Treatment of esophageal diverticula in uniportal video-assisted thoracoscopic surgery
Introduction
Esophageal diverticulum is a rare disease (incidence 1/100,000) caused by impairment of esophageal motility. Esophageal diverticula are classified according to the localization in: upper esophageal (Zenker: 70%), thoracic and mediastinal (10%) and epiphrenic diverticula (20%). Traditionally, surgical treatment involves a thoracotomy approach that allows diverticulectomy and esophageal myotomy. For many years, esophageal surgery has been recognized as a very challenging issue for surgeons and risky for patients. Indeed, the esophagus is really located deep in the neck and the posterior mediastinum and the absence of a formal serous layer leads to unsafe anastomosis with a great risk of leakage.
The first description of thoracoscopic diverticulectomy dates back to 2001 (1). The minimally invasive surgery has been proven to guarantee many advantages such a reduction in pulmonary complications, wound infections, postoperative pain and length of postoperative stay compared to open surgery (2,3). A superior cosmetic result is an additional benefit, especially when dealing with benign diseases in younger patients. Nowadays there are not yet much data in the literature concerning the uniportal video-assisted thoracoscopic surgery (VATS) approach for esophageal diverticula (4).
In the present work, we report our preliminary experience in uniportal VATS esophageal diverticulectomy.
Case presentation
Between December 2016 and January 2018, 3 patients (2 men, 1 woman) underwent diverticulum resection of the middle and distal esophagus (2 epiphrenic and 1 medium thoracic) and esophageal myotomy in uniportal VATS at our Center.
The average age of patients was 63.5±1.5 years. The clinical data of the three patients are reported in Table 1.
Table 1
| Characteristics | N=3 |
|---|---|
| Age (years) | 63.5±1.5 |
| Gender (Male) | 2 (67%) |
| Smoking | 2 (67%) |
| COPD | 1 (33%) |
| Heart disease | 2 (67%) |
| Arterial hypertension | 2 (67%) |
| Diabetes | 0 |
| ASA score | 2.3±0.57 |
| Other diseases | 2 (67%) |
| Hiatal hernia | 1 (33%) |
| Fundoplication | 1 (33%) |
| Preoperative dysphagia | 3 (100%) |
| Weight loss | 3 (100%) |
COPD, chronic obstructive pulmonary disease. The data were expressed as mean ± SD or n (%).
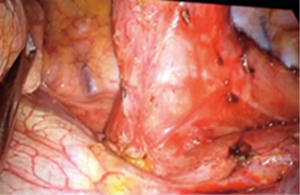
A Carlens dual lumen endotracheal tube was used under general anesthesia. The patient was positioned in a lateral left-side position, with the table slightly flexed. The surgeons stood in front of the patient’s ventral side. A single 4 cm “muscle sparing” incision was performed at the level of the fifth right intercostal space on the mid-posterior axillary line. A skin retractor was introduced and all instruments passed through the same incision, with the 30° 10 mm-camera positioned above everything (Figure 1). The procedure started with dissection and mobilization of the esophagus (using an energy device) and the identification of the diverticulum (Figure 2).
In case of epiphrenic diverticula the dissection of the diaphragmatic crus could be necessary. Careful attention was paid to identify and preserve the vagus nerve. After that we proceeded with the preparation of the diverticular collar and its section along the major axis of esophagus, using an endoscopic linear stapler (sequential 2.5/45-mm vascular cartridges; Figure 3). The resected diverticulum was removed by a retrieval bag. A hydropneumatic test was performed for checking and excluding any staple-line leak. The application of some Fibrin glue is useful to reinforce the staple line. The procedure was completed with a standard esophageal myotomy (4–5 cm along the esophagus, above and below the resected diverticulum). Hiatoplasty was performed if there was a story of reflux disease and hiatus hernia. A 28 Fr drainage was placed through the same skin incision, with the distal tip into the posterior mediastinum, near the esophageal suture and a nasogastric tube was left in place. At the end of the procedure a regional loco-anesthetic block of the intercostal spaces was also performed to further reduce postoperative pain. In the post-operative period, the patient received a total parenteral nutrition up to the execution of the esophagogram on the 5th postoperative day (Figures 4,5). Subsequently, the pleural drainage and the nasogastric tube were removed.
The mean duration of the operation was 180±37 min. There were no conversions. The average hospital stay was 7.0±1.0 days (Table 2).
Table 2
| Variables | N=3 |
|---|---|
| Operative time (min) | 180±37 |
| Conversion | 0 |
| No. pleural drainages | 1 |
| Chest drain removal (days) | 6.5±0.5 |
| Post-operative stay (days) | 7.0±1.0 |
| Esophagogram (days) | 5.6±0.4 |
| Beginning of postoperative oral intake (days) | 5.6±0.4 |
| Localization of the diverticulum | |
| Middle thoracic esophagus | 1 (33%) |
| Lower thoracic esophagus | 2 (67%) |
| Extension (cm) | 3.88±1.26 |
The data were expressed as mean ± SD or n (%).
We did not have severe complications or dehiscences in the postoperative period. One patient developed atrial fibrillation (with a preoperative known story of pericarditis and recurrent atrial fibrillation) that was pharmacologically cardioverted.
The antalgic therapy was based on intraoperative intercostal block and subsequent administration of only paracetamol and NSAIDs, without opioid use. The mean pain on I postoperative day was 2.3±1.1 measured on VAS scale, with complete resolution after pleural tube removal. We have not registered neuralgia, paresthesias or wound infections. The aesthetic result was also judged satisfactory (Table 3).
Table 3
| Variables | N=3 |
|---|---|
| Pain in first postoperative day (VAS scale) | 2.3±1.1 |
| Mean duration of pain (days) | 3±1 |
| Pain after chest tube removal (VAS scale) | 0 |
| Cosmetic result (1 to 3 points) | 2.66±0.57 |
| Postoperative paresthesia and neuralgia | 0 |
| Wound infections | 0 |
The data were expressed as mean ± SD or n (%).
All patients were discharged in good condition with oral nutrition without any major complications. At the 6-month esophagogram control, we did not appreciate relapses and only one patient complained dysphagia, related to the previous too tight Nissen Fundoplication. An endoscopic dilatation resolved the problem.
Discussion
Abnormal esophageal motility is probably the main reason at the basis of diverticulum development (5). Dysphagia and posture-related regurgitation are usually the main symptoms. The dimension of diverticulum may worsen the symptomatology, although it is known that the symptoms correlate better with the esophageal motility characteristics than with the dimensions of the diverticulum (6).
Symptomatic patients should undergo surgical treatment, but surgery is not without risk. The Mayo Clinic series (7) reported a complication rate of 33% and a death rate of 9.1%. The Mayo Clinic study also found that patients with minimal symptoms were unlikely to progress clinically, so the surgical treatment should be reserved for patients with incapacitating symptoms.
Myotomy is routinely performed in patients with epiphrenic diverticula. Usually the myotomy is performed at the level of the diverticular collar and is extended both towards the cranial and at the distal level (over the lower esophageal sphincter), to treat the entire esophageal portion involved in the motility disorder. The only diverticulectomy without treatment of the underlying motor disorder is not advisable. It has been associated with a higher incidence of diverticulum recurrence and a suture line leak rate of 10% to 20% (7).
Laparoscopy is a possible approach to perform combining diverticulectomy, myotomy and fundoplication, as reported in recent studies (2). However, it may be difficult with this approach to reach the top of the diverticulum neck if the diverticulum is more than a few centimeters from the gastroesophageal junction and it may also be difficult to perform a proper extension myotomy. Furthermore, laparoscopic dissection in the mediastinum can be complicated by the rupture of the mediastinal pleura leading to pneumothorax, also hypertensive. The thoracoscopic approach, vice versa, may be appropriate for diverticulectomy and myotomy (in particular for patients with diverticula located more than few centimeters from the gastroesophageal junction or those requiring a long myotomy) but the laparoscopic approach seems preferable for fundoplication, although it was even described by uniportal VATS approach in literature (8). In recent years, the standard multiport VATS has evolved into a uniportal approach (9), used for lung resection and other increasingly complex cases (10-12), that is showing potential postoperative benefits in terms of reduction of pain and faster patient’s recovery.
Nowadays, however, there are not enough data in the literature, in particular on the uniportal thoracoscopic approach for esophageal diseases (13), to make a real and effective comparison between the different minimally invasive techniques. Nevertheless, it can be said that the minimally invasive approach has a positive impact from the point of view of pain control, ensuring early mobilization and reducing hospitalization time.
In our preliminary experience, the thoracoscopic uniportal approach seems to be feasible and safe, allowing the resection of diverticulum and the treatment of underlying motor disorder. Longer follow-up and more extensive studies are needed to clarify the role of uniportal VATS, compared to other mini-invasive techniques, such as robotic, laparoscopic or endoscopic techniques, in the treatment of esophageal diverticular disease.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the editorial office, Shanghai Chest for the series “The Second Roman Tips and Tricks in Thoracic Surgery - the Great Potential of Uniportal VATS”. The article has undergone external peer review.
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/shc.2019.01.03). The series “The Second Roman Tips and Tricks in Thoracic Surgery - the Great Potential of Uniportal VATS” was commissioned by the editorial office without any funding or sponsorship. Elisa Meacci served as the unpaid Guest Editor of the series and serves as an unpaid editorial board member of Shanghai Chest from Mar 2018 to Feb 2020. Stefano Margaritora served as the unpaid Guest Editor of the series. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patients for publication of this manuscript and any accompanying images.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- van der Peet DL, Klinkenberg-Knol EC, Berends FJ, et al. Epiphrenic diverticula: minimal invasive approach and repair in five patients. Dis Esophagus 2001;14:60-2. [Crossref] [PubMed]
- Andrási L, Paszt A, Simonka Z, et al. Laparoscopic Surgery for Epiphrenic Esophageal Diverticulum. JSLS 2018;22(2).
- Bencini L, Moraldi L, Bartolini I, et al. Esophageal surgery in minimally invasive era. World J Gastrointest Surg 2016;8:52-64. [Crossref] [PubMed]
- Fiorelli A, Izzo AC, Arrigo E, et al. Resection of esophageal diverticulum through uniportal video-assisted thoracoscopic surgery. Ann Transl Med 2018;6:179. [Crossref] [PubMed]
- Nehra D, Lord RV, DeMeester TR, et al. Physiologic basis for the treatment of epiphrenic diverticulum. Ann Surg 2002;235:346-54. [Crossref] [PubMed]
- Evander A, Little AG, Ferguson MK, et al. Diverticula of the mid- and lower esophagus: pathogenesis and surgical management. World J Surg 1986;10:820-8. [Crossref] [PubMed]
- Benacci JC, Deschamps C, Trastek VF, et al. Epiphrenic diverticulum: results of surgical treatment. Ann Thorac Surg 1993;55:1109-13; discussion 1114. [Crossref] [PubMed]
- Caronia FP, Fiorelli A, Santini M, et al. Uniportal Video-Assisted Thoracoscopic Surgery Resection of a Giant Midesophageal Diverticulum. Ann Thorac Surg 2017;103:e365-e367. [Crossref] [PubMed]
- Bertolaccini L, Rocco G, Viti A, et al. Geometrical characteristics of uniportal VATS. J Thorac Dis 2013;5:S214-6. [PubMed]
- Gonzalez-Rivas D, Fieira E, Delgado M, et al. Uniportal video-assisted thoracoscopic lobectomy. J Thorac Dis 2013;5:S234-45. [PubMed]
- Gonzalez-Rivas D, Yang Y, Sekhniaidze D, et al. Uniportal video-assisted thoracoscopic bronchoplastic and carinal sleeve procedures. J Thorac Dis 2016;8:S210-22. [PubMed]
- Lirio F, Galvez C, Bolufer S, et al. Tubeless major pulmonary resections. J Thorac Dis 2018;10:S2664-S2670. [Crossref] [PubMed]
- Nachira D, Meacci E, Mastromarino MG, et al. Initial experience with uniportal video-assisted thoracic surgery esophagectomy. J Thorac Dis 2018;10:S3686-S3695. [Crossref] [PubMed]
Cite this article as: Zanfrini E, Nachira D, Chiappetta M, Meacci E, Congedo MT, Ferretti GM, Pogliani L, Iaffaldano A, Vita ML, Porziella V, Margaritora S. Treatment of esophageal diverticula in uniportal video-assisted thoracoscopic surgery. Shanghai Chest 2019;3:6.