Annual report of thoracic surgery service at Shanghai Chest Hospital in 2021
Highlight box
Key findings
• The thoracic surgery team of Shanghai Chest Hospital overcame various challenges of the post-pandemic era and provided high-quality thoracic surgery service to patients with chest diseases.
What is known and what is new?
• The thoracic surgery team of Shanghai Chest Hospital has been publishing its annual report since 2018, summarizing the services and major progress over the last year.
• The services provided and progress made in 2021 by the thoracic surgery team of Shanghai Chest Hospital were reviewed, reflecting our constant effort to help our patients with high-standard services and state-of-the-art techniques.
What is the implication, and what should change now?
• The thoracic surgery team will continue to advance in the fields of lung surgery, esophageal surgery, mediastinal surgery, tracheal surgery, chest wall surgery and lung transplantation, improving skills and techniques as well as patient care in general in the upcoming year.
Introduction
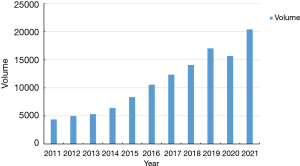
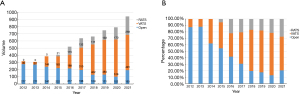
In 2021, the second year of the coronavirus disease 2019 (COVID-19) pandemic, the situation has been in good control with timely and effective prevention and control measures. The volume of thoracic services at Shanghai Chest Hospital, one of the largest tertiary referral centers for chest diseases in China, has largely recovered from the year 2020. Over the year of 2021, a total of 20,405 patients received thoracic surgeries at Department of Thoracic Surgery and Department of Oncological Surgery of Shanghai Chest Hospital (Figure 1). These included 17,829 pulmonary procedures, 1,113 esophageal procedures, 1,077 mediastinal procedures, 83 tracheal procedures, 76 chest wall procedures, 18 lung transplantations and 209 other procedures. This was the first time for the thoracic surgical volume of Shanghai Chest Hospital to exceed over 20,000 cases per year. In addition, with 18,909 cases carried out by minimally invasive surgery (MIS), the percentage of MIS was as high as 92.7% among all cases. Importantly, the volume of single-institution robotic-assisted thoracic surgery (RATS) exceeded 1,000 cases per year, up to 1,006 cases in 2021.
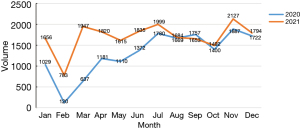
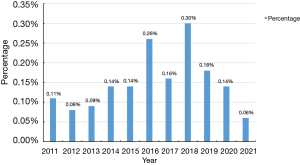
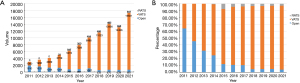
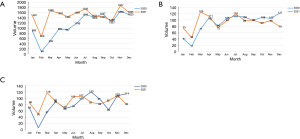
Under the circumstance of pandemic prevention and control measures, the volume of thoracic surgery has come back on track in the second half of the year 2020. In the first half year of 2021, the surgical volume in each month was higher than the corresponding month in 2020 (Figure 2). In addition to this increase in case volume, the thoracic team of Shanghai Chest Hospital kept improving the quality of clinical services. Average length of hospital stays (LOS) after thoracic surgery shortened continually, along with a low rate of perioperative complications and an extremely low in-hospital mortality rate of 0.06% (Figure 3).
With regard to the COVID-19 pandemic and the accompanying prevention and control measures, we retrospectively reviewed the efforts of the thoracic team from Shanghai Chest Hospital to cope with the challenges and opportunities these incurred on management of thoracic surgical patients.
Methods
Patients
Clinical data of patients who underwent thoracic surgeries between January 2021 and December 2021 at the Department of Thoracic Surgery and the Department of Oncological Surgery of Shanghai Chest Hospital were retrospectively collected. According to various conditions and surgical treatments, enrolled patients were divided into six categories, including pulmonary surgery, esophageal surgery, mediastinal surgery, tracheal surgery, chest wall surgery and lung transplantation. Numbers and percentages of surgical procedures and approaches, along with pathological subtypes were retrospectively collected and compared to data from the previous years. Perioperative outcomes including in-hospital mortality and postoperative LOS defined as the interval time between thoracic surgery to patient discharge were also retrospective collected. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). Ethical approval and individual consent for this retrospective analysis were not needed.
Statistical analysis
Categorical and continuous variables were presented as frequencies (percentages) and mean ± standard deviation (SD), respectively. Bar, line, and pie graphs were plotted and the statistical analysis was performed using the SPSS version 22.0 (IBM Corp., Armonk, NY, USA).
Results
Pulmonary surgery
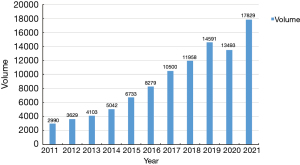
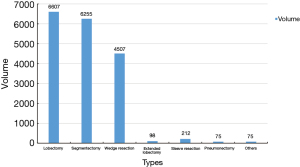
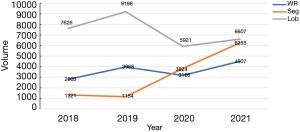
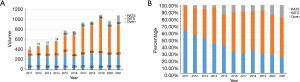
In 2021, the Division of Pulmonary Surgery in Shanghai Chest Hospital gradually walked out of the predicament of COVID-19 pandemic. This year saw the highest surgical volume for thoracic disorders in the history of the hospital. A total of 17,829 patients underwent pulmonary surgeries, an increase of 32.1% from the previous year (Figure 4). Among them, 16,631 patients (93.3%) received video-assisted thoracic surgery (VATS), 517 patients (2.9%) received RATS resections, and 681 patients (3.8%) received open thoracotomies (Figure 5A,5B). Both VATS and RATS resections reached the historical heights in the past decades. A total of 15,686 cases (88.0%) were diagnosed as malignant diseases and 2,143 cases (12.0%) were benign diseases. The rate of pulmonary malignancy was similar to the previous year. The most common type of surgical procedure was lobectomy (n=6,607, 37.1%), closely followed by segmentectomy (n=6,255, 35.1%) and wedge resection (n=4,507, 25.3%). A small but not insignificant proportion of patients still had to received extended resections including sleeve lobectomy (n=212, 1.2%), bilobectomy (n=98, 0.5%), pneumonectomy (n=75, 0.4%) and others (n=75, 0.4%) (Figure 6).
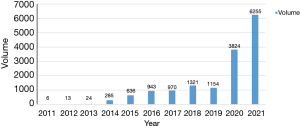
With the use of computed tomography (CT) screening especially for COVID-19, early-stage non-small cell lung cancers (NSCLCs), especially those appearing as ground glass opacity (GGO) are increasingly detected. Comparing with the past four years up to 2019, the volume of standard lobectomy has decreased by over 30.0%. At the same time, the volume of anatomical segmentectomy has increased by nearly 4.4 times compared to 2019. Over the past ten years, the number of segmentectomy was rapidly increasing from only 6 cases in 2011 to 6,255 cases in 2021 (Figure 7). While the number of wedge resection was comparable to the previous two years (Figure 8), the combined volume of sublobar resections had surpassed that of standard lobectomy for the first time in 2020, and continued to increase in 2021.
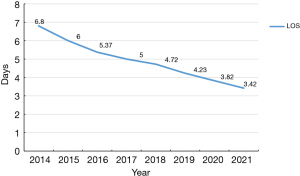
For the postoperative outcomes, average LOS after pulmonary surgeries shortened steadily over the past 7 years, from 6.80 to 3.42 days (Figure 9). There were two major reasons for this continuously decreasing LOS. On the one hand, recovery from thoracic surgery was significantly fastened by the increasing use of MIS techniques. Patients who underwent MIS had an average LOS of 3.28 days. On the other hand, sublobar resections has become the dominant part of routine practice. LOS after sublobar resections was only 2.92 days on average. The lesser resection extents also contributed to a better recovery and shorter hospital stay.
Apart from MIS for early-stage NSCLC, the thoracic team of Shanghai Chest Hospital also focused on the complicated pulmonary surgeries, especially those for locally advanced NSCLC after induction therapies. Average LOS for those complicated surgeries including sleeve resection, extended lobectomy, pneumectomy were only 7.62 days, indicating a safe recovery and a low rate of postoperative complications due to the highly developed surgical skills and outstanding work of peri-operative care.
Esophageal surgery
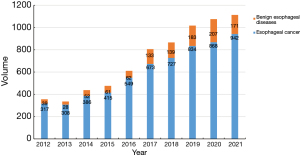
The Division of Esophageal Surgery of Shanghai Chest Hospital overcame the impact of COVID-19 pandemic, and made a 3.5% increase in surgical volume in the past year.
A total of 1,113 patients had esophageal procedures performed in the year 2021, including 942 patients diagnosed as esophageal cancer and 171 patients diagnosed as benign esophageal diseases (Figure 10). The percentage increase of total esophageal procedures and esophageal cancer resections were up to 3.5% and 8.5% compared with the previous year of 2020, respectively. Among the 942 esophagectomies for esophageal carcinoma, rate of minimally invasive esophagectomy (MIE) accounted for about 79.5%, with 491 (52.1%) VATS and 258 (27.4%) RATS esophagectomies (Figure 11A). Both the total number and the rate of RATS esophagectomy have increased steadily since 2015 (Figure 11B).
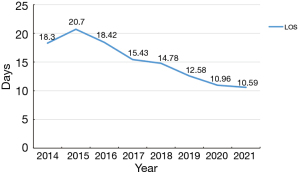
In-hospital mortality rate of esophageal procedures was as low as 0.27%. Average length of LOS after esophageal surgeries was shortened to 10.59 days (Figure 12). In detail, average LOS for esophageal carcinoma was 11.2 days and average LOS for benign esophageal diseases was only 6.89 days.
Mediastinal surgery
Albeit routine pandemic preventions and controls, surgical volume of mediastinal procedures again exceeded 1,000 cases in 2021 for the second time in history since the year 2019. In comparison to the prior year, the total mediastinal surgery volume increased by over 11.1%. Of the 1,077 patients who underwent mediastinal procedures, 680 (63.1%) were diagnosed as mediastinal malignancies and 397 (36.9%) were benign diseases. Specifically, 622 patients (57.8%) received VATS procedures, 197 patients (18.3%) received RATS procedures and 258 patients (23.9%) received open procedures (Figure 13A,13B). The volume of RATS for mediastinal surgeries reached a historical height with an increase of almost 46% comparing to the year 2020. No in-hospital mortality ever occurred during the postoperative period of mediastinal surgeries. In the meantime, average LOS after mediastinal surgery has been continuingly shortened from 5.80 days in 2018 to 3.92 days in 2021 (Figure 14).
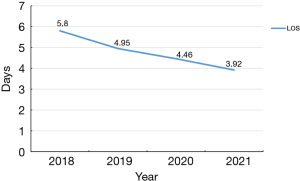
In addition to the increased surgical volume, there has also been a major shift in the model for diagnosis and treatment of mediastinal diseases. In September 2021, a multidisciplinary treatment (MDT) ward for mediastinal diseases was officially established. This one-stop approach to treating complicated mediastinal diseases not only ensured the precision and efficacy of treatment, but also provided convenience for the patients. What is more, the Division of Mediastinal Surgery of Shanghai Chest Hospital firstly proposed a novel strategy of superior vena cava reconstruction under the guidance of internal jugular vein pressure monitoring. This reconstruction strategy was applied to the resection of mediastinal tumors invading the great blood vessels. This easily generalizable measure could help shorten the operation time, reduce the intraoperative trauma and risk, and thus leading to a better recovery and outcomes after such complicated procedures.
Tracheal surgery, chest wall surgery and lung transplantation
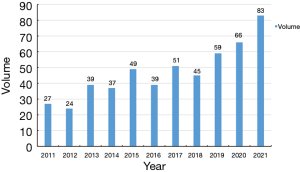
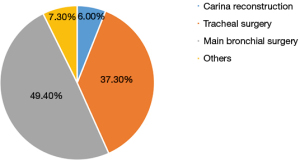
As one of the tracheal surgery birthplaces in China, the Division of Tracheal Surgery of Shanghai Chest Hospital has maintained a large volume of tracheal procedures and has always made contributions to the complicated bronchial and tracheal surgeries. In 2021, a total of 83 tracheal procedures were successfully performed, representing a 25.8% increase over the previous year (Figure 15). Among them, 41 (49.4%) received main bronchial surgeries, 31 (37.3%) received tracheal surgeries, 5 (6.0%) received carina resection and reconstruction and 6 (7.3%) received other procedures (Figure 16). The average LOS after tracheal surgery was 6.8 days, an almost 37.0% drop from 2020. No in-hospital mortality was observed.
In 2021, a specialized service for diseases of chest wall was established in the Department of Thoracic Surgery. A total of 76 patients with chest wall diseases received surgical treatment in the past year. There were 18 patients with chest wall deformities (16 funnel chests and 2 pigeon chests) and 58 with chest wall tumors (34 benign tumors and 24 malignancies). Average LOS for chest wall procedures was 3.50 days. In particular, average LOS was 2.44 days for chest wall deformity and 3.83 days for chest wall tumor. No in-hospital mortality occurred in the previous year.
Different from the first year of COVID-19 pandemic, volume of lung transplantations also increased. A total of 18 patients received lung transplantations in 2021. Among them, 11 patients received single-lung transplantation and 7 patients received double-lung transplantation. Average LOS for lung transplantations was 32.69 days, being 31 days for single-lung transplantation and 38.3 days for double-lung transplantation. Three patients died after single-lung transplantations and no mortality occurred in patients receiving double-lung transplantations. In-hospital mortality rate for lung transplantation was 16.7%.
Discussion
The thoracic surgery team of Shanghai Chest Hospital has been publishing its annual reports to the public since the year 2017. Summarized in these reports are the major achievements made in the past year, in addition to an overview of the statistics of surgical services at Shanghai Chest Hospital.
Shanghai Chest Hospital is one of the largest thoracic surgery centers in China. Its annual volume in thoracic surgery has exceeded over 10,000 cases since 2016. Facing the great impact of COVID-19 pandemic in the year of 2020, the number of thoracic surgeries was largely truncated, especially for pulmonary surgeries in the first half year owing to the stringent strategies of pandemic prevention and control measures (Figure 2). Fortunately, great efforts were made by the staff at Shanghai Chest Hospital and routine thoracic surgery service gradually returned to normal and even showed a steady increase during the second half of year 2020 (1). In 2021, the thoracic team of Shanghai Chest Hospital continued to overcome the heavy burden bought on by the pandemic and provided uncompromised medical care for those in need even in the hardest of times. To the best of our knowledge, under the various circumstances of COVID-19, Shanghai Chest Hospital was one of the only two thoracic centers that treated a historically high number of over 20,000 cases of thoracic disease patients requiring surgery in 2021 around the whole world.
In 2021, number of pulmonary surgeries showed a significant increase, up to 24% compared with the previous year. By comparing the monthly case volumes of 2020 and 2021, the largest increase in volume of pulmonary surgery occurred during the first half year of 2021, especially in February, March and April (Figure 2 and Figure 17A). This was mainly owing to the widespread use of CT scan for COVID screening, incidentally leading to a large number of pulmonary nodules especially GGO detected. In addition, pulmonary surgeries for small-sized and GGO lesions were largely postponed. And non-local patients were deterred from seeking medical services in Shanghai due to the stringent prevention and control measures of the previous year (1). With the COVID policies loosening up, those patients whose surgeries had been postponed and who were non-local gradually came back to Shanghai Chest Hospital in the year 2021. As for esophageal surgery and mediastinal surgery, the increase in volume was not as prominent as pulmonary surgery (Figure 17B,17C). This phenomenon, in a way, reflected the stable incidence rates of esophageal and mediastinal disease. It also indicated that the more urgent thoracic surgeries for esophageal carcinoma and mediastinal tumors were not affected by the pandemic or corresponding policies. Besides, under such a great burden of thoracic surgery volume, no patient or medical staff was ever infected by COVID, as long as the regular prevention and control measures were adhered to during the routine clinical works.
The percentage of MIS in 2021 was up to 92.7%, 1.6% higher than that in 2020; and the rate of MIS for pulmonary surgeries was as high as 96.3%. For early stage Ia lung cancers, there has been a consistent debate over surgical resection extent (2). Recently, a series of clinical trials have suggested an oncological non-inferiority or even a superiority of sublobar resections for GGO-containing NSCLCs, including the Japan Clinical Oncology Group (JCOG) 0802, JCOG 0804, JCOG 1211 and Cancer and Leukemia Group B 140503 (CALGB 140503) (3-5). Based on the evidence provided by these trials, indications for sublobar resections have been changed from a compromised procedure for high-risk patients to an intentional procedure for selected patients with early-stage GGO-containing NSCLC. At Shanghai Chest Hospital, such a change is echoed in our clinical practices and can be seen from the increasing number of sublobar resections, especially anatomical segmentectomy, over the years. In 2021, more than 6,000 patients received anatomical segmentectomy at Shanghai Chest Hospital, which was nearly twice in comparison with the previous year and six times higher than that of the year 2019. In addition, the number of wedge resections was more than 4,500 cases, an almost 40.0% increase compared to 2020. The total number of sublobar resections amounted to over 10,000 in 2021 and its annual increase from 2020 was prominent while the increase in volume of lobectomy was modest. Sublobar resections have been gradually replacing lobectomy as the first choice for patients with peripheral small-sized lung cancers in our routine clinical practice. Along with other 18 tertiary referral centers in China, Shanghai Chest Hospital has been leading a prospective controlled randomized phase III trial to investigate the minimally invasive segmentectomy versus lobectomy for GGO-containing early-stage invasive lung adenocarcinoma (the GREAT trial) since 2020. At the end of 2021, the GREAT trial had successfully achieved more than 1/3 of its estimated enrollment nationwide and we truly hope that this trial could further prove the superiority of minimally invasive segmentectomy and benefit more patients with early-stage lung cancers.
Even under the heavy burden of COVID-19 pandemic, the quality of our thoracic surgery service remained uncompromised and well-guaranteed. The average LOS after pulmonary surgeries was shortened to 3.42 days in 2021, which was almost half of that in the year of 2014. According to our previous study, 93% of wedge resection, nearly 80% of segmentectomy and more than 60% of lobectomy patients could be discharged within 48 hours after surgery at Shanghai Chest Hospital. The average LOS after esophageal and mediastinal surgeries was also shortened comparing with the previous year. Such shortening in LOS indicated the excellent implementation of enhanced recovery after surgery (ERAS) in thoracic surgery, made possible by the joint efforts of the Department of Anesthesiology and the Department of Nursing. In addition, good perioperative outcomes and low rate of complications also reflected the well-developed surgical skills and cutting-edge techniques here at Shanghai Chest Hospital.
There were several limitations in this research. First, the clinical epidemiology, differences or decreases were demonstrated as the rates of outcomes or the length of stay, but not after the statistical analysis. Second, in-hospital mortality was not a 100% valid surrogate of the risk of surgical procedures instead of the 30-day and 90-day mortality. Therefore, those limitations will be overcame in future annual report.
In the upcoming year, the thoracic surgery team of Shanghai Chest Hospital will continue to overcome various challenges of the post-pandemic era and provide high-quality thoracic surgery service to patients with chest diseases. The thoracic surgery team will quicken the pace in the transformation from clinically-focused to more translational-related practice. In detail, the main focus for pulmonary surgery remains on providing precise and personalized care for early-stage and locally-advanced NSCLC patients through carefully designed clinical studies in MIS and induction therapies followed by surgery. Also, day-surgery for thoracic diseases has also started based on the ideology of ERAS. In esophageal surgery, we will continue to provide the best of care for our patients from diagnosis to treatment, including endoscopic diagnosis and treatment, as well as neoadjuvant therapy in addition to esophagectomy for advanced diseases. In mediastinal surgery, we will keep providing cutting-edge surgical skills for more patients, promoting clinical trials on novel therapies for locally advanced and late-stage thymic tumors. Last but not the least, we will continue to advance in the fields of tracheal surgery, chest wall surgery and lung transplantation, improving skills and techniques as well as patient care in general.
Acknowledgments
Funding: None.
Footnote
Data Sharing Statement: Available at https://shc.amegroups.com/article/view/10.21037/shc-23-2/dss
Peer Review File: Available at https://shc.amegroups.com/article/view/10.21037/shc-23-2/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://shc.amegroups.com/article/view/10.21037/shc-23-2/coif). QL serves as an unpaid Associate Editor-in-Chief of Shanghai Chest. WF serves as an unpaid Executive Editor-in-Chief of Shanghai Chest. The other authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). Ethical approval and individual consent for this retrospective analysis were not needed.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Wang Y, Zhang Y, Bao F, et al. The Feasibility and Safety of Routine Thoracic Surgeries in the Low-Risk Areas During the Coronavirus Disease 2019 Pandemic. JTO Clin Res Rep 2021;2:100144. [Crossref] [PubMed]
- Cheng X, Onaitis MW, D'amico TA, et al. Minimally Invasive Thoracic Surgery 3.0: Lessons Learned From the History of Lung Cancer Surgery. Ann Surg 2018;267:37-8. [Crossref] [PubMed]
- Saji H, Okada M, Tsuboi M, et al. Segmentectomy versus lobectomy in small-sized peripheral non-small-cell lung cancer (JCOG0802/WJOG4607L): a multicentre, open-label, phase 3, randomised, controlled, non-inferiority trial. Lancet 2022;399:1607-17. [Crossref] [PubMed]
- Altorki NK, Wang X, Wigle D, et al. Perioperative mortality and morbidity after sublobar versus lobar resection for early-stage non-small-cell lung cancer: post-hoc analysis of an international, randomised, phase 3 trial (CALGB/Alliance 140503). Lancet Respir Med 2018;6:915-24. [Crossref] [PubMed]
- Suzuki K, Watanabe SI, Wakabayashi M, et al. A single-arm study of sublobar resection for ground-glass opacity dominant peripheral lung cancer. J Thorac Cardiovasc Surg 2022;163:289-301.e2. [Crossref] [PubMed]
Cite this article as: Wang Y, Gu Z, Yao F, Mao T, Wang R, Sun Y, Li Z, Yang J, Tan Q, Luo Q, Fang W. Annual report of thoracic surgery service at Shanghai Chest Hospital in 2021. Shanghai Chest 2023;7:15.