This article has an erratum available at: http://dx.doi.org/10.21037/shc.2018.05.02 the article has been update on 2018-05-04 at here.
Annual report of Department of Thoracic Surgery at Shanghai Chest Hospital
Introduction
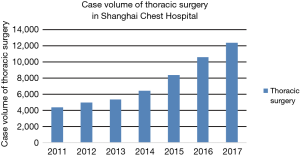
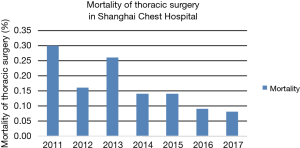
The Department of Thoracic Surgery in Shanghai Chest Hospital is the largest thoracic center in China with the most complete spectrum of diseases and disorders. In recognition of the departmental skill and expertise, it is considered a national key clinical discipline. Along those lines, and in order to further improve outcomes, the Thoracic Surgery Department was one of the earliest departments in China to carry out standardized surgery treatment for thoracic cancer. The Department was awarded second place in the list of national best specialists in 2014, 2015 and 2016 consecutively. The amount of thoracic surgery has exceeded 10,000 cases since 2016 (Figure 1) and peri-operative mortality of thoracic surgery was extremely low: 0.09% in 2016 and 0.08% in 2017 (Figure 2).
In a move to further improve outcomes, since June 2015 the Department of Thoracic Surgery at Shanghai Chest Hospital has been evolving into several thoracic sub-specialties, including lung, esophagus, mediastinum, trachea, and transplantation. The Department of Esophageal Surgery has formed distinctive clinical programs, containing minimally invasive surgical treatment, complex esophageal surgery, endoscopic interventional therapy and one-stop multi-disciplinary service. The annual operational cases of mediastinal surgery are increasing, especially for thymic surgery, where Shanghai Chest has the highest case volume in the world. In keeping with international trends, and leading the way in China, the proportion of minimally invasive surgery continues to increase within our department. New technologies continue to develop, and the success of minimally invasive preoperative diagnosis is improving. The field of advanced tracheal surgery continues to grow with more than 50 tracheal disease patients admitted each year to Shanghai Chest.
Section of Lung Surgery
High-volume center for lung surgery
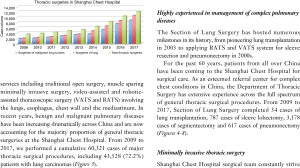
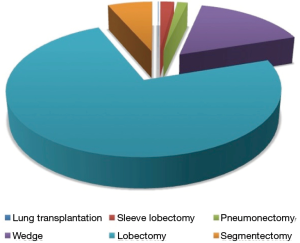
The Department of Thoracic Surgery offers a full range of services including traditional open surgery, muscle sparing minimally invasive surgery, video-assisted and robotic-assisted thoracoscopic surgery (VATS and RATS) involving the lungs, esophagus, chest wall and the mediastinum. In recent years, benign and malignant pulmonary diseases have been increasing dramatically across China and are now accounting for the majority proportion of general thoracic surgeries at the Shanghai Chest Hospital. From 2009 to 2017, we performed a cumulative 60,321 cases of major thoracic surgical procedures, including 43,528 (72.2%) patients with lung carcinomas (Figure 3).
Highly experienced in management of complex pulmonary diseases
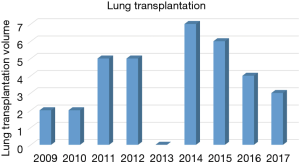
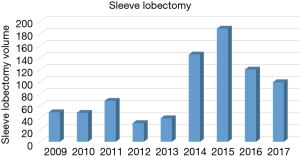
The Section of Lung Surgery has hosted numerous milestones in its history, from pioneering lung transplantation in 2003 to applying RATS and VATS system for sleeve resection and pneumonectomy in 2000s.
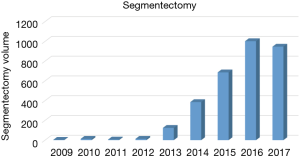
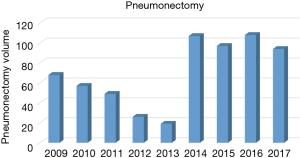
For the past 60 years, patients from all over China have been coming to the Shanghai Chest Hospital for surgical care. As an esteemed referral center for complex chest conditions in China, the Department of Thoracic Surgery has extensive experience across the full spectrum of general thoracic surgical procedures. From 2009 to 2017, Section of Lung Surgery completed 34 cases of lung transplantation, 787 cases of sleeve lobectomy, 3,178 cases of segmentectomy and 617 cases of pneumonectomy (Figures 4-8).
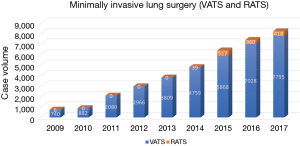
Minimally invasive thoracic surgery
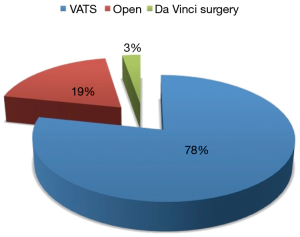
Shanghai Chest Hospital surgical team constantly strive to investigate and incorporate the latest techniques in minimally invasive surgery, from muscle sparing thoracotomy to VATS and RATS, for management of pulmonary diseases. Among the 43,528 lung carcinoma resections in the past 9 years, 33,952 (78%) were fulfilled by VATS resection and 1,306 (3%) by robot (Figures 9,10). In 2015, the first robot-assisted sleeve lobectomy for lung cancer in China was successfully completed here. To date, 23 patients with complex centrally located lung cancer have received this minimal invasive procedure.
Our mission
Our mission is to offer outstanding surgical care with an individualized approach. By utilizing the state-of-the-art facilities and technology, such as VATS and robotic systems, we will never cease in our goal to deliver the most up-to-date surgical techniques and care available in the world. We are also committed to improve the standard of care through cutting-edge clinical studies and translational research and state of the art medical and surgical education.
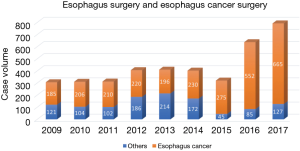
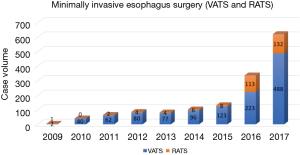
Section of Esophageal Surgery
A total of 792 cases of esophageal resections were completed in 2017. With the increasing number of early stage esophageal cancer being detected, the goal of an “all in one” endoscopy—thoracoscopy and laparoscopy—robot platform to manage these patients was established. The goal was to offer minimally invasive approaches to carry out individualized surgical treatment for our patients. For early superficial lesions, endoscopic diagnosis, staging, and resection have become the standard of care at Shanghai Chest. For locally advanced disease, minimally invasive surgery represented by total thoracoscopic-laparoscopic esophagectomy has been increasing rapidly in the past few years and has gradually become the mainstay of all resections. Now its use has been extended into patients with locally advanced diseases after successful induction therapies prior to surgery. With the addition of robot-assisted minimally invasive esophagectomy, we have brought the most advanced technology for esophageal cancer resection in the world to Shanghai Chest and its patients. After successfully completed the first case of robot-assisted esophagectomy in China in 2010, Shanghai Chest Hospital has completed the largest number of these procedures in China. In total, 132 cases were accomplished in 2017 (Figures 11,12).
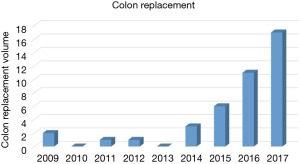
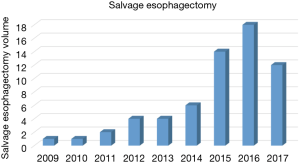
As one of the top-level service providers in China, the esophageal surgery division strives to provide individualized management of complex and difficult disease with extensive group experience, multi-disciplinary teams, and outstanding surgical and endoscopic techniques. Examples of innovations include the use of free jejunal interposition for benign cervical strictures of the esophagus in the attempt to preserve normal anatomy and function of the digestive tract, use of colon replacement/interposition for patients with cervical esophageal cancer and/or previous history of gastric surgery, and salvage esophagectomy for recurrent or persistent disease after definitive chemoradiotherapy (Figures 13,14).
As the leading unit in Jiao Tong University Clinical Center for Esophageal Diseases, a multidisciplinary team (MDT) for diagnosis and treatment of esophageal cancer was established in 2010. A team uniting members of surgery, radiotherapy, medical oncology, radiology, pathology, endoscopy, and nursing care, the MDT discussion takes place at regular intervals, providing individualized and standardized therapeutic strategy for esophageal cancer patients.
For patients with locally advanced disease, neoadjuvant therapy including chemotherapy and concurrent chemoradiation are delivered to increase the radical resection rate and to improve long-term outcomes. Clinical trials are also ongoing to investigate the safety and effectiveness of various adjuvant therapies after surgery. These include a multi-center phase III trial of adjuvant therapies or surgery alone for high-risk pN0 esophageal cancer (NCT02891083), and comparison of robot-assisted minimally invasive esophagectomy versus open surgery in patients with locally advanced esophageal cancer after neoadjuvant chemoradiotherapy (17411971200), comparative of robot assisted minimally invasive esophagectomy and thoracoscopic-laparoscopic esophagectomy for esophageal cancer.
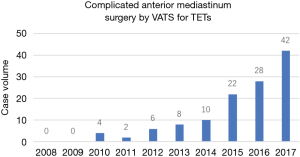
Section of Mediastinum Surgery
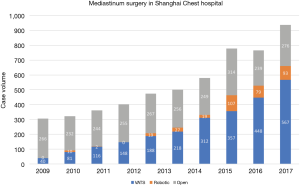
Numerous benign or malignant disorders occur within the mediastinum, including conditions pertinent to the primary structures, diseases extending from neighboring organs, or lesions manifesting systemic changes of the body. Figure 15 highlights the development of mediastinum surgery in Shanghai Chest hospital over the last decade. The total number of major procedures completed during 2008 to 2017 in mediastinal surgery has reached 5,449 cases. Minimally invasive surgical techniques, such as VATS and robotic surgery have been increasing very rapidly, along with a decrease in open procedures in recent years. In the Shanghai Chest surgical database, the number of minimally invasive procedures had exceeded open procedure since 2014. In 2017, VATS and robotic procedure were performed in 567 and 93 patients, which accounted for 60.6% and 9.9% of the total number of annual cases respectively. In addition to benign lesions and early stage malignancies, minimally invasive surgery has been increasingly applied in patients with locally advanced diseases even after induction therapies, as well as those with recurrent diseases. This has led to better patient recovery and improved quality of life and functional status after surgery.
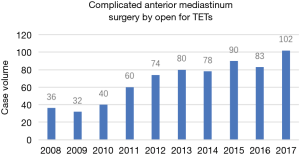
Locally advanced mediastinum tumor patients with complicated surgery (including vascular reconstruction or replacement, partial cardiac resection, lobectomy, giant mediastinal tumor resection, etc.) continue to increase (Figures 16,17).
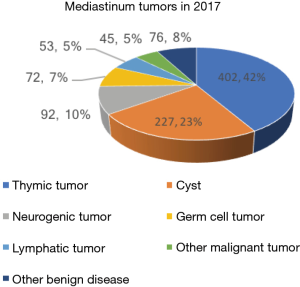
Among the 936 mediastinal lesions resected in 2017, there were 402 thymic epithelial tumors, followed by 275 cysts, 92 neurogenic tumors, 72 germ cell tumors, and 53 lymphatic tumors (Figure 18).
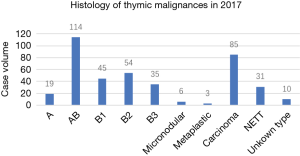
Histological analysis revealed 276 thymomas (19 of type A, 114 of type AB, 45 of type B1, 54 of type B2, 35 of type B3, 6 of micronodular thymoma, 3 of metaplastic thymoma), 85 thymic carcinomas, 31 neuroendocrine thymic tumors (NETT) and 10 unknown types (Figure 19).
Thanks to the joint effort from an outstanding multi-disciplinary team, comprehensive and evidence-based multi-modality approach has helped our patients with advanced mediastinal tumors. By employing induction chemoradiation, extensive surgical procedures such as superior vena cava bypass and pleurectomy together with intrapleural thermo-chemotherapy, and hemi-thorax pleural irradiation, a satisfactory control rate has been achieved in stage III–IV thymic diseases.
Section of Tracheal Surgery
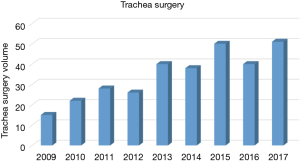
Shanghai Chest Hospital is the leading center for tracheal surgery in China and a constant innovator in this challenging area (Figure 20). Total number of trachea and bronchial surgery cases was 51 in 2017. These included trachea surgeries in 40 cases, main bronchial surgery in six cases, and carina resection and reconstruction in five cases.
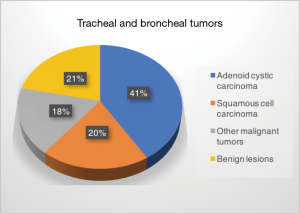
The disease spectrum included benign and malignant lesions in the trachea, main bronchus, and at the carina, with the majority of cases being malignant tumors. Among the tracheal and main bronchial malignancies, the most common types are adenoid cystic carcinoma (21 cases) and squamous cell carcinoma (ten cases). The other nine cases of primary malignant tumors were mucinous adenocarcinoma, adenosquamous carcinoma, small cell carcinoma, leiomyosarcoma, myoepithelioma, epithelial-myoepithelial carcinoma, mucosa-associated lymphoid tissue (MALT) lymphoma, lymphoepithelioma-like carcinoma, and metastatic thyroid papillary carcinoma. In 11 cases the lesion was benign, including airway stenosis after trauma, leiomyoma, and mucous gland adenoma (Figure 21).
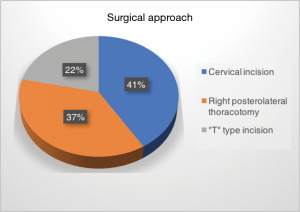
Airway resection and reconstruction is an extremely complicated surgery and requires the ability to use multiple different surgical approaches. Individualized surgical approach for optimal exposure is therefore critically important for such procedures. Based on the imaging studies and bronchoscopy examination, right posterolateral thoracotomy was adopted in 19 cases, including four complex reconstructions in patients with tumor invading the carina. Cervical incision was used in 21 cases. Addition of partial sternotomy was required in 11 cases to ensure radical resection and successful reconstruction (Figure 22). In two patients with difficult airway because of nearly complete tumor blockage of the tracheal lumen, extracorporeal circulation was introduced so as to assure the safety of surgery.
Research: current studies
- Xufeng Guo. Comparison of robot assisted minimally invasive esophagectomy versus open surgery in patients with locally advanced esophageal cancer after neoadjuvant chemoradiotherapy. Shanghai Science and Technology Committee;
- Wentao Fang. A prospective multicenter randomized controlled clinical test for the comparison of postoperative adjuvant chemotherapy and adjuvant radiotherapy versus surgical treatment alone for high-risk pN0 thoracic esophageal squamous cell carcinoma. Three years of clinical innovation action plan;
- Zhigang Li. A prospective multicenter open randomized controlled study of comparative of robot assisted minimally invasive esophagectomy and thoracoscopic-laparoscopic esophagectomy for esophageal cancer. Three years of clinical innovation action plan;
- Heng Zhao. Diagnosis and surgical treatment of small pulmonary nodules guided by imaging and genealogy. Three years of clinical innovation action plan;
- Limin Fan. The study of disposable thoracic drainage device. Three years of clinical innovation action plan;
- Rui Wang. A model for predicting the properties of pulmonary nodules by imaging and molecular characteristics. Shanghai health and family planning system training program for outstanding young medical faculty;
- Bo Ye. Artificial intelligence CT screening for early lung cancer. Shanghai Jiao Tong University;
- Xufeng Guo. Comparative study of robotic minimally invasive surgery and open surgery for local advanced esophageal carcinoma after neoadjuvant chemoradiotherapy. Shanghai Charity Foundation;
- Chenxi Zhong. The function and mechanism of feedback loop formed by HMGCR and c-Myc in esophageal squamous cell carcinoma. National Natural Science Foundation;
- Bo Ye. The Function and regulation mechanism of KIT gene in thymus cancer. National Natural Science Foundation;
- Jianxin Shi. The function of intermediary complex subunit MED23 in non-small cell lung cancer and its role in regulation of beta-catenin/TCF signaling. National Natural Science Foundation;
- Feng Yao. Regulatory effect of lung cancer suppressor gene GPRC5A on STAT3 signaling pathway. National Natural Science Foundation;
- Xinghua Cheng. Using CRISPR technique to explore the effect and mechanism of Nrf2 anti-oxidant pathway in hypoxia-induced metastasis of lung cancer. National Natural Science Foundation;
- Rui Wang. Identification and functional mechanism of driver mutation of MET in non-small cell lung cancer. Shanghai Rising-Star Program;
- Qingquan Luo. Prospective randomized controlled test on artificial intelligence and standard thoracotomy in the treatment of N2 non-small cell lung cancer. Shanghai Municipal Commission of Health and Family Planning;
- Wen Gao. Study on path of diagnosis and treatment of solitary pulmonary nodules. Shanghai Municipal Science and Technology Committee;
- Heng Zhao. Biomarker study of immune related glycoprotein glycoforms in serum of lung GGN patients. Shanghai Jiao Tong University.
Publications
- Pan X, Gu C, Wang R, et al. Transmanubrial osteomuscular sparing approach for resection of cervico-thoracic lesions. J Thorac Dis 2017;9:3062-8. [Crossref] [PubMed]
- Zhao Y, Gu H, Fan L, et al. Comparison of clinical features and survival between thymic carcinoma and thymic carcinoid patients. Eur J Cardiothorac Surg 2017;52:33-8. [Crossref] [PubMed]
- Zhou C, Zhao J, Shao J, et al. Prognostic relevance of TTF-1 expression in stage I adenocarcinoma. Oncotarget 2017;8:107462-8. [Crossref] [PubMed]
- Guo X, Ye B, Yang Y, et al. Impact of unplanned events on early postoperative results of minimally invasive esophagectomy. Thorac Cancer 2018;9:94-8. [Crossref] [PubMed]
- Yuan Y, Huang Q, Gu C, et al. Disease-free survival improved by use of adjuvant EGFR tyrosine kinase inhibitors in resectable non-small cell lung cancer: an updated meta-analysis. J Thorac Dis 2017;9:5314-21. [Crossref] [PubMed]
- Yang Y, Gao W, Ding X, et al. Variations within 3'-UTR of MDM4 gene contribute to clinical outcomes of advanced non-small cell lung cancer patients following platinum-based chemotherapy. Oncotarget 2017;8:16313-24. [PubMed]
- Luo J, Wang R, Han B, et al. Solid predominant histologic subtype and early recurrence predict poor postrecurrence survival in patients with stage I lung adenocarcinoma. Oncotarget 2017;8:7050-8. [PubMed]
- Wang Y, Wang R, Zheng D, et al. Predicting the recurrence risk factors and clinical outcomes of peripheral pulmonary adenocarcinoma ≤3 cm with wedge resection. J Cancer Res Clin Oncol 2017;143:1043-51. [Crossref] [PubMed]
- Wang Y, Wang R, Zheng D, et al. The indication of completion lobectomy for lung adenocarcinoma ≤3 cm after wedge resection during surgical operation. J Cancer Res Clin Oncol 2017;143:2095-104. [Crossref] [PubMed]
- Gu C, Wang R, Pan X, et al. Comprehensive study of prognostic risk factors of patients underwent pneumonectomy. J Cancer 2017;8:2097-103. [Crossref] [PubMed]
- Gu C, Wang R, Pan X, et al. Sublobar resection versus lobectomy in patients aged ≤35 years with stage IA non-small cell lung cancer: a SEER database analysis. J Cancer Res Clin Oncol 2017;143:2375-82. [Crossref] [PubMed]
- Gu C, Pan X, Chen Y, et al. Short-term and mid-term survival in bronchial sleeve resection by robotic system versus thoracotomy for centrally located lung cancer. Eur J Cardiothorac Surg 2018;53:648-55. [Crossref] [PubMed]
- Fan L, Yang H, Yao F, et al. Clinical outcomes of epidermal growth factor receptor tyrosine kinase inhibitors in recurrent adenosquamous carcinoma of the lung after resection. Onco Targets Ther 2017;10:239-45. [Crossref] [PubMed]
- Zhang X, Yang Y, Ye B, et al. Minimally invasive esophagectomy is a safe surgical treatment for locally advanced pathologic T3 esophageal squamous cell carcinoma. J Thorac Dis 2017;9:2982-991. [Crossref] [PubMed]
- Pan WB, Li HX, Zheng JH, et al. Comparison of larynx-preserving esophagectomy and definitive chemoradiotherapy for patients with cervical esophageal squamous cell carcinoma. Int J Clin Exp Med 2017;10:13687-94.
- Fang W, Fu J, Shen Y, et al. Management of thymic tumors-consensus based on the Chinese Alliance for Research in Thymomas Multi-institutional retrospective studies. J Thorac Dis 2016;8:641-5. [Crossref] [PubMed]
- Gu Z, Fu J, Shen Y, et al. Thymectomy versus tumor resection for early-stage thymic malignancies: a Chinese Alliance for Research in Thymomas retrospective database analysis. J Thorac Dis 2016;8:680-6. [Crossref] [PubMed]
- Yao F, Yang H, Zhao H. Single-stage bilateral pulmonary resections by video-assisted thoracic surgery for multiple small nodules. J Thorac Dis 2016;8:469-75. [Crossref] [PubMed]
- Sun Y, Yang Y, Chen Y, et al. Translocation of left inferior lobe pulmonary artery to the pulmonary artery trunk for central type non-small cell lung cancers. J Thorac Dis 2016;8:826-32. [Crossref] [PubMed]
- Ye B, Zhong CX, Yang Y, et al. Lymph node dissection in esophageal carcinoma: Minimally invasive esophagectomy vs open surgery. World J Gastroenterol 2016;22:4750-6. [Crossref] [PubMed]
- Zhao Y, Shi J, Fan L, et al. Evaluation of the proposed International Association for the Study of Lung Cancer (IASLC)/International Thymic Malignancies Interest Group (ITMIG) staging revisions in thymic well-differentiated neuroendocrine carcinoma patients. Eur J Cardiothorac Surg 2016;49:569-73. [Crossref] [PubMed]
- Zhao Y, Shi J, Fan L, et al. Surgical treatment of thymoma: an 11-year experience with 761 patients. Eur J Cardiothorac Surg 2016;49:1144-9. [Crossref] [PubMed]
- Jiang WY, Wang R, Pan XF, et al. Clinicopathological features and prognosis of primary pulmonary lymphoepithelioma-like carcinoma. J Thorac Dis 2016;8:2610-6. [Crossref] [PubMed]
- Pan X, Gu C, Wang R, et al. Initial Experience of Robotic Sleeve Resection for Lung Cancer Patients. Ann Thorac Surg 2016;102:1892-7. [Crossref] [PubMed]
- Luo J, Wang R, Han B, et al. Analysis of the clinicopathologic characteristics and prognostic of stage I invasive mucinous adenocarcinoma. J Cancer Res Clin Oncol 2016;142:1837-45. [Crossref] [PubMed]
- Luo J, Huang Q, Wang R, et al. Prognostic and predictive value of the novel classification of lung adenocarcinoma in patients with stage IB. J Cancer Res Clin Oncol 2016;142:2031-40. [Crossref] [PubMed]
- Zhao W, Fang W. Giant thymoma successfully resected via hemiclamshell thoracotomy: a case report. J Thorac Dis 2016;8:E677-80. [Crossref] [PubMed]
- Yang H, Yao F, Tantai J, et al. Resected Tracheal Adenoid Cystic Carcinoma: Improvements in Outcome at a Single Institution. Ann Thorac Surg 2016;101:294-300. [Crossref] [PubMed]
- Yang H, Sun Y, Yao F, et al. Surgical Therapy for Bilateral Multiple Primary Lung Cancer. Ann Thorac Surg 2016;101:1145-52. [Crossref] [PubMed]
- Gu C, Pan X, Wang R, et al. Analysis of mutational and clinicopathologic characteristics of lung adenocarcinoma with clear cell component. Oncotarget 2016;7:24596-603. [Crossref] [PubMed]
- Fu H, Gu ZT, Fang WT, et al. Long-Term Survival After Surgical Treatment of Thymic Carcinoma: A Retrospective Analysis from the Chinese Alliance for Research of Thymoma Database. Ann Surg Oncol 2016;23:619-25. [Crossref] [PubMed]
- Yue J, Gu Z, Yu Z, et al. Pretreatment biopsy for histological diagnosis and induction therapy in thymic tumors. J Thorac Dis 2016;8:656-64. [Crossref] [PubMed]
- Wei Y, Gu Z, Shen Y, et al. Preoperative induction therapy for locally advanced thymic tumors: a retrospective analysis using the ChART database. J Thorac Dis 2016;8:665-72. [Crossref] [PubMed]
- Wang H, Gu Z, Ding J, et al. Perioperative outcomes and long-term survival in clinically early-stage thymic malignancies: video-assisted thoracoscopic thymectomy versus open approaches. J Thorac Dis 2016;8:673-9. [Crossref] [PubMed]
- Liu Q, Gu Z, Yang F, et al. The role of postoperative radiotherapy for stage I/II/III thymic tumor-results of the ChART retrospective database. J Thorac Dis 2016;8:687-95. [Crossref] [PubMed]
- Ma K, Gu Z, Han Y, et al. The application of postoperative chemotherapy in thymic tumors and its prognostic effect. J Thorac Dis 2016;8:696-704. [Crossref] [PubMed]
- Liang G, Gu Z, Li Y, et al. Comparison of the Masaoka-Koga staging and the International Association for the Study of Lung Cancer/the International Thymic Malignancies Interest Group proposal for the TNM staging systems based on the Chinese Alliance for Research in Thymomas retrospective database. J Thorac Dis 2016;8:727-37. [Crossref] [PubMed]
- Wang F, Pang L, Fu J, et al. Postoperative survival for patients with thymoma complicating myasthenia gravis-preliminary retrospective results of the ChART database. J Thorac Dis 2016;8:711-7. [Crossref] [PubMed]
- Huang Q, Li J, Sun Y, et al. Efficacy of EGFR Tyrosine Kinase Inhibitors in the Adjuvant Treatment for Operable Non-small Cell Lung Cancer by a Meta-Analysis. Chest 2016;149:1384-92. [Crossref] [PubMed]
Education
This Department has eight PhD candidates and four master’s candidates of medicine college at Shanghai Jiao Tong University.
Training programme
As one of the largest and top thoracic and cardiovascular surgery training centers in China, our programs has enrolled a total of 69 thoracic surgeons from all regions of China this year, including 37 trainees in the 45th National Cardiothoracic Surgery Training Program.
Discussion
Starting with 2017 data, the Department of Thoracic Surgery in Shanghai Chest Hospital will publish an annual performance report every year. This will not only enable our peers to obtain the medical quality information and case volume of our team but will also serve as an internal reminder to constantly improve the efficiency and quality of the medical services we provided. Through the exchange and cooperation with domestic and foreign counterparts, we will continue to push Shanghai Chest to be one of the best clinical centers for comprehensive thoracic surgery in the world.
In the next year, we will strive to improve the quantity and quality of surgery. We wish to expand the indication of minimally invasive surgery through combining the mature minimally invasive techniques with more complex surgery. Continuously more innovative techniques will be incorporated into our program via ongoing education and collaboration within our institution, colleagues in China, and colleagues around the world. Our department will initiate and participate in more single center and multi-centered clinical trials and get actively involved in the development or modification of treatment guidelines for thoracic surgery.
Acknowledgments
Funding: None.
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/shc.2017.10.03). AS serves as an unpaid editorial board member of Shanghai Chest from Jul 2017 to Jun 2019. DKH serves as an unpaid editorial board member of Shanghai Chest from Jan 2018 to Dec 2019. DM serves as an unpaid editorial board member of Shanghai Chest from Dec 2017 to Nov 2019. WF serves as an unpaid Executive Editor-in- Chief of Shanghai Chest. The other authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
Cite this article as: Yao F, Wang R, Guo X, Gu Z, Fan L, Zhou W, Ye B, Zhong C, Zhao H, Li Z, Sihoe A, Hogarth DK, Molena D, Fang W. Annual report of Department of Thoracic Surgery at Shanghai Chest Hospital. Shanghai Chest 2018;2:18.