
Principles of complex chest wall reconstruction
Introduction
Chest wall reconstruction remains a big problem in Thoracic Surgery. The main indication for chest wall reconstruction are thoracic defects after resection of lung cancer, the repair of congenital deformities, post traumatic deformity and also complications of surgery (1). The term complex chest wall reconstruction usually includes a procedure required to repair large defects of the chest wall using a combination of materials including various flaps, omentoplasty (2) and in recent years a microvascular technique as well as individually made artificial replacements. The complexity of chest wall reconstruction does not necessarily include technical difficulties of surgery but also general complex clinical situations such as chest wall defects in patients after transplant surgery with suppressed immunity and healing requiring technically relatively simple procedures to achieve closure of the defect. Usually in these cases artificial material should be avoided (3) and the wound should be closed with natural flaps and transposed omentum. The indications for chest wall reconstruction varies but commonly includes defects of more than 5 cm in diameter when four or more ribs are absent with the risk of lung herniation and paradoxical motion of the chest wall. More frequently chest wall reconstruction is required when the defect is located in an anterolateral position. Prior to considering surgery for chest wall reconstruction, the existing function loss or cosmetic problems must be assessed as well as adequate control of underlying disease, the available technical resources and the acceptable risk of complications. After taking on board all these factors, the surgeon and the patient may conclude that reconstruction is not beneficial at all because of the potential risks and serious consequences for the patient.
Operative technique
The main technical principles of chest wall reconstruction are of a stable repair, compatibility of materials and meticulous surgical technique to minimise potential complications and the combination of available technologies. Apart from muscular or musculo-cutaneous flaps and omentum, the most commonly used materials for chest wall reconstruction are metal bars, various forms of plastic mesh, titanium mesh, cement and occasionally cadaveric bone. The use of 3D printing is gaining its popularity, but it is still in the experimental stage.
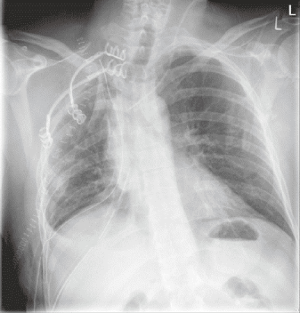
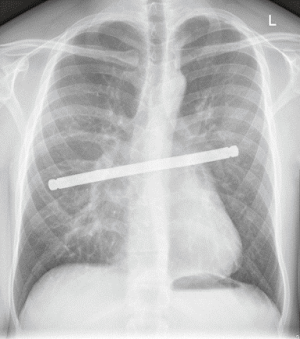
In lung cancer surgery, chest wall reconstruction may be required after chest wall resection performed due to direct invasion of the tumour into the chest wall. If the tumour is located in the lung apex (Figure 1) causing Pancoast syndrome, reconstruction is rarely indicated, however it may be necessary to prevent dropping of the shoulder and maintaining the shape of the chest wall close to normal. In these cases, the metal bars may be used to recreate the anatomically acceptable shape of the chest wall. StraTos bars (MedXpert, Germany) could be quite useful, because it is possible to bend them to the required shape and to secure them normally or in the invert position if required (Figure 2). The repair of the first rib is usually not possible and not usually performed.

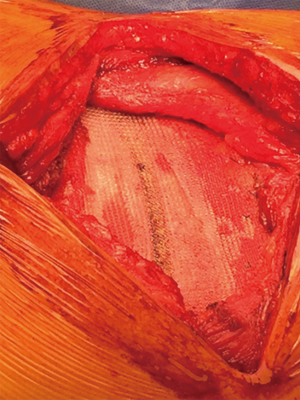
More frequently chest wall reconstruction is required for peripheral lung cancer invading lateral aspects of the chest wall. In this situation absent ribs also could be replaced by various forms of titanium bars, such as titanium Stratos bars (MedXpert, Germany) which are available in different size and could be also trimmed according to the individual need (Figure 3). If the muscle defect over the bars is significant, overlying Prolene mesh may be helpful to prevent lung herniation in the postoperative period.
If the defect of the chest wall is very large, particularly after resection of a primary malignant tumour of the chest wall and where is no technical possibility to secure metal bars, a combination of cement and natural flaps could be an ideal option. Most commonly used is methyl methacrylate bone cement in combination with a synthetic mesh (4) applied to the defect and covered with a latissimus dorsi muscle flap. Following resection of the sternum, one of the ways to replace the defect would be to use a cadaveric sternum, which is put in place and secured with various forms of metal bars attached to the adjacent ribs.
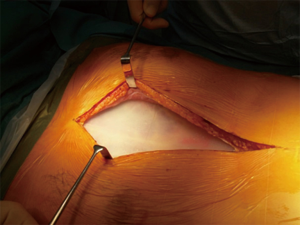
Complex chest wall reconstruction is also indicated in patients operated for borderline pathology such as aggressive desmoid fibroma or other benign or borderline pathology of the chest such as fibrous dysplasia of the rib. The defect after resection may be very large because desmoid fibroma requires wide incision due to well-known tendency to grow deep onto the skeletal muscle so the defect could comparable to the defect expected after resection of a malignant tumour.
In these cases, the implantation of a metal bar covered with Prolene Mesh would be ideal to resolve this problem (Figure 4). Amongst the varieties of metal bars in place, it is preferable to use bars made from titanium because this metal is inert and rarely causing infective complications.
Another area of chest wall reconstruction, which could be considered complex is the repair of congenital chest wall deformities such as pectus excavatum or pectus carinatum in young adults or occasionally in patients with a more advanced age. Many versions of the same procedure originally suggested by Ravitch (5) exist, and all of them include the repair of the normal anatomy with the stable fixation of the repair. This surgery is performed via a transverse incision with a patent placed in a decubitus position. For this purpose, titanium bars are also ideal because they allow to maintain stability, but these bars require removal at a later stage, which is the down side of this procedure. The reconstruction may also be semi-rigid. As an example, the sternum may be secured with strips of Prolene Mesh positioned under the sternum and attached to the bony ends of the resected costal cartilages using non-absorbable sutures making them adequately tight after one end is properly fixed. This type of repair does not require a repeat procedure to remove the mesh.
Another area of complex and difficult surgery is operating on patients with complications of attempted repair of congenital chest wall deformities. The usual indications in this situation would be sub-optimal correction, retained metal constructions (Figure 5), persistent pain and an unstable chest.
For this kind of surgery, a wide surgical access is usually required. Even though a transverse incision is preferential, the old incision should be used, if previously a vertical incision was employed (Figure 6). An attempt to just perform a minimal procedure usually is not satisfactory because it does not lead to a desired result and does not allow to remove firmly embedded foreign material into the chest, so full exposure and complete reconstruction is required to achieve nearly normal anatomy and firm stabilisation.
A relatively rare, but a very problematic area of chest wall reconstruction is late dehiscence of the sternum after median sternotomy routinely used in cardiac surgery (6). This type of sternal dehiscence usually occurs 3–6 months after sternotomy. Patients who are prone for this complication frequently have diabetes and an increased body mass, osteoporosis and bilateral harvesting of internal thoracic arteries.
Indications for reconstruction of sternal non-union after sternotomy are relatively simple. These patients suffer from persisting symptoms of an unstable sternum such as pain and unpleasant movements even with minimal changing of the position of the body. Some of them previously underwent various interventions to repair the sternum and in the majority the sternum is almost completely destroyed (Figure 7) with a substantial gap and multiple fragments of broken wires.

The priority here is to ensure that the underlying disease is controlled and that the comorbidities of these patients are manageable.
The main principle of sternal reconstruction for sternal non-union is firm stabilisation. It is necessary to fill the sternal gap with healthy tissue and to stimulate bone regeneration. To minimise the risk of the procedure the interference behind the sternum should be avoided to prevent damage to the patent grafts or major anatomical structures in the heart. The main surgical steps of reconstruction of sternal non-union are exposure of the defect via the existing sternotomy scar with lateral mobilisation of pectoral muscle flaps. After that the sternotomy gap could be refreshed on the edges and all foreign bodies such as broken wires, detritus and non-viable tissue should be removed.
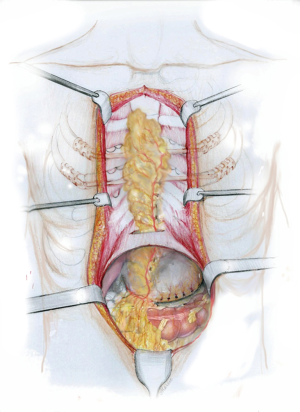
The bone graft could be harvested from the edge of the sternal defect with excising the edge of the sternum with an oscillating saw and bending them into the defect. Additionally, bone chips from the ribs and the xiphoid process should be harvested and placed into the sternal gap. After that the sternum should be reliably fixed with titanium bars (Figure 8). To improve the blood supply an omentoplasty would be an ideal step and for this reason laparotomy and harvesting of the greater omentum based on the right gastro-epiploic arcade is necessary. Harvesting of the greater omentum is performed in the usual fashion creating a flap adequate in size and dividing the vascular tributaries between the right gastro-epiploic arcade and the gastric wall. The harvested flap is transposed in front of the sternum via a window in the anterior portion of the diaphragm to decrease the risk of postoperative incisional hernia (Figure 9). Two vacuum drains should be placed.

Comments
After any complex chest wall reconstruction, patients may experience persistent pain, which is relatively rare and the rejection of foreign materials and late infection. In some situations, a persistent deformity could be seen and become a problem. The possibility of breaking or displacement of the bars should be kept in mind as well as the recurrence of tumour if surgery is performed in patients with cancer. For that reason, every patient after complex chest wall reconstruction require long term follow up. Particular attention should be paid to the development of new symptoms or a change of the existing symptoms. Options of redo surgery should always be kept in mind.
Conclusions
In general, modern techniques of chest wall resection and reconstruction expands the surgical options of patients with chest wall defects and reconstruction should always be considered as part of the treatment plan for patients. The operating team may include not only a thoracic surgeon, but other specialists as well depending on the local expertise, because a combination of surgical modalities is usually required.
Acknowledgments
This paper has been presented at “2 International Forum on Thoracic Surgery” 19-24 November 2019 Shanghai, China.
Funding: None.
Footnote
Conflicts of Interest: The author has completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/shc-20-26). The author has no conflicts of interest to declare.
Ethical Statement: The author is accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Informed consent was achieved from the patients for publication of this manuscript and any accompanying images.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Seder CW, Rocco G. Chest wall reconstruction after extended resection. J Thorac Dis. 2016;8:S863-71. [Crossref] [PubMed]
- Botianu PVH. Current indications for the intrathoracic transposition of the omentum. J Cardiothorac Surg 2019;14:103. [Crossref] [PubMed]
- Merritt RE. Chest Wall Reconstruction Without Prosthetic Material. Thorac Surg Clin 2017;27:165-9. [Crossref] [PubMed]
- McCormack P, Bains MS, Beattie EJ Jr, et al. New trends in skeletal reconstruction after resection of chest wall tumors. Ann Thorac Surg 1981;31:45-52. [Crossref] [PubMed]
- Ravitch MM. The Operative Treatment of Pectus Excavatum. Ann Surg 1949;129:429-44. [Crossref] [PubMed]
- Listewnik MJ, Jędrzejczak T, Majer K, et al. Complications in cardiac surgery: An analysis of factors contributing to sternal dehiscence in patients who underwent surgery between 2010 and 2014 and a comparison with the 1990-2009 cohort. Adv Clin Exp Med 2019;28:913-22. [Crossref] [PubMed]
Cite this article as: Anikin V. Principles of complex chest wall reconstruction. Shanghai Chest 2020;4:42.



