Minimally-invasive surgery for non-thymomatous myasthenia gravis
Introduction
Myasthenia gravis (MG) is an autoimmune disease of the neuromuscular junction for which clear pathophysiological basis and diagnostic modalities are well-known. MG results from the output of antibodies against the postsynaptic nicotinic acetylcholine receptors at the neuromuscular junctions (1,2). Thymoma is described in about 15% of patients with MG (3). The thymic gland, which is recognized as site of production of these autoantibodies, is located in the anterior mediastinum space, between both right and left phrenic nerves, however being sometimes also located above or below them. Furthermore, ectopic islands of thymic tissues may be observed at various sites in the anterior mediastinum (2,4).
MG clinical manifestations include extraocular muscle weakness, which is characterized by eyelid ptosis and diplopia (ocular MG). In approximately 50% of patients with ocular MG, generalized MG (GMG) may also develop: it involves other muscles and manifests as limb weakness and bulbar symptoms, within 2-year period (5).
A recent randomized trial has definitively demonstrated the importance of thymic resection in MG patients, showing improved clinical outcomes over 3-year period for those who received thymectomy, compared to those treated with medical therapy, only (6).
Once the thymectomy role is established, the next question regards the optimal surgical approach to the thymic gland. The first transcervical thymectomy was performed in 1912 by Sauerbruch, in Germany; in 1988 Jaretzki et al. (2) recommended the so-called “maximal transcervical-trans-sternal thymectomy” for non-thymomatous (NT) myasthenic patients. Since then, the trans-sternal approach (with several different modifications) was routinely employed (7). The debate between transcervical and trans-sternal thymectomy continued until the recent dramatic development of minimally-invasive techniques (MITs) [e.g., video-assisted thoracic surgery (VATS) and robotic assisted thoracic surgery (RATS)]. The first VATS thymectomy was successfully performed by Landreneau et al. in 1992 (8).
The ultimate goal of surgery is to achieve MG complete stable remission (CSR), defined as no myasthenic symptoms or signs without any ongoing treatment for at least 1 year (9). The neurological outcome is dependent on the extent of the mediastinal tissue resection, which is, at the same time, dependent on surgeon’s commitment in pursuing the resection, in terms of time and scrupulous search for possible ectopic thymic tissue in the mediastinal space. Thymectomy for NT MG may potentially be a morbid surgical intervention: it is, in fact, usually performed in young and fragile patients, in which MG clinical compensation is achieved generally after several medical attempts. The risk of developing postoperative complications (generally respiratory) is high. Therefore, the optimal surgical approach should take into account these risks and it should be chosen through a reduced operative and anesthesia time, avoiding long periods of artificial ventilation as well as painful surgical incisions. Lastly, patient’s general satisfaction and quality of life (QOL) after thymectomy, including less pain and a cosmetic surgical incision, should also be considered when a surgeon decides the approach.
The aim of this editorial is to describe MIT results, compared to the classical extended trans-sternal thymectomy.
Extended transcervical thymectomy
Ruffini et al. (10) recently report the ultimate results of thymectomy for NT MG patients operated through an extended transcervical approach, previously described by Maggi et al. (11). This technique requires a single-lumen endotracheal tube with the patient placed in a supine position with the neck hyperextended. A small (3–4 cm) cervical incision few centimetres above the sternal notch is performed, and the mid-cervical fascia is incised. The two thymic upper poles are exposed and ligated, and the thymic gland is carefully separated from the posterior cervical connective. The upper sternal portion is therefore exposed and a partial (8–10 cm) sternal split is performed. Through this incision the mediastinum is accessed. The thymectomy is then completed through the thymic vein ligation. The mediastinal pleura is gently separated from the mediastinal fatty tissue and the thymic dissection is conducted down to the pericardium and laterally to both the phrenic nerves. The thymus and its capsule are completely resected along with the mediastinal fat tissue. A careful inspection of the surgical specimen and the mediastinal space is then conducted, to rule out of any residual unresected thymic tissue. A small drainage is placed retrosternally. If the mediastinal pleura is inadvertently opened, a small-bore pleural drain is laterally placed. Figure 1 illustrates the intervention.
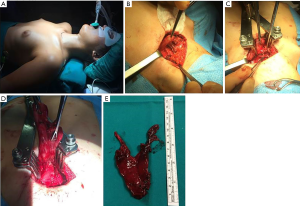
In uncomplicated procedure, the operative time is approximately 90 minutes, the mediastinal drainage is removed in postoperative day (POD) 1, and the patient is discharged in POD 2.
This intervention is classified as T-1c, according to the Myasthenia Gravis Foundation of America (MGFA) thymectomy classification (12), with removal of all visible thymic tissue encapsulated and extracapsular in the mediastinal fatty tissue.
The authors analyse 215 NT MG patients, operated between 1988 and 2012 in a single Institution; the median preoperative MG symptoms duration is 9 months. There were no intra/postoperative mortality; 14 cases of minor complications (pneumothorax, prolonged mediastinal drainage, wound seroma) are observed. Ten patients die, of whom 3 are of MG. MG symptoms improve in 85% of patients; CSR rate is 34%, pharmacological remission (PR) 4%. Cumulative incidence of CSR/PR is 27%, 37% and 46% at 5, 10 and 15 years, respectively.
Independent predictors of CSR/PR increased rate are: age (P=0.028) and MG symptoms duration <6 months (P=0.013).
Calhoun et al. (13) report their results on 100 MG patients who received a transcervical thymectomy between 1989 and 1998. The median hospital stay is 1 day; there are no deaths or severe complications after surgery. Of the 78 patients who underwent surgery >12 months ago and therefore are available for the statistical analyses, with a median follow-up of 5 years, the median preoperative Osserman grade (14) improves from 3.0 (mean 2.73) before, to 1.0 (mean 0.94) after surgery.
Shrager et al. (15) describes the outcome of 151 patients treated between 1992 and 2000 with this technique. The overall complication rate is 7.3% and nearly all procedures are outpatient. The mean postoperative Osserman class is 1.0. Kaplan-Meier estimates of CSR are 43% and 45% at 3 and 6 years, respectively. At multivariate analysis, only preoperative MG severity is inversely significantly associated with CSR.
The predictors of outcome in thymectomy for MG are also analysed by Budde et al. (16): in 113 consecutive thymectomies (between 1974 and 1999) CSR is observed in 21% of patients, while marked MG improvement in 54%. At the univariate analysis, sex, age and pathology (22 patients, in fact, presented with Thymoma) significantly correlate with outcome (P<0.05).
Extended thoracoscopic thymectomy
Tomulescu and Popescu (17) firstly proposed a thoracoscopic unilateral extended thymectomy (TUET), with the aim to proceed with the rigorous resection of all thymus and fat tissue in the anterior mediastinum from the diaphragm to the cervical area, between the two phrenic nerves, using a thoracoscopic approach. The advantages of this technique are: surgical trauma minimization along with undoubted cosmetic results. Furthermore, the use of high-definition cameras achieves an exceptional intraoperative view, making also the intervention safer, minimizing the risks of injury of fine structures, not related to the surgical procedure. Farther, VATS thymectomy allows better lung functions preservation, if compared to the classical median sternotomy (18).
For unilateral VATS thymectomy, the patient is placed in the supine position, tilted upward by 30°. The trachea is intubated with a double-lumen tube for split-lung ventilation. Three trocars are inserted usually into the left hemithorax (the first through the 5 or 6° intercostal space, between the middle and posterior axillary lines; the second and third through the third intercostal space on the anterior axillary line and through the fourth or fifth intercostal space on the midclavicular line, respectively). Pleural cavity exploration is facilitated by both the selective bronchial intubation and CO2 insufflation at a maximum of 10 mmHg pressure.
The operation starts with two incisions in the mediastinal pleura, along the phrenic nerve and the internal thoracic artery, with the aim to delimitate the surgical field as well as to allow CO2 to facilitate mediastinal dissection. By using energy devices, the dissection is facilitated, decreasing the time of the intervention, and avoiding the risks of electrocoagulation in this area. AII anterior mediastinal tissue including the pericardial fat at the pericardiophrenic angle is included in the “en bloc” resection. During the posterior dissection, the pericardium, the aortic arch, the left brachiocephalic vein, and the superior vena cava are visualized and all fat tissue in this area is resected. The most difficult area to dissect is between the superior vena cava and the left brachiocephalic vein. At the superior pole, the dissection is performed in the anterior carotidal plane to the internal thoracic artery level. The thymectomy ends with the identification of the superior part of the gland, the thyreothymic ligament section, and freeing of the superior horns from the surrounding tissue. Cervical skin transillumination identifies the cervical limit of the dissection. During the operation superior, lateral, or medial arterial thymic pedicles are visualized, and clipped or ultrasonically coagulated. The thymus is quite easily extracted by enlarging the hole of the second trocar port (the anterior one) and bagging the piece before the extraction. A small chest drainage is then placed in the pleural cavity through the inferior trocar port.
A thoracoscopic thymectomy through the right side is technically performed in the same manner. However, as reported by Rückert et al. (19), the aorto-pulmonary window and the left thymic inferior horn are the most difficult part of this surgical approach. The left approach seems to have some advantages: (I) a better phrenic nerve visualization and, therefore, a safer manoeuvres to dissect it, reducing the risk of possible damage; (II) an easier thymic right side dissection through a left-side approach rather than the contrary, especially for the aorto-pulmonary window and the left pericardiophrenic angle. Tomulescu and Popescu (17) believe that a left-side approach may facilitate the respective procedures, especially when a large amount of fat tissue, mostly located in the anterior left mediastinum, is present.
The CO2 insufflation is to be preferred, since anterior mediastinum is enlarged and this usually aids the dissection (20). The anaesthetist should be aware of the surgical technique because of possible problems with both intraoperative patient’s ventilation and CO2 insufflation. Moreover, the use of a 30° high-definition camera provides a significant help in the completeness of thymic resection evaluation, ensuring also that the dissection did not caused any damage to the phrenic nerves.
Bilateral VATS thymectomy, which usually starts from the right-side approach, has been also reported by some authors (21-23); generally the extent and the amount of mediastinal tissue resected through this approach is very similar to those in trans-sternal thymectomy, with less invasiveness for the MG patients.
One of the largest TUET series is reported by Tomulescu et al. (24). The authors analyze their 10-year experience on 240 patients treated with unilateral thoracoscopic approach: CSR is observed in 61% of patients and the cumulative probability to achieve is 0.88 at 10 years. There is no mortality and 5% morbidity, only, with one case of severe postoperative myasthenic crisis observed. The authors conclude that the ideal MG patient candidate for a thoracoscopic thymectomy should be less than 35-year-old, treated within 1 year after MG development, and expecting to have CSR within 18 months (24).
Finally, a recent meta-analysis about the results of VATS versus extended open thymectomy (OT) shows no significant difference in terms of operation time, intensive-care unit (ICU) postoperative stay and complications (especially pneumonia) and CSR rate, between the two approaches. On the other hand, patients who received VATS have a significantly less intraoperative blood loss, a shorter hospital time and less postoperative myasthenic crisis (25).
Robotic thymectomy
Robotic thymectomy is another fundamental step forward in the field of minimally-invasive surgery for the anterior mediastinum. Thymectomy appears to be adequate for a robotic procedure since the gland is located in a small space, with rigid walls and difficult access. Recent improvement of material as well as robotic technique makes extended thymectomy generally easier and safer compared to the traditional thoracoscopy, despite the lack of tactile sense, respecting also the surgeon’s ergonomy. Furthermore, proctoring and training with the robotic technique is more easy and rapid compared to the traditional VATS (13). This may explain why surgeons with limited thoracoscopic experience and with access to a robotic program prefer the latter and learn to perform an extended thymectomy more rapidly and effectively than through a VATS approach. Between 2001 and 2012 approximately 3,500 robotic thymectomies have been performed worldwide, and registered by Intuitive Surgical (Sunny Vale, CA, USA).
A left-side approach is preferred also for the robotic thymectomy, to avoid injuries to the mediastinal structures. The patient is placed in a supine position, with the table slightly tilted to the patient’s right side. The left arm is usually placed below the table level (Figure 2A). A 12 mm trocar for the binocular camera is placed in the 5
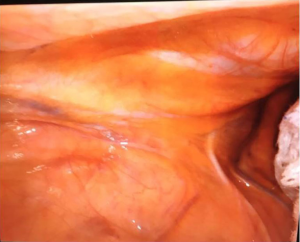
Thymic gland dissection starts in the middle of the pericardium, parallel to the phrenic nerve, which is usually well recognized (Figure 3). After the aorto-pulmonary window tissue dissection, cervical pleura identification and opening at the entrance of the innominate vein is performed. Tissue dissection, also with blunt gentle manoeuvre, is continued until the subxiphoid pleura is reached. Then the right lung, covered only by the parietal pleura is visualized. The thymic vein(s), originating from the innominate one, is/are dissected and clipped; special attention should be done in case of atypically located veins. The preparation of the right thymic lobe is mostly performed under CO2 insufflation. Care should be taken to identify the right phrenic nerve, even before opening the right mediastinal pleura. The thymic/mediastinal tissue bloc is bagged and then removed through a middle trocar incision, and a chest drain is placed.
Several authors report large series of robotic thymectomies; the main indications are MG but also thymomas. Ismail et al. (26) describes 317 thymectomies, of which 273 for MG: the CSR rate is 57%. The authors conclude that in selected cases (small children, older or obese patients) robotic approach has a special technical advantage.
Freeman et al. (27), describing 75 MG operated patients (no thymoma were included), reports a CSR rate of 28%, 25% pharmacologic remission and 47% of patients with minimal clinical manifestations. No patient experiences a worsening of myasthenic symptoms after thymectomy.
Della Marina and co-authors (28) recently report the outcome of robotic thymectomy in a very particular subset of patients: children and adolescent with juvenile acetylcholine receptor antibody-positive MG. In 13/16 operated patients, clinical improvement following thymectomy at 6 months follow-up (76%) is achieved for a minimum of one grade (according to MGFA classification) and at a 12-month follow-up (out of 16 patients) 7 patients are in PR (44%).
In a retrospective study of 100 MG patients (with and without thymoma), Marulli et al. (29) report a CSR rate of 28.5%. Finally, Table 1 shows the comparison of results of thymectomy according to the different surgical approaches.
Table 1
| Approach | Author | Patients | CSR (%) |
|---|---|---|---|
| Transsternal maximal thymectomy | Jaretzki | 95 | 37.9 |
| Transcervical | Ruffini | 215 | 34 |
| Calhoun | 100 | NA | |
| Shrager | 151 | 43 | |
| Budde | 113 | 21 | |
| VATS thymectomy | Tomulescu | 240 | 61 |
| Robotic thymectomy | Ismail | 273 | 57 |
| Freeman | 75 | 28 | |
| Marulli | 100* | 28.5 |
*, also thymoma patients are included in this series. NA, not available; CSR, complete stable remission.
Discussion
MG is one of the most common disorders of the neuromuscular transmission. A wide variation in clinical severity is observed, ranging from occasional diplopia and ptosis (with often spontaneous remission) to severe generalized weakness, which seldom requires temporary mechanical ventilation. A recent randomized clinical trial has demonstrated that thymectomy is effective in achieving MG symptoms improvement and definitive CSR (6). Significant debate in the scientific community however continues concerning the ideal surgical approach for thymectomy.
Thymic gland anatomy is characterized by a typical H-shape with two cervical and two mediastinal poles, the latter broadly extending along the pericardium and in the anterior cardio-phrenic recess. Furthermore, an extreme anatomical thymic variability has also been described, making very profound implication on surgery whenever the optimal surgical approach is discussed (30). Additional ectopic thymic islands may be found, in fact, in 32–98% of patients in which an extended transsternal thymectomy is performed. They are generally located in the paratracheal and anterior mediastinal fat tissue, between thyroid and diaphragm, as well as bilaterally, from beyond each phrenic nerve (30). Most thoracic surgeons are therefore convinced that an extended thymectomy is the prerequisite to achieve postoperative MG improvement or CSR.
The MGFA classifies the different types of surgical thymectomy for MG onto four categories and several sub-categories, according to the presumed extent of the thymic resection performed (9). The operations may vary in the extent to which extracapsular mediastinal and cervical fat tissues are removed.
MG outcome has been reported by several series, in the form of complete and/or partial remission rate, using, generally, the crude remission rate. However, MGFA recommendations for clinical research standards (9) suggest that response to thymectomy should be judged by the drug-free CSR rate, evaluated by the Kaplan-Meier analysis.
In 1996, Masaoka et al. (31) described their 20-year experience with 278 MG patients who received an extended trans-sternal thymectomy. Reported remission rates were 36% at 3 years and 45.8% at 5 years, and 20 years 50%. Morbidity of this surgical approach was not inconsistent (14 patients died postoperatively, 6 for MG complications). Since then, the aim of surgery is to achieve and adequate thymectomy (including also mediastinal fat tissue) while minimizing adverse postoperative outcomes, as well as facilitating patient’s recovery for the operation. Surgery, in fact, poses MG patients at high risk because of surgical stress, which may worsen clinical symptoms, also precipitating possible postoperative respiratory failure as well as myasthenic crisis. An optimal surgical approach therefore should combine the least invasiveness with the maximal radicality.
The recent advent of minimally-invasive operations (VATS and robotic thymectomy in particular) extended the indication for thymectomy in MG patients, achieving comparable results with less traumatic approaches (19,32,33). Recent meta-analysis study (25) demonstrate that VATS is superior to extended thymectomy in terms of intraoperative blood loss, hospital stay, low postoperative complications rates and risk of myasthenic crisis development. Furthermore, MIT reduced trauma, due to the minimal incisions, causes also less postoperative pain and, therefore, more benefit for the patient and less postoperative complications (34). In addition, demonstration that the pulmonary function is significantly better preserved in the immediate postoperative period after VATS than after median sternotomy is reported in another study (35).
MG CSR rate is regarded as an important criterion whether the thymus and the ectopic mediastinal fat tissue have been effectively resected. No significant differences in CSR rates are observed between VATS and extended transsternal thymectomy: therefore, MITs thymectomy could offer comparable results (36,37). Similar results have been observed also for transcervical and robotic thymectomy.
In conclusion, NT MG patients can be treated with a minimally-invasive approach with CSR rates broadly comparable to more invasive ones. The choice of surgical approach should be done by considering first MG severity and its medical grade of clinical compensation, since MG patients are usually fragile with high risk of developing serious respiratory complications. Finally, we believe that the type of surgery should depend on surgeon’s preference and experience.
Acknowledgments
Funding: None.
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/shc.2017.12.07). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Drachman DB, McIntosh KR, Reim J, et al. Strategies for treatment of myasthenia gravis. Ann N Y Acad Sci 1993;681:515-28. [Crossref] [PubMed]
- Jaretzki A 3rd, Penn AS, Younger DS, et al. "Maximal" thymectomy for myasthenia gravis. Results. J Thorac Cardiovasc Surg 1988;95:747-57. [PubMed]
- Papatestas AE, Genkins G, Kornfeld P, et al. Effects of thymectomy in myasthenia gravis. Ann Surg 1987;206:79-88. [Crossref] [PubMed]
- Ashour M. Prevalence of ectopic thymic tissue in myasthenia gravis and its clinical significance. J Thorac Cardiovasc Surg 1995;109:632-5. [Crossref] [PubMed]
- Bever CT Jr, Aquino AV, Penn AS, et al. Prognosis of ocular Myasthenia. Ann Neurol 1983;14:516-9. [Crossref] [PubMed]
- Wolfe GI, Kaminski HJ, Aban IB, et al. Randomized Trial of Thymectomy in Myasthenia Gravis. N Engl J Med 2016;375:511-22. [Crossref] [PubMed]
- Prokakis C, Koletsis E, Salakou S, et al. Modified maximal thymectomy for myasthenia gravis: effect of maximal resection on late neurologic outcome and predictors of disease remission. Ann Thorac Surg 2009;88:1638-45. [Crossref] [PubMed]
- Landreneau RJ, Dowling RD, Castillo WM, et al. Thoracoscopic resection of an anterior mediastinal tumor. Ann Thorac Surg 1992;54:142-4. [Crossref] [PubMed]
- Jaretzki A 3rd, Barohn RJ, Ernstoff RM, et al. Myasthenia gravis: recommendations for clinical research standards. Task Force of the Medical Scientific Advisory Board of the Myasthenia Gravis Foundation of America. Ann Thorac Surg 2000;70:327-34. [Crossref] [PubMed]
- Ruffini E, Guerrera F, Filosso PL, et al. Extended transcervical thymectomy with partial upper sternotomy: results in non-thymomatous patients with myasthenia gravis. Eur J Cardiothorac Surg 2015;48:448-54. [Crossref] [PubMed]
- Maggi G, Casadio C, Cavallo A, et al. Thymectomy in myasthenia gravis. Results of 662 cases operated upon in 15 years. Eur J Cardiothorac Surg 1989;3:504-9; discussion 510-1. [Crossref] [PubMed]
- Sonett JR, Jaretzki A 3rd. Thymectomy for nonthymomatous myasthenia gravis: a critical analysis. Ann N Y Acad Sci 2008;1132:315-28. [Crossref] [PubMed]
- Calhoun RF, Ritter JH, Guthrie TJ, et al. Results of transcervical thymectomy for myasthenia gravis in 100 consecutive patients. Ann Surg 1999;230:555-9; discussion 559-61. [Crossref] [PubMed]
- Drachman DB. Myasthenia gravis. N Engl J Med 1994;330:1797-810. [Crossref] [PubMed]
- Shrager JB, Nathan D, Brinster CJ, et al. Outcomes after 151 extended transcervical thymectomies for myasthenia gravis. Ann Thorac Surg 2006;82:1863-9. [Crossref] [PubMed]
- Budde JM, Morris CD, Gal AA, et al. Predictors of outcome in thymectomy for myasthenia gravis. Ann Thorac Surg 2001;72:197-202. [Crossref] [PubMed]
- Tomulescu V, Popescu I. Unilateral extended thoracoscopic thymectomy for nontumoral myasthenia gravis--a new standard. Semin Thorac Cardiovasc Surg 2012;24:115-22. [Crossref] [PubMed]
- Rückert JC, Walter M, Müller JM. Pulmonary function after thoracoscopic thymectomy versus median sternotomy for myasthenia gravis. Ann Thorac Surg 2000;70:1656-61. [Crossref] [PubMed]
- Rückert JC, Czyzewski D, Pest S, et al. Radicality of thoracoscopic thymectomy--an anatomical study. Eur J Cardiothorac Surg 2000;18:735-6. [Crossref] [PubMed]
- Mineo TC, Pompeo E, Ambrogi V, et al. Adjuvant pneumomediastinum in thoracoscopic thymectomy for myasthenia gravis. Ann Thorac Surg 1996;62:1210-2. [Crossref] [PubMed]
- Scelsi R, Ferrò MT, Scelsi L, et al. Detection and morphology of thymic remnants after video-assisted thoracoscopic extended thymectomy (VATET) in patients with myasthenia gravis. Int Surg 1996;81:14-7. [PubMed]
- Huang CS, Cheng CY, Hsu HS, et al. Video-assisted thoracoscopic surgery versus sternotomy in treating myasthenia gravis: comparison by a case-matched study. Surg Today 2011;41:338-45. [Crossref] [PubMed]
- Lee CY, Kim DJ, Lee JG, et al. Bilateral video-assisted thoracoscopic thymectomy has a surgical extent similar to that of trans-sternal extended thymectomy with more favourable early surgical outcomes for myasthenia gravis patients. Surg Endosc 2011;25:849-54. [Crossref] [PubMed]
- Tomulescu V, Sgarbura O, Stanescu C, et al. Ten-year results of thoracoscopic unilateral extended thymectomy performed in nonthymomatous myasthenia gravis. Ann Surg 2011;254:761-5; discussion 765-6. [Crossref] [PubMed]
- Qi K, Wang B, Wang B, et al. Video-assisted thoracoscopic surgery thymectomy versus open thymectomy in patients with myasthenia gravis: a meta-analysis. Acta Chir Belg 2016;116:282-8. [Crossref] [PubMed]
- Ismail M, Swierzy M, Rückert JC. State of the art of robotic thymectomy. World J Surg 2013;37:2740-6. [Crossref] [PubMed]
- Freeman RK, Ascioti AJ, Van Woerkom JM, et al. Long-term follow-up after robotic thymectomy for nonthymomatous myasthenia gravis. Ann Thorac Surg 2011;92:1018-22; discussion 1022-3. [Crossref] [PubMed]
- Della Marina A, Kölbel H, Müllers M, et al. Outcome after Robotic-Assisted Thymectomy in Children and Adolescents with Acetylcholine Receptor Antibody-Positive Juvenile Myasthenia Gravis. Neuropediatrics 2017;48:315-22. [Crossref] [PubMed]
- Marulli G, Schiavon M, Perissinotto E, et al. Surgical and neurologic outcomes after robotic thymectomy in 100 consecutive patients with myasthenia gravis. J Thorac Cardiovasc Surg 2013;145:730-5; discussion 735-6. [Crossref] [PubMed]
- Shields T. The thymus. In: Shields T. editor. Mediastinal surgery. Philadelphia: Lea & Febiger, 1991:6-13.
- Masaoka A, Yamakawa Y, Niwa H, et al. Extended thymectomy for myasthenia gravis patients: a 20-year review. Ann Thorac Surg 1996;62:853-9. [Crossref] [PubMed]
- Toker A, Eroglu O, Ziyade S, et al. Comparison of early postoperative results of thymectomy: partial sternotomy vs. videothoracoscopy. Thorac Cardiovasc Surg 2005;53:110-3. [Crossref] [PubMed]
- Yim AP. Paradigm shift in surgical approaches to thymectomy. ANZ J Surg 2002;72:40-5. [Crossref] [PubMed]
- Kaseda S, Aoki T, Hangai N, et al. Better pulmonary function and prognosis with video-assisted thoracic surgery than with thoracotomy. Ann Thorac Surg 2000;70:1644-6. [Crossref] [PubMed]
- Mack MJ, Landreneau RJ, Yim AP, et al. Results of video-assisted thymectomy in patients with myasthenia gravis. J Thorac Cardiovasc Surg 1996;112:1352-9; discussion 1359-60. [Crossref] [PubMed]
- Meyer DM, Herbert MA, Sobhani NC, et al. Comparative clinical outcomes of thymectomy for myasthenia gravis performed by extended transsternal and minimally invasive approaches. Ann Thorac Surg 2009;87:385-90; discussion 390-1. [Crossref] [PubMed]
- Lin MW, Chang YL, Huang PM, et al. Thymectomy for non-thymomatous myasthenia gravis: a comparison of surgical methods and analysis of prognostic factors. Eur J Cardiothorac Surg 2010;37:7-12. [Crossref] [PubMed]
Cite this article as: Filosso PL, Ruffini E, Lausi PO, Lyberis P, Costardi L, Olivetti S, Oliaro A, Guerrera F. Minimally-invasive surgery for non-thymomatous myasthenia gravis. Shanghai Chest 2018;2:23.