Pneumonectomy for trauma and war casualties
Introduction
At Edwin Smith Surgical Papyrus written around 3000 bc (1) one can find the first report for thoracic trauma. The Iliad from Homer has details of thoracic injuries at battle of Troy.
Baron Dominic-Jean Larrey, Napoleon’s great surgeon, successfully managed an open chest wound by immediate trapping of sucking wounds, not allowing time for blood to escape (2). In the Civil War, open chest wounds were hermetically sealed, to prevent hemorrhage but not to improve breathing and inevitable the mortality rate was 62.6% for penetrating wounds of the chest (3), that represented 8% of all wounds (2). At these times there were almost no recognition and understanding of the pleural space physiology, addressed for the first time by Sauerbruch with his famous cage.
Major advances in medicine during the time period between World War I and World War II in the field of intratracheal anesthesia, lung resection surgery and treatment of heart wounds were critical for the results improvement in chest trauma victims.
In 1942, Dolley and Brewer (4) stated “At the outset, the problems are primarily those of mechanical derangement of the thoracic organs and hemorrhage, while later, infection assumes a dominant role.”. The standard care of thoracic trauma war victims was: cover open wounds; aspiration of pneumothorax, hemothorax and hemo- or pneumopericardium; maintain the bronchial tree free from blood or secretions and support paradoxal movements of the thorax. Intratracheal anesthesia was recommended for all patients undergoing thoracotomy (2). During World War II, a study on the approach of the thoracic trauma victims proved the superiority of the physiological approach, becoming the official policy for treating chest wounds in the Mediterranean Field of Operations.
War is always a dramatic environment with challenging clinical situations that can be used in elective surgery.
Mortality for chest wounds in war improved dramatically over the time and civil or elective surgery for other reasons evolved based on the principles acquired in War to turn thoracic surgery into the safe practice we witness today (2).
Although pneumonectomy has always been considered the simplest anatomic lung resection from a technical point of view the first successful left-sided pneumonectomy, for lung cancer, was only achieved in 1933 (5) by Graham and Singer.
Pneumonectomy is a severe amputation of organ function that should only be performed when the benefit outcomes the risks.
In lung cancer and benign lesions—destroyed lung—the indications are defined and usually there is time to study and decide in a weighted manner whether that patient should or not be submitted to a pneumonectomy.
As in any other context for lung resection, in major trauma and war, pneumonectomy should always be the last resort as it carries the highest rate of postoperative mortality.
Following a thoracic trauma, a patient has a pneumothorax, hemothorax, hemopericardium, lung contusion, heart contusion or a combination of this. The treatment of all of entities is mainly achieved by thoracic drainage and conservative measures which are effective in the vast majority of chest trauma patients. The need for urgent thoracotomy is reported between 1.1% and 12% (6-10). Of the patients that needed emergency thoracotomy, direct repair of the wound or less-than-pneumonectomy resections are the most frequent, with pulmonary resection being done in around 3.5% (10). The need for pneumonectomy has been reported to be between 0.01% (11) and 1.1% (6). However, major trauma with disrupture of the major vessels at the hilar level or main bronchi disruption beyond repair will always exist and the thoracic surgeon must always be prepared for the possibility of pneumonectomy to damage control.
Reported mortality after pneumonectomy in the major trauma setting is reported to be as high as 100% (12).
With this paper, the authors aim to review the literature on outcomes of pneumonectomy in the context of major trauma and war and evaluate the role of this surgery in the third millennium.
Methods
A search in the literature was made using the PubMed database. The authors searched using the query “trauma AND pneumonectomy”, “emergency pneumonectomy”, “trauma AND lung resection” or “emergency AND lung resection” and papers that reported results on outcomes were selected. Afterwards references were searched manually for further selection. Articles in languages other than English were considered only in the cases of high-volume series. References were added manually to the reference manager software Bookends v13.0.6 by Sonny software.
Results
The PubMed search retrieved 405 results. Afterwards selection was made by including papers referring to the specific context of thoracic trauma and included data on thoracotomies, type of lung resection made and outcomes.
The final result was 9 papers reporting series of trauma patients with need for lung resection, including pneumonectomy.
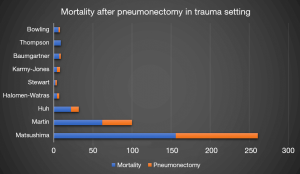
The mortality rate for pneumonectomy after thoracic trauma was between 50% and 100% (12-20), as illustrated in Figure 1.
Martin et al. (17) and Matsushima et al. (18) analyzed the data of the National Trauma Data Bank in the period from 1994 until 2003 and 2007 until 2014 respectively reported an incidence of 0.01% to 0.2% of pneumonectomy of all patients with blunt and penetrating thoracic trauma. Overall in-hospital mortality was 62% for the first period and 59.8% for the second.
Sub-analysis of patients with isolated pulmonary injury showed a stepwise increase in mortality by extent of resection: 19% for wedge resection, 27% for lobectomy, and 53% for pneumonectomy, as expected, reflecting both the trauma severity and the extension of lung resection.
Demirhan et al. (21) report the experience of 4,205 patients with chest trauma over a 10-year period. Only 255 patients needed thoracotomy (6%) with the need for pneumonectomy in 48 cases, corresponding to 18.8% of all thoracotomies. The authors report a global mortality rate of 9.3% but do not report the specific mortality rate after lung resection or pneumonectomy.
Huh et al. (20) report a retrospective study including all patients in a level I trauma center requiring thoracotomy for pulmonary injuries in a 15-year period. The authors reported 397 thoracotomies after thoracic trauma in the study period, with need for pneumonectomy in 33 of patients, 8% of all thoracotomies. Overall in-hospital mortality was 27%. Mortality increased in a stepwise fashion from tractotomy (9%) to wedge resection (20%), pneumorrhaphy (24%), lobectomy (35%) and pneumonectomy was the subgroup with the highest score of 69.7%.
Halonen-Watras et al. (15) report the need for pneumonectomy in 7 cases (1.2%) out of 580 patients who needed emergency thoracotomy, during a 6-year period. The global number of patients admitted for thoracic trauma was 2,088. Overall in-hospital mortality after pneumonectomy was 57%.
Karmy-Jones et al. (16) report the experience of 143 patients requiring lung resection after thoracic trauma over a 3-year period (1995–1998). Eight patients needed pneumonectomy. Overall in-hospital mortality after pneumonectomy was 50%.
Stewart et al. (19) report a 10-year retrospective review of 2,455 patients with chest trauma. One hundred and eighty-three patients (7.5%) needed thoracotomy and 32 required lung resections. Only 4 cases underwent pneumonectomy and overall in-hospital mortality after pneumonectomy was 50%.
Baumgartner et al. (13) report a series of 9 cases of pneumonectomy after thoracic trauma in the period from 1980 to 1994. Overall in-hospital mortality was 77.8%.
Thompson et al. (12) and Bowling et al. (14) published 1988 and 1985, respectively, a series of 9 and 8 pneumonectomies after thoracic trauma with a 100% and 75% in-hospital mortality rate.
Velmahos et al. (22) paper reports a 4-year period with 40 cases of thoracotomy after chest trauma. They report only 1 case of need for pneumonectomy that didn’t survive the postoperative period.
All major series were concordant in reporting a higher mortality rate after blunt trauma comparing to penetrating trauma (17,18,20,21), as reported in Table 1.
Table 1
| Papers | Blunt trauma mortality, % | Penetrating trauma mortality, % |
|---|---|---|
| Matsushima | 77.6 | 49.1 |
| Martin | 37 | 30 |
| Demirhan* | 6.8 | 1.4 |
| Huh | 63 | 18 |
*, Demirhan reports global mortality for all thoracic trauma patients, not only pneumonectomy.
Additionally, associated injuries in other systems as abdominal or head trauma was associated with higher mortality (17,18,21). Associated trauma was more often present in the blunt trauma comparing with penetrating trauma.
The association of thoracic trauma and head trauma resulted in an odds ratio (OR) 2.11 for mortality (18).
The authors couldn’t find any specific publication that would report outcomes after pneumonectomy (2) in war context. Brewer reports the mortality after chest trauma in World War II as 6.9% for simple wounds, 12.4% for thoracotomy and 27.3% for thoracoabdominal wounds and compares with global mortality after chest wound during World War I of 56% (2).
Infection was a major concern in the war scenario and chest trauma victims were transferred from the war front lines to the base hospitals and many had to undergo surgery for decortication, performed for the first time in World War II by Major Burford in April 1943 (2), and a rate of success in lung expansion and infection control was reported in 75% of patients.
In Vietnam War, Brewer reports a need for thoracotomy in 20.8% of 159 thoracic trauma victims in a 3-month period during war, with a global mortality rate of 7.9% (2).
A report form Senanayake et al. (23) of thoracic surgery during Iraq and Afghanistan Wars identified 184 patients with thoracic trauma who needed evacuation and referral to base hospitals in the UK, in the time period from March 2006 to March 2011. The need for thoracotomy was 20% and no type of lung resection is reported. Global overall mortality for the 184 patients was 4.9%. The authors warn that a cardiothoracic department was referred only in 39% of the cases.
Discussion
Pneumonectomy after severe chest trauma is a procedure of extremely high risk.
The pathophysiology of severe hypoxia and progressive pulmonary hypertension creates a vicious cycle of heart failure and ultimately death. Pulmonary edema after massive fluid resuscitation also play a role in this process. Pulmonary contusion and adult respiratory distress syndrome will increase pulmonary vascular resistance and increase the workload on the right heart, contributing to this process.
However, the need for pneumonectomy will only appear in the severe trauma with lesions beyond repair in whom no action will inevitably lead to death.
Therefore, the thoracic surgeon of the third millennium must be ready to promptly perform such a surgery, having in mind the balance between trying the repair by lung sparing procedures methods, such as direct repair, tractotomy or less-than-pneumonectomy lung resections, and prolong the time to patients’ stabilization. Early hilar control may play a fundamental role in both stabilizing and lesion assessment for decision making. Wiencek et al. (24) report a possible positive impact on survival from early hilar control after thoracotomy in this scenario.
Wagner et al. (25) hypothesize that simultaneously stapled pneumonectomy may have similar survival the individual ligation with much quicker operative times—88.9±14.3 vs. 213.0±57.8 minutes, respectively, P=0.01.
The patient exsanguinating, in hypovolemic shock in whom massive fluid resuscitation in being made, is particularly ate risk after pneumonectomy.
All the mentioned papers report the minimum mortality of 50% and this rate is not expected to lower in the future. Mortality is not related to the technical complexity of the pneumonectomy but to the mechanism of the trauma, associated injuries and patient presentation aggravated by the impact of resecting one lung.
Fortunately, only a small proportion of the thoracic trauma patients will have injuries that can only be controlled by pneumonectomy.
A word of caution to blunt trauma as it is, undoubtfully, associated with higher mortality comparing to penetrating trauma of the chest, not only in the context or emergent thoracotomy but also by the severe contusion and associated acute respiratory distress syndrome (ARDS) that have a worst prognosis.
The extremely severe patients in whom pneumonectomy is needed may have in this procedure their only hope and, therefore, we advocate for fast decision in this rare scenario.
Although the papers analyzed are focused on the immediate postoperative period, there is a theoretical increased risk for bronchopleural fistula due to compromised healing in hypovolemic shock scenario and this should be surveilled after discharge. After stabilization and before closing, bronchial stump reinforcement can be performed if the conditions allow it. However, bronchial closure technique may not be adequate in the emergency and bleeding scenario and some authors recommend staplers as they may provide a safer alternative (11,25).
Most of the papers report road traffic accidents (21) as the major cause for thoracic trauma, followed by accidental falls. In war, the pattern of injury will probably be more severe and complex. A recent report reflecting Iraq and Afghanistan Wars reported a 73% of victims of explosion (23).
To our knowledge, literature on lung surgery in war is scarce. No papers in the last decade were found but important information and data is found in literature between 1960 and 1970.
To the authors’ view, war may pose a special problem with even worse outcomes. The proportion of major trauma due to high-energy projectiles or explosions will certainly be higher, as well as patients with associated head or abdominal trauma. Emergency thoracotomies in campaign hospitals and the lack of infrastructure to support complex postoperative care will also be a factor.
In this scenario, damage control surgery will play a fundamental role (26), not only to avoid bad outcomes but also to lighten the high volume of major trauma in this scenario.
A temporary clamping of the hilar structures or a proper thoracic tamponade and quick transport to referral centers may have the potential to improve outcomes.
The historical note by Brewer (2) in Vietnam War underlines the importance of the mechanism of rapid evacuation form the battlefield to the frontline hospital—operation dust off—with an average of 40 minutes for transportation which allows for a medical approach in the very-early post trauma period.
Evolution in medical care and surgical techniques of thoracic lesions repair and damage have, undoubtfully, evolved much due to the input from war and military surgeons. Antibiotic therapy evolution after World War I was a major breakthrough in handling infections after trauma.
Data from the Pentagon after Vietnam War showed a global mortality rate of 3% of every hospitalized patient, and 84% of casualties returning to duty, what is major improvement comparing with older wars.
The fundamental principles to approach the chest wound victim developed during World War II have stood the test of time.
Additionally, improvements in protective equipment for combat troops resulted in low rates of thoracic injury, with a resultant rate of surgical intervention for thoracic or vascular repair of only 10% in recent conflicts (27).
Thoracic surgeons may have a fundamental role in war. As stated by Helsel et al. in 2016 (27), cardiothoracic surgeons provide skills fundamental in military surgery: general surgery training, proficiency in vascular techniques, routine care of critically ill patients, familiarity with basic and advanced techniques for hemorrhage control; capability to work in busy or mass casualty situations and expertise in critical care. Additionally, their presence may induce a sense of confidence and peace of mind to other members of the team and even increase the sense of security in combat forces (27).
The study published in 2014, reporting the experience in the UK during Iraq and Afghanistan Wars, by Senanayake et al. (23), assessed the outcomes of casualties with thoracic injuries repatriated to the UK and the impact of specialist cardiothoracic care hypothesize that victims repatriated to their home base facility are associated with low mortality and morbidity. Referral to cardiothoracic center was low—39%—and the authors believe that a more effective referral is critical to improve outcomes.
Conclusions
Pneumonectomy in chest trauma has a high mortality mainly related to the injury severity and associated lesions (brain and abdominal). All efforts should be made to preserve the organ and control the hemorrhage or air leak before deciding for the pneumonectomy, such as hilar control.
The presence of a thoracic or cardiothoracic surgeon in a war scenario is not only important to deal with chest trauma, but he is specially trained to deal and to lead a team in complex, emergent and life-threatening environments. The authors defend that a chest surgeon should always be involved in the approach of a severe trauma patient at the emergency room.
More investigation should be done in order to identify the actual causes of emergent pneumonectomy.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editors (Lorenzo Spaggiari and Luca Bertolaccini) for the series “The Role of Pneumonectomy in Thoracic Surgery in The Third Millennium” published in Shanghai Chest. The article has undergone external peer review.
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/shc.2019.10.08). The series “The Role of Pneumonectomy in Thoracic Surgery in The Third Millennium” was commissioned by the editorial office without any funding or sponsorship. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Breasted JH. The Edwin Smith Surgical Papyrus: published in facsimile and hieroglyphic transliteration with translation and commentary in two volumes. Chicago: University of Chicago Press, 1930.
- Brewer LA 3rd. Wounds of the chest in war and peace, 1943-1968. Ann Thorac Surg 1969;7:387-408. [Crossref] [PubMed]
- Coates JB Jr. Thoracic surgery. Washington: Office of the Surgeon General, Department. of the Army, 1963.
- Dolley FS, Brewer LA. Chest injuries. Ann Surg 1942;116:668-86. [Crossref] [PubMed]
- Graham EA, Singer JJ. Landmark article Oct 28, 1933. Successful removal of an entire lung for carcinoma of the bronchus. By Evarts A. Graham and J. J. Singer. JAMA 1984;251:257-60. [Crossref] [PubMed]
- Cakan A, Yuncu G, Olgaç G, et al. Thoracic trauma: analysis of 987 cases. Ulus Travma Derg 2001;7:236-41. [PubMed]
- Segers P, Van Schil P, Jorens P, et al. Thoracic trauma: an analysis of 187 patients. Acta Chir Belg 2001;101:277-82. [PubMed]
- Kiss L, Lăpădatu E, Balint I. The incidence of emergency thoracotomy in thoracic trauma. 7000 cases of thoracic trauma (T.T.) treated in the period of 1978-1995. Chirurgia (Bucur) 1997;92:269-75. [PubMed]
- Adebonojo SA. Management of chest trauma: a review. West Afr J Med 1993;12:122-32. [PubMed]
- Tominaga GT, Waxman K, Scannell G, et al. Emergency thoracotomy with lung resection following trauma. Am Surg 1993;59:834-7. [PubMed]
- Phillips B, Turco L, Mirzaie M, et al. Trauma pneumonectomy: a narrative review. Int J Surg 2017;46:71-4. [Crossref] [PubMed]
- Thompson DA, Rowlands BJ, Walker WE, et al. Urgent thoracotomy for pulmonary or tracheobronchial injury. J Trauma 1988;28:276-80. [Crossref] [PubMed]
- Baumgartner F, Omari B, Lee J, et al. Survival after trauma pneumonectomy: the pathophysiologic balance of shock resuscitation with right heart failure. Am Surg 1996;62:967-72. [PubMed]
- Bowling R, Mavroudis C, Richardson JD, et al. Emergency pneumonectomy for penetrating and blunt trauma. Am Surg 1985;51:136-9. [PubMed]
- Halonen-Watras J, O'Connor J, Scalea T. Traumatic pneumonectomy: a viable option for patients in extremis. Am Surg 2011;77:493-7. [PubMed]
- Karmy-Jones R, Jurkovich GJ, Shatz DV, et al. Management of traumatic lung injury: a Western Trauma Association Multicenter review. J Trauma 2001;51:1049-53. [Crossref] [PubMed]
- Martin MJ, McDonald JM, Mullenix PS, et al. Operative management and outcomes of traumatic lung resection. J Am Coll Surg 2006;203:336-44. [Crossref] [PubMed]
- Matsushima K, Aiolfi A, Park C, et al. Surgical outcomes after trauma pneumonectomy: Revisited. J Trauma Acute Care Surg 2017;82:927-32. [Crossref] [PubMed]
- Stewart KC, Urschel JD, Nakai SS, et al. Pulmonary resection for lung trauma. Ann Thorac Surg 1997;63:1587-8. [Crossref] [PubMed]
- Huh J, Wall MJ Jr, Estrera AL, et al. Surgical management of traumatic pulmonary injury. Am J Surg 2003;186:620-4. [Crossref] [PubMed]
- Demirhan R, Onan B, Oz K, et al. Comprehensive analysis of 4205 patients with chest trauma: a 10-year experience. Interact Cardiovasc Thorac Surg 2009;9:450-3. [Crossref] [PubMed]
- Velmahos GC, Baker C, Demetriades D, et al. Lung-sparing surgery after penetrating trauma using tractotomy, partial lobectomy, and pneumonorrhaphy. Arch Surg 1999;134:186-9. [Crossref] [PubMed]
- Senanayake EL, Poon H, Graham TR, et al. UK specialist cardiothoracic management of thoracic injuries in military casualties sustained in the wars in Iraq and Afghanistan. Eur J Cardiothorac Surg 2014;45:e202-3207. [Crossref] [PubMed]
- Wiencek RG Jr, Wilson RF. Central lung injuries: a need for early vascular control. J Trauma 1988;28:1418-24. [Crossref] [PubMed]
- Wagner JW, Obeid FN, Karmy-Jones RC, et al. Trauma pneumonectomy revisited: the role of simultaneously stapled pneumonectomy. J Trauma 1996;40:590-4. [Crossref] [PubMed]
- Garcia A, Martinez J, Rodriguez J, et al. Damage-control techniques in the management of severe lung trauma. J Trauma Acute Care Surg 2015;78:45-50; discussion 50-1. [Crossref] [PubMed]
- Helsel BS, David EA, Antevil JL. Special considerations of military cardiothoracic surgeons. J Thorac Cardiovasc Surg 2016;152:664-6. [Crossref] [PubMed]
Cite this article as: Santos Silva J, Calvinho PA, Olland A, Falcoz PE. Pneumonectomy for trauma and war casualties. Shanghai Chest 2020;4:2.