terminal sentence to a survivable condition. The vast majority of this experience was VRARR; however, a small cohort of VSARR was included. There were few differences in early results between the VRARR and VSARR cohorts, who had similarly low rates of operational death. The article described VRARR as a permanent method of repair and the treatment of choice for most surgeons, noting that “the role of valve-sparing procedures in Marfan syndrome patients remains unclear”.
The AVOMP (Aortic Valve Operative Outcomes in Marfan Patients) prospective, international registry study examined early and mid-term VRARR and VSARR outcomes in Marfan syndrome patients (20). The overall impression from this study, given a significantly longer period of cardiopulmonary bypass, aortic cross-clamp, and surgery in the VSARR cohort, was that the form of ARR had no effect on early results. More specifically, results showed that VSARR does not have to be limited to technically gifted surgeons, but is a reproducible strategy.
In a subsequent study of 1-year results from the same registry, the survival rates for VRARR and VSARR groups were comparable, and the type of procedure was not significantly associated with any valve-related events (21). Although functional mortality rates were comparable (one in each group), 7% of VSARR patients had more than mild aortic valve regurgitation at 1 year, validating previous durability concerns.
A study from Hamburg (22) on ARR outcomes in patients with Marfan syndrome over a short observation period found two deaths from heart failure and arrhythmia during the observation period among 58 patients who underwent the David procedure. Freedom from aortic regurgitation rated as moderate or greater was 80% at 10 years, and only two patients (3.4%) had repeated aortic root surgery.
Benedetto et al. (17) published a systematic review and meta-analysis of 11 articles culled from an initial assessment of 530 studies identified via PubMed, Embase, and the Cochrane library. In this analysis of long-term results of 1,385 Marfan syndrome patients (Bentall procedure: 972 patients; VSARR: 413 patients), no differences were found in valve-related complication or endocarditis rates; however, the thromboembolism rate was higher in VRARR, and the aortic valve reintervention rate was higher in VSARR.
In a 2014 systematic review of six clinical trials, Hu et al. (23) analyzed data from 539 patients with Marfan syndrome; the risk ratios for complications (re-exploration for hemorrhage, early mortality, thromboembolism, endocarditis, repeat surgery on the aortic root, late mortality) were calculated for VSARR versus the Bentall procedure, along with the incidence of moderate or severe regurgitation in various procedure types. The results confirmed VSARR’s superiority in terms of hemorrhage, thromboembolism, endocarditis, re-exploration, and long-term survival. Moderate or severe regurgitation occurred in 2–5% of patients undergoing the David procedure, approximately 20% of patients undergoing the Yacoub procedure, and 0–8% of patients with a Valsalva graft; those undergoing the Yacoub procedure, which tends to leave the annulus unsupported, had a higher incidence of regurgitation than did the other VSARR patients.
A recent systematic review and meta-analysis reported by Flynn et al. (24) evaluated 23 studies reporting the outcomes of aortic root surgery in 2,976 Marfan patients. Of these, 1,624 patients were treated with VRARR and 1,352 patients were treated with VSARR. Compared with VRARR, VSARR was associated with reduced risk for thromboembolism, late hemorrhagic complications, and endocarditis. No significant difference was found in reintervention rates between VSARR and VRARR. This study showed that an increasing body of evidence indicates that VSARR can be reliably performed in patients with Marfan syndrome.
Conclusions
Over time, prophylactic repair at lower aortic diameters in patients with Marfan syndrome has been made possible by advances ensuring that ARR could be repeated safely at multiple sites, could be accomplished with a low early mortality rate, and could extend life. Although unanswered questions remain about the optimal ARR approach for patients with Marfan syndrome, as evident in various contemporary publications (14,21-24), valve-sparing procedures are now more commonly used than valve-replacement approaches in these patients. Nevertheless, VSARR approaches were developed by master surgeons, and it should be borne in mind that this method often includes painstaking repair of the valve leaflet, which requires advanced surgical skills. In the end, the choice between VRARR and VSARR is complex and requires input from the patient as well as guidance from an experienced surgeon.
Acknowledgments
Jeanie F. Woodruff, BS, ELS, and Susan Y. Green, MPH, contributed to the editing of the manuscript. The authors thank Scott Weldon, MA, CMI, FAMI, for illustrations; Mr. Weldon’s work is partly supported by the E. Stanley Crawford Endowment.
Footnote
Conflicts of Interest: Dr. Coselli consults for and participates in clinical trials with Medtronic and W.L. Gore; and consults for, participates in clinical trials with, and receives royalties and grant support from Terumo Aortic. Dr. Cekmecelioglu has no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
References
- Judge DP, Dietz HC. Marfan's syndrome. Lancet 2005;366:1965-76. [Crossref] [PubMed]
- Loeys BL, Dietz HC, Braverman AC, et al. The revised Ghent nosology for the Marfan syndrome. J Med Genet 2010;47:476-85. [Crossref] [PubMed]
- Fleischer KJ, Nousari HC, Anhalt GJ, et al. Immunohistochemical abnormalities of fibrillin in cardiovascular tissues in Marfan's syndrome. Ann Thorac Surg 1997;63:1012-7. [Crossref] [PubMed]
- Coselli JS, Weldon SA, Preventza O, et al. Valve-sparing versus composite root replacement procedures in patients with Marfan syndrome. Ann Cardiothorac Surg 2017;6:692-6. [Crossref] [PubMed]
- Groenink M, Lohuis TA, Tijssen JG, et al. Survival and complication free survival in Marfan's syndrome: implications of current guidelines. Heart 1999;82:499-504. [Crossref] [PubMed]
- Silverman DI, Burton KJ, Gray J, et al. Life expectancy in the Marfan syndrome. Am J Cardiol 1995;75:157-60. [Crossref] [PubMed]
- Bentall H, De Bono A. A technique for complete replacement of the ascending aorta. Thorax 1968;23:338-9. [Crossref] [PubMed]
- Kouchoukos NT, Wareing TH, Murphy SF, et al. Sixteen-year experience with aortic root replacement. Results of 172 operations. Ann Surg 1991;214:308-18; discussion 18-20. [Crossref] [PubMed]
- Yacoub MH, Gehle P, Chandrasekaran V, et al. Late results of a valve-preserving operation in patients with aneurysms of the ascending aorta and root. J Thorac Cardiovasc Surg 1998;115:1080-90. [Crossref] [PubMed]
- David TE, Armstrong S, Ivanov J, et al. Results of aortic valve-sparing operations. J Thorac Cardiovasc Surg 2001;122:39-46. [Crossref] [PubMed]
- Coselli JS. It's time to get to the root of things. J Thorac Cardiovasc Surg 2016;151:291-3. [Crossref] [PubMed]
- Erbel R, Aboyans V, Boileau C, et al. 2014 ESC Guidelines on the diagnosis and treatment of aortic diseases: Document covering acute and chronic aortic diseases of the thoracic and abdominal aorta of the adult. The Task Force for the Diagnosis and Treatment of Aortic Diseases of the European Society of Cardiology (ESC). Eur Heart J 2014;35:2873-926. [Crossref] [PubMed]
- Hess PJ Jr, Klodell CT, Beaver TM, et al. The Florida sleeve: a new technique for aortic root remodeling with preservation of the aortic valve and sinuses. Ann Thorac Surg 2005;80:748-50. [Crossref] [PubMed]
- Orozco-Sevilla V, Whitlock R, Preventza O, et al. Redo aortic root operations in patients with Marfan syndrome. Int J Angiol 2018;27:92-7. [Crossref] [PubMed]
- Cameron DE, Alejo DE, Patel ND, et al. Aortic root replacement in 372 Marfan patients: evolution of operative repair over 30 years. Ann Thorac Surg 2009;87:1344-9; discussion 9-50. [Crossref] [PubMed]
- David TE, Coselli JS, Khoury GE, et al. Aortic valve repair. Semin Thorac Cardiovasc Surg 2015;27:271-87. [Crossref] [PubMed]
- Benedetto U, Melina G, Takkenberg JJ, et al. Surgical management of aortic root disease in Marfan syndrome: a systematic review and meta-analysis. Heart 2011;97:955-8. [Crossref] [PubMed]
- David TE, David CM, Feindel CM, et al. Reimplantation of the aortic valve at 20 years. J Thorac Cardiovasc Surg 2017;153:232-8. [Crossref] [PubMed]
- Gott VL, Greene PS, Alejo DE, et al. Replacement of the aortic root in patients with Marfan's syndrome. N Engl J Med 1999;340:1307-13. [Crossref] [PubMed]
- Volguina IV, Miller DC, LeMaire SA, et al. Valve-sparing and valve-replacing techniques for aortic root replacement in patients with Marfan syndrome: Analysis of early outcome. J Thorac Cardiovasc Surg 2009;137:1124-32. [Crossref] [PubMed]
- Coselli JS, Volguina IV, LeMaire SA, et al. Early and 1-year outcomes of aortic root surgery in patients with Marfan syndrome: a prospective, multicenter, comparative study. J Thorac Cardiovasc Surg 2014;147:1758-66, 67 e1-4.
- Bernhardt AM, Treede H, Rybczynski M, et al. Comparison of aortic root replacement in patients with Marfan syndrome. Eur J Cardiothorac Surg 2011;40:1052-7. [PubMed]
- Hu R, Wang Z, Hu X, et al. Surgical reconstruction of aortic root in Marfan syndrome patients: a systematic review. J Heart Valve Dis 2014;23:473-83. [PubMed]
- Flynn CD, Tian DH, Wilson-Smith A, et al. Systematic review and meta-analysis of surgical outcomes in Marfan patients undergoing aortic root surgery by composite-valve graft or valve sparing root replacement. Ann Cardiothorac Surg 2017;6:570-81. [Crossref] [PubMed]
Cite this article as: Cekmecelioglu D, Coselli JS. Valve-sparing versus valve-replacing aortic root operations in patients with Marfan syndrome. Shanghai Chest 2020;4:23.


