
Advancing cardiovascular care through nursing research, quality improvement, and evidence-based practice
Introduction/background
The global burden of cardiovascular disease is growing problem accounting for 17.3 million deaths in 2013 and projected to increase to 23.6 million by 2030 (1). Similar to other countries around the globe, in the United States, cardiovascular disease is endemic, remaining the greatest cause of hospitalization and mortality; attributing to more than 45% of deaths among American adults (1,2). The American Heart Association [2017] reports more than 92.1 million American adults living with some form of cardiovascular disease such as hypertension, peripheral vascular disease, or heart failure (1,2). These alarming statistics cannot not be ignored, confounding the need for research, implementation of practice guidelines and innovations that can improve health outcomes.
As the second largest economy in the world after the United States, China is the most populous nation and has the largest elderly population in the world (3). The healthcare priorities in China are now shifting from infectious diseases to non-communicable diseases (4) along with China’s tremendous economic development and people’s lifestyle change since the past four decades. Cardiovascular disease has been and will remain the leading cause of death for adults among both urban and rural Chinese population, accounting for approximately 43% and 45% of deaths in urban and rural areas (5), with hypertension as one of the most common risk factors (6).
Clinical practice guidelines
There are several approaches that can be used to target cardiovascular problems. The American Heart Association and American Colleges of Cardiology (AHA/ACC) promotes this through patient-centered research and the development of clinical practice guidelines for health care providers (7). Practice guidelines provide recommendations applicable to patients with, or at risk of developing cardiovascular disease. The focus of these guidelines is on medical practice in the United States, but guidelines developed in collaboration with other organizations can have a global impact. Although guidelines may be used to inform regulatory or payer decisions, they are intended to improve patients’ quality of care and align with patients’ interests. Guidelines are intended to define practices meeting the needs of patients in most, but not all, circumstances and should not replace clinical judgment (7).
In China, the first evidence-based clinical practice guidelines in the field of cardiovascular disease nursing was published in 2016 focusing on nursing care for acute heart failure adult patients (8). The guidelines together developed by National Center for Cardiovascular diseases, Committee of Heart Failure of Chinese Medical Doctor Association, and Beijing Nursing Association, systematically synthesized and clearly stated recommendations (including quality of evidence and strength of recommendations) with regard to factors including rapid assessment and triage, treatment, monitoring, follow-up (9).
Evidence-based practice (EBP)
The Johns Hopkins Hospital (JHH) is located in the east side of Baltimore city in Maryland, USA. A level-one urban academic medical center, the JHH receives more than 3 million patients and more than 360,000 emergency room visits per year. In the emergency department, more than 20% of patients seen for treatment are presenting with one or more cardiovascular related complaint. The JHH serves the east Baltimore community and beyond, providing treatment for a wide range of local, national and international patients. Health care teams at JHH work interdependently with the faculty of Johns Hopkins University, specifically with the schools of nursing, medicine, and public health, to support research development (10).
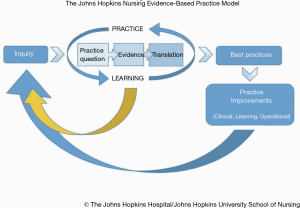
The Johns Hopkins Nursing Evidence-Based Practice (JHNEBP) model incorporates three critical components of professional nursing: practice, education and research (11). Since 2007, the JHNEBP model and tools have been guiding nursing professionals in their reporting of the scientific evidence (Figure 1). This model has served as an essential foundation of professional standards to guide nurses’ integration of the best available evidence, including research findings, into guiding practice decisions (11).
Compared with the JHNEBP model, the Joanna Briggs Institute (JBI)’s approach to evidence-based healthcare, or the JBI model (12,13), is more often utilized in nursing practice in China (Figure 2). Since the first center for evidence-based nursing was established at Fudan University School of Nursing in Shanghai in 2004, seven nursing schools and hospitals have established collaboration centers with the JBI to advance EBP in nursing and healthcare through evidence generation, evidence synthesis, evidence transfer, evidence implementation, and global health (15).

Quality improvement
Nurses and other health care professionals can lead quality improvement projects with a focus on improving processes, policies, and protocols on a unit or organizational level (11). Quality improvement teams work in tandem with leadership teams to develop a systematic approach in improving patient outcomes. Models such as the “Plan, Do, Study, Act” (PDSA) are often used to implement rapid cycle change in the hospital setting (11). The quality improvement process can also be guided by translational frameworks that guide the translation of research to clinical practice. At Johns Hopkins, nurse-led quality improvement projects are often targeted toward improving cardiovascular outcomes by reducing unplanned readmission, door-to-balloon times, and improving discharge patient education.
Chinese nurses have long been asked to enhance the nursing role to improve health outcomes of cardiovascular disease (16). However, great efforts are still needed to motivate nurses to play the critical role in educating patients and their lifestyle change, even though the majority of the nurses are considered to be knowledgeable about cardiovascular disease risk factors (17). At the same time, international successful experience as well as local unique factors should be taken into consideration to promote nurse-led multidisciplinary programs aiming at health improvement and quality improvement.
Research
Nurses have the opportunity to identify gaps in healthcare, explore this unknown territory, and generate new knowledge. Examples of Johns Hopkins nurses working diligently to advance cardiovascular healthcare include studying the impact of technology on health promotion, studying the impact of self-care and depression on heart failure readmissions, and studying health literacy in heart transplantation.
Johns Hopkins Professor of Nursing, Jerilyn Allen, along with a colleague and BSN nursing student, studied the impact of smartphone technology on weight loss in young adults. In a randomized control trial, researchers implemented a smartphone application for weight loss with text messaging from a coach. The data were compared to a control. The results showed statistically significant weight loss, reduction in body mass index (BMI) and reduction in waist circumference compared to the control group (18). Nurses in this scenario recognized the cultural trend of use of cell phone application and text messaging and optimized this practice to promote health outcomes.
Heart failure readmission is an important issue in the United States, with heart failure admissions costing the American health care system $39 billion annually and heart failure being the highest frequency 30-day readmission (19). Identifying readmission causes and finding solutions is imperative to promoting the health of our population, as well as sustaining our healthcare financial infrastructure. Johns Hopkins research nurses explored the possible link between self-care and depression and heart failure readmission. They found that those with major depressive symptoms were five times more likely to delay hospitalization than those without. This stemmed from feelings of uncertainty or indecision about whether their symptoms were urgent. Those hospitalized were also found to be less likely to consult healthcare providers prior to hospitalization, thus possibly avoiding a hospitalization (20).
Johns Hopkins nursing professors, along with colleagues from the Institute of Nursing Science Switzerland, the Academic Center for Nursing and Midwifery in Belgium, and the University of Missouri, USA, collaborated to study the health literacy in heart transplantation. The understanding of health literacy is imperative in supporting transplant recipients during their journey, providing educational materials and programs, and maintaining treatment adherence and compliance. In an international multicenter, cross-sectional study which surveyed heart transplant recipients across 11 countries and 4 continents, the BRIGHT study determined that 33.1% of heart transplant recipients had inadequate health literacy. Adequate health literacy was associated with compliance with physical therapy, but not with other health behaviors (21). Understanding health literacy of heart transplant candidates is critical to ensure patient adherence to treatment and understanding of their disease process.
Like the United States, great attention has been paid to nursing research on cardiovascular disease in China. According to a hot spot analysis of 5 years [2012–2016] in China’s nursing research (both English and Chinese language articles), “nursing on cardiovascular diseases” was identified as the leading cluster among all nursing research hot spot topics (22). When combining evidence-based nursing and cardiovascular disease research, nurses can be equipped with most updated best nursing practice, and patients can be provided with best available nursing recommendations.
Multidisciplinary, interdisciplinary and transdisciplinary teams
Cross-discipline team-based care is the gold standard model that underpins each approach highlighted in this article (23,24). The complexity of patient conditions and evolving health care systems means that silo working is increasingly risky for patient safety (23). Conversely, different team-based models employed across the spectrum of management issues of cardiovascular disease have been found effective, leading to decreased hospitalizations and hospital mortality, and reduced length of stay (24,25). Broadly speaking, there are three main models for cross-discipline team-based care and research that can be employed: multidisciplinary teams, interdisciplinary teams, and transdisciplinary teams. These terms are sometimes used interchangeably but do have specific definitions. Multidisciplinary teams are comprised of mixed-discipline practitioners who share their expertise but may not interact regularly and may still work in isolation (26). Interdisciplinary teams are again, formed of mixed-discipline practitioners, but in this model, they work more collaboratively, drawing together their expertise to develop a cohesive plan of patient-centered care (26). Transdisciplinary teams go a step further, often drawing in non-healthcare partners and encouraging practitioners to move beyond the remit of their training and discipline with the purpose of integrating expertise to solve problems and generating new knowledge (27). The nurse’s role in these teams may vary depending on the scope of practice which can vary from country to country. However, in general as well as specific to cardiovascular care, nurses are increasingly encouraged to take leading roles in EBP, advocacy and collaboration between disciplines (26).
While all three models can support effective healthcare delivery as well as research, EBP and quality improvement efforts to improve cardiovascular care, it is the transdisciplinary approach that is of particular relevance to this article. As one transdisciplinary model demonstrates, such teams are well suited to serve as clinical research teams who can perform research, EBP and quality improvement from conception through to implementation and translation (27). An example of this approach that has focused on cardiovascular disease comes from a transdisciplinary team based at Johns Hopkins University (28). This group established a transdisciplinary research center with the aims of reducing cardiovascular morbidity and mortality, and improving quality of life and healthcare experiences for African Americans and others affected by disparities in the local area. The transdisciplinary team includes but is not limited to partners from medicine, public health and nursing, with additional collaborations with colleagues from a range of disciplines such as pharmacy, nutrition, economics and psychology, insurance and the community. Among its many efforts to achieve these aims, the center houses a shared resources core, provides training and career development, and supports both research and quality improvement projects (28). While this is a particularly large undertaking across multiple settings with significant resources and funding, smaller transdisciplinary teams can also operate successfully within a single setting, which may be particularly useful when integrating evidence-based quality improvement projects (29).
Conclusions
Cardiovascular disease continues to be the number one cause of death in the United States, confounding the need for research to improve health outcomes. In China, cardiovascular disease is also shifting as a health care priority. The alarming statistics on both sides of the globe underscore the need for transdisciplinary teams that engage in EBP, quality improvement and research. As this paper discusses, there are numerous models and frameworks that can used to support the health care practitioner in this endeavor. Further research is necessary to explore the effectiveness of these models, and how they impact cardiovascular outcomes cross-culturally.
Acknowledgments
The authors would like to thank Professor Changqing Pan, Chairman and Xiaoxin Liu, Director of Nursing Department at Shanghai Chest Hospital.
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the editorial office, Shanghai Chest. The article did not undergo external peer review.
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/shc.2019.02.01). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- American Heart Association. Heart Disease and Stroke Statistics 2017: At-a-Glance. Available online: https://healthmetrics.heart.org/wp-content/uploads/2017/06/Heart-Disease-and-Stroke-Statistics-2017-ucm_491265.pdf
- Baptiste D. Who you are and where you live can determine how long you live: What nurses need to know about cardiovascular disease among low-income urban-dwelling minority communities. J Clin Nurs 2018;27:3441-2. [Crossref] [PubMed]
- Guo C, Zheng X. Health Challenges and Opportunities for an Aging China. Am J Public Health 2018;108:890-2. [Crossref] [PubMed]
- Han M, Shi XM, Cai C, et al. Evolution of non-communicable disease prevention and control in China. Glob Health Promot 2017;1757975917739621 [Epub ahead of print]. [PubMed]
- Chen WW, Gao RL, Liu LS, et al. China cardiovascular diseases report 2015: a summary. J Geriatr Cardiol 2017;14:1-10. [PubMed]
- Lewington S, Lacey B, Clarke R, et al. The Burden of Hypertension and Associated Risk for Cardiovascular Mortality in China. JAMA Intern Med 2016;176:524-32. [Crossref] [PubMed]
- Yancy CW, Jessup M, Bozkurt B, et al. 2017 ACC/AHA/HFSA Focused Update of the 2013 ACCF/AHA Guideline for the Management of Heart Failure: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Failure Society of America. Circulation 2017;136:e137-e161. [Crossref] [PubMed]
- Li Q, Li Z, Kang X, et al. Nursing Practice Guidelines of Acute Heart Failure. Chinese Nursing Management 2016;16:1179-88.
- Zhang J. Editorial of Nursing Practice Guideline of Acute Heart Failure. Chinese Nursing Management 2016;16:1189-90.
- University TJH. About Johns Hopkins Medicine. Maryland, USA. 2019. Accessed 31st January 2019. Available online: https://www.hopkinsmedicine.org/about/index.html
- Dang D, Dearholt S. Johns Hopkins Nursing Evidence-Based Practice: Model and Guidelines. 3rd edition. Indianapolis: Sigma Theta Tau, 2017.
- Institute TJB. The JBI Approach. 2016. Available online: http://joannabriggs.org/jbi-approach.html
- Pearson A, Wiechula R, Court A, et al. The JBI model of evidence-based healthcare. Int J Evid Based Healthc 2005;3:207-15. [PubMed]
- Jordan Z, Lockwood C, Munn Z, et al. Redeveloping the JBI Model of Evidence Based Healthcare. Int J Evid Based Healthc 2018;16:227-41. [Crossref] [PubMed]
-
Institute TJB Joanna Briggs Collaboration 2019 . Available online: http://joannabriggs.org/jbc.html - Cao Y, Davidson PM, DiGiacomo M. Cardiovascular disease in China: an urgent need to enhance the nursing role to improve health outcomes. J Clin Nurs 2009;18:687-93. [PubMed]
- Ding S, Deng Y, Lu S, et al. Knowledge and practice in cardiovascular disease prevention among hospital registered nurses: a cross-sectional study. J Clin Nurs 2017;26:3318-27. [Crossref] [PubMed]
- Stephens JD, Yager AM, Allen J. Smartphone Technology and Text Messaging for Weight Loss in Young Adults: A Randomized Controlled Trial. J Cardiovasc Nurs 2017;32:39-46. [Crossref] [PubMed]
- Butler J, Kalogeropoulos A. Hospital strategies to reduce heart failure readmissions: where is the evidence? J Am Coll Cardiol 2012;60:615-7. [Crossref] [PubMed]
- Xu J, Gallo JJ, Wenzel J, et al. Heart Failure Rehospitalization and Delayed Decision Making: The Impact of Self-care and Depression. J Cardiovasc Nurs 2018;33:30-9. [Crossref] [PubMed]
- Cajita MI, Denhaerynck K, Dobbels F, et al. Health literacy in heart transplantation: Prevalence, correlates and associations with health behaviors-Findings from the international BRIGHT study. J Heart Lung Transplant 2017;36:272-9. [Crossref] [PubMed]
- Zhao J, Liu X, Zhang W, et al. Evidence-based nursing outputs and hot spot analysis of the last 5 years in mainland China: Results of a bibliometric analysis. Int J Nurs Pract 2018;24:e12628 [Crossref] [PubMed]
- Babiker A, El Husseini M, Al Nemri A, et al. Health care professional development: Working as a team to improve patient care. Sudan J Paediatr 2014;14:9-16. [PubMed]
- Morton G, Masters J, Cowburn PJ. Multidisciplinary team approach to heart failure management. Heart 2018;104:1376-82. [Crossref] [PubMed]
- Fanari Z, Barekatain A, Kerzner R, et al. Impact of a Multidisciplinary Team Approach Including an Intensivist on the Outcomes of Critically Ill Patients in the Cardiac Care Unit. Mayo Clin Proc 2016;91:1727-34. [Crossref] [PubMed]
- Jennings C, Astin F. A multidisciplinary approach to prevention. Eur J Prev Cardiol 2017;24:77-87. [Crossref] [PubMed]
- Hall KL, Vogel AL, Stipelman B, et al. A Four-Phase Model of Transdisciplinary Team-Based Research: Goals, Team Processes, and Strategies. Transl Behav Med 2012;2:415-30. [Crossref] [PubMed]
- Cooper LA, Boulware LE, Miller ER 3rd, et al. Creating a transdisciplinary research center to reduce cardiovascular health disparities in Baltimore, Maryland: lessons learned. Am J Public Health 2013;103:e26-38. [Crossref] [PubMed]
- Innes K, Crawford K, Jones T, et al. Transdisciplinary care in the emergency department: A qualitative analysis. Int Emerg Nurs 2016;25:27-31. [Crossref] [PubMed]
Cite this article as: Baptiste DL, Li Q, Milesky JL, Wright R. Advancing cardiovascular care through nursing research, quality improvement, and evidence-based practice. Shanghai Chest 2019;3:13.


