Endoscopic thoracic sympathectomy or sympathicotomy versus clipping in the surgical management of primary hyperhidrosis: a systematic review and meta-analysis
Introduction
Primary hyperhidrosis affects males and females indifferently, mainly in adolescence, with an underestimated incidence due to the feeling of shame and guilt of patients. This pathology has important implications in the life of the subjects who are affected, sometimes causing problems in relationship and in social life. Over the years, numerous conservative and surgical medical treatments have been proposed. However, surgery appears to be the best strategy considering the limited invasiveness of modern techniques. The excision of sympathetic chain and ganglia (conventional sympathectomy, CS) or the interruption of sympathetic trunk (sympathicotomy, ST) at various levels based on the sweaty areas and the positioning titanium clips along the chain (sympathetic block, SB) are the most used methods. Many authors debate the validity of one or other technique. In this work, we have tried to identify which of the sympathectomy/sympathicotomy versus SB offers the best results.
Methods
A search strategy using a combination of free-text words, relevant MeSH terms and appropriate filters was designed; the searching strategy was developed in MEDLINE (via PubMed) from 2009 until 2019, without imposing any language restrictions. Records identified through our search strategy were imported into reference management software. Two authors worked independently to assess each identified study based on the eligibility criteria. The two independent reviewers when in disagreements assessed the risk of bias by discussion and consensus. The following items were extracted from each study if available: first author’s surname, publication year, surgical strategy, recurrence/failure and compensatory sweating. The meta-analysis was performed by combining the reported recurrence/failure and compensatory sweating results of the individual studies using a random effect model. The Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) Statement was used to improve the report of this systematic review.
Results
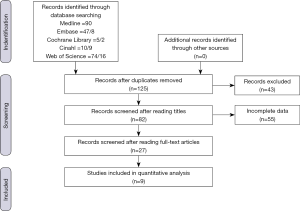
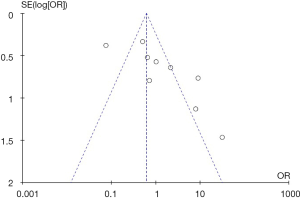
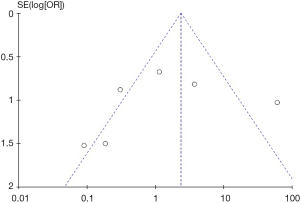
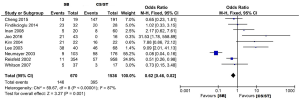
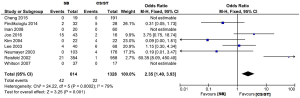
The selection of the articles was carried out by interrogating five databases: Medline, Scopus, Cinahl, Web of Science, Cochrane. The following search string was used: “hyperhidrosis AND (thoracic simpatic * OR clip *)”. Two hundred twenty-six results were obtained and, after the duplicates were removed, 125 articles were identified. Of these, only 82 were relevant after reading the title and the abstract. Afterwards only 49 were retained relevant after reading the full text. This step was performed independently by two researchers. In case of doubt, a third independent researcher was consulted. For the statistical analysis, 9 articles (1-9) were identified and taken into consideration (Figure 1). These provided overall information on 2,206 patients treated for primary hyperhidrosis. Of these, 670 patients were treated with a sympathetic chain clipping procedure and 1,536 were treated with endoscopic sympathectomy/sympathicotomy. Patients were divided into two distinct groups based on the parameters considered in this study. The first category included patients who developed compensatory hyperhidrosis, while the second category included patients with relapse/strategy failure. As far as compensatory hyperhidrosis is concerned, an asymmetry of the funnel graph to the right is evident. This suggests the presence of publication bias (Figure 2). Similarly, as regards the data relating to recurrences, an asymmetry of the funnel graph is evident, this time to the left. This suggests the presence of publication bias (Figure 3). As for the compensatory hyperhidrosis, the study of the graphs shows the presence of a considerable heterogeneity of the data. The latter is demonstrated by the value of I2 even by 87%. It must therefore be considered that the currently available studies do not reach a high level of statistical significance. However, the data in our possession indicate a stronger correlation between compensatory hyperhidrosis and the endoscopic sympathectomy/sympathetic procedure compared to clipping. This is confirmed by an odds ratio of 0.62 (Figure 4). Therefore, it is less frequently found in patients subjected to clipping. As for the rate of recurrence/failure of treatment, the graphs show once again a considerable heterogeneity, demonstrated by the value of I2 even by 79%. Therefore, even in this case, the currently available studies do not reach a high statistical significance. Nevertheless, the data in possession indicate a strong correlation between recurrence/failure rate and the clipping procedure compared to that of endoscopic sympathectomy/sympathicotomy. This is confirmed by an odds ratio of 2.35 (Figure 5). The clear benefit of CS/ST against relapses is therefore evident compared to the SB technique.
Discussion
In primary hyperhidrosis, surgery is now considered the treatment of choice. Alternatives to surgery have limited or temporary efficacy (10). Modern video-assisted thoracoscopic surgery (VATS) techniques allow the interruption or section of the sympathetic chain at different levels (11,12). The advantages are considerable in terms of effectiveness, recurrence rate and complications. However, it is necessary to consider the risk of complications both intraoperative such as hemorrhage, irreversible ganglia injury (such as the lesion of the stellate ganglion resulting in Horner’s syndrome) and postoperative such as pneumothorax, compensatory hyperhidrosis, strategy relapse/failure (13-16). The choice of the best technique is a debated topic. According to many authors, CS/ST would be preferred but there are also some variations with respect to the standard method as the Wittmoser technique where the communicating branches are interrupted to avoid the failure of the surgical strategy. Other authors instead consider the irreversible interruption of the sympathetic chain to be unsafe and prefer the block through the positioning of metal clips along the course of the chain itself, with the possibility of removing the latter in case of adverse events. Reversibility is the major advantage of this method as opposed to the CS/ST which is a very effective but irreversible procedure (17-19). According to the data emerging from our analysis, “clipping” is characterized by a slightly lower or almost overlapping compensatory hyperhidrosis rate compared to CS/ST although some authors believe that compensatory hyperhidrosis is independent of the method used (20). Furthermore, the strategy relapse/failure rate is significantly higher. Considering these data and according to the experience of many authors, the irreversible excision/interruption of the sympathetic chain should be preferred for several reasons. In fact, the interventions are similar in terms of invasiveness, present the same risks and require an equal hospitalization period (21,22). Moreover, a limitation of the SB is represented by the impossibility to selectively interrupt the communicating branches given the small size of the latter. This is often the cause of relapse/strategy failure. In regard to the possibility of removing the clips, it should be emphasized that the fibrotic phenomena, which often occurs a few days after the operation, makes this procedure sometimes difficult or even impossible to complete. Also, the removal is characterized by a high risk of complications, involves a greater discomfort for patients who have to undergo a double operation and often does not may restore the nerve to the original functionality (23,24). In conclusion, considering the results emerged from the analysis of the data present in the literature we believe that sympathectomy/sympathicotomy is the preferred techniques in terms of efficacy and complication rate.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editors (Federico Raveglia and Marco Scarci) for the series “Hyperhidrosis Management: from Diagnosis to Therapy” published in Shanghai Chest. The article has undergone external peer review.
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/shc.2019.07.08). The series “Hyperhidrosis Management: from Diagnosis to Therapy” was commissioned by the editorial office without any funding or sponsorship. LB serves as an unpaid editorial board member of Shanghai Chest from Jun 2017 to May 2019. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Cheng A, Johnsen H, Chang MY. Patient Satisfaction after Thoracoscopic Sympathectomy for Palmar Hyperhidrosis: Do Method and Level Matter? Perm J 2015;19:29-31. [PubMed]
- Findikcioglu A, Kilic D, Hatipoglu A. Is clipping superior to cauterization in the treatment of palmar hyperhidrosis? Thorac Cardiovasc Surg 2014;62:445-9. [PubMed]
- Inan K, Goksel OS, Uçak A, et al. Thoracic endoscopic surgery for hyperhidrosis: comparison of different techniques. Thorac Cardiovasc Surg 2008;56:210-3. [Crossref] [PubMed]
- Joo S, Lee GD, Haam S, et al. Comparisons of the clinical outcomes of thoracoscopic sympathetic surgery for palmar hyperhidrosis: R4 sympathicotomy versus R4 sympathetic clipping versus R3 sympathetic clipping. J Thorac Dis 2016;8:934-41. [Crossref] [PubMed]
- Kim DY, Paik HC, Lee DY. Comparative analysis of T2 selective division of rami-communicantes (ramicotomy) with T2 sympathetic clipping in the treatment of craniofacial hyperhidrosis. Eur J Cardiothorac Surg 2004;26:396-400. [Crossref] [PubMed]
- Lee DY, Paik HC, Kim DH, et al. Comparative analysis of T3 selective division of rami communicantes (ramicotomy) to T3 sympathetic clipping in treatment of palmar hyperhidrosis. Clin Auton Res 2003;13:I45-7. [Crossref] [PubMed]
- Neumayer C, Zacherl J, Holak G, et al. Experience with limited endoscopic thoracic sympathetic block for hyperhidrosis and facial blushing. Clin Auton Res 2003;13:I52-7. [Crossref] [PubMed]
- Reisfeld R, Nguyen R, Pnini A. Endoscopic thoracic sympathectomy for hyperhidrosis: experience with both cauterization and clamping methods. Surg Laparosc Endosc Percutan Tech 2002;12:255-67. [Crossref] [PubMed]
- Whitson BA, Andrade RS, Dahlberg PS, et al. Evolution of clipping for thoracoscopic sympathectomy in symptomatic hyperhidrosis. Surg Laparosc Endosc Percutan Tech 2007;17:287-90. [Crossref] [PubMed]
- Panhofer P, Gleiss A, Eilenberg WH, et al. Long-term outcomes after endothoracic sympathetic block at the T4 ganglion for upper limb hyperhidrosis. Br J Surg 2013;100:1471-7. [Crossref] [PubMed]
- Choi BC, Lee YC, Sim SB. Treatment of palmar hyperhidrosis by endoscopic clipping of the upper part of the T4 sympathetic ganglion. Preliminary results. Clin Auton Res 2003;13:I48-51. [Crossref] [PubMed]
- Lee DY, Hong YJ, Shin HK. Thoracoscopic sympathetic surgery for hyperhidrosis. Yonsei Med J 1999;40:589-95. [Crossref] [PubMed]
- Du X, Zhu X, Wang T, et al. Compensatory hyperhidrosis after different surgeries at the same sympathetic levels: a meta-analysis. Ann Transl Med 2018;6:203. [Crossref] [PubMed]
- Henteleff HJ, Kalavrouziotis D. Evidence-based review of the surgical management of hyperhidrosis. Thorac Surg Clin 2008;18:209-16. [Crossref] [PubMed]
- Lin TS, Huang LC, Wang NP, et al. Video-assisted thoracoscopic T2 sympathetic block by clipping for palmar hyperhidrosis: analysis of 52 cases. J Laparoendosc Adv Surg Tech A 2001;11:59-62. [Crossref] [PubMed]
- Moya J, Ramos R, Morera R, et al. Results of high bilateral endoscopic thoracic sympathectomy and sympatholysis in the treatment of primary hyperhidrosis: a study of 1016 procedures. Arch Bronconeumol 2006;42:230-4. [PubMed]
- Sciuchetti JF, Corti F, Ballabio D, et al. Results, side effects and complications after thoracoscopic sympathetic block by clamping. The monza clinical experience. Clin Auton Res 2008;18:80-3. [Crossref] [PubMed]
- Stefaniak TJ, Ćwigoń M. Long-term results of thoracic sympathectomy for primary hyperhidrosis. Pol Przegl Chir 2013;85:247-52. [Crossref] [PubMed]
- Sugimura H, Spratt EH, Compeau CG, et al. Thoracoscopic sympathetic clipping for hyperhidrosis: long-term results and reversibility. J Thorac Cardiovasc Surg 2009;137:1370-6. [Crossref] [PubMed]
- Moya J, Ramos R, Vives N, et al. Compensatory sweating after upper thoracic sympathectomy. Prospective study of 123 cases. Arch Bronconeumol 2004;40:360-3. [PubMed]
- Lin TS, Huang LC, Wang NP, et al. Endoscopic thoracic sympathetic block by clipping for palmar and axillary hyperhidrosis in children and adolescents. Pediatr Surg Int 2001;17:535-7. [Crossref] [PubMed]
- Fibla JJ, Molins L, Mier JM, et al. Effectiveness of sympathetic block by clipping in the treatment of hyperhidrosis and facial blushing. Interact Cardiovasc Thorac Surg 2009;9:970-2. [Crossref] [PubMed]
- Hynes CF, Yamaguchi S, Bond CD, et al. Reversal of sympathetic interruption by removal of clips. Ann Thorac Surg 2015;99:1020-3. [Crossref] [PubMed]
- Thomsen LL, Mikkelsen RT, Derejko M, et al. Sympathetic block by metal clips may be a reversible operation. Interact Cardiovasc Thorac Surg 2014;19:908-13. [Crossref] [PubMed]
Cite this article as: Divisi D, Zaccagna G, Di Francescantonio W, Bardhi D, Calvaruso F, Bertolaccini L, Crisci R. Endoscopic thoracic sympathectomy or sympathicotomy versus clipping in the surgical management of primary hyperhidrosis: a systematic review and meta-analysis. Shanghai Chest 2019;3:36.