
Foreign body aspiration: a review of current strategies for management
Introduction and epidemiology
Aspiration of foreign objects into the airway presents an infrequent but potentially lethal clinical scenario. According to the National Electronic Injury Surveillance System, from 2000 to 2014, roughly 2,600 pediatric aspiration events occurred in American emergency departments (1). Nearly 300 annual deaths occur in the United States’ pediatric population related to foreign body aspiration (2). The incidences of adult aspiration events are fewer and less fatal (3,4). Airway foreign bodies are commonly classified as comprised of either inorganic or organic material (5). Epidemiological patterns regarding the type of item found in airways are influenced significantly by the patient’s age and demographics. For example aspiration of animal bone is reported more commonly in Asian countries whereas meat aspiration is reported more frequently in Western nations (6,7). Inorganic items are more common in children than adults (8). The size and structural features of aspirated foreign bodies impact the ultimate location of the item in the airway. Overall the majority of aspirated objects in retrospective studies were found in the right bronchus intermedius and truncus basalis (9,10).
Clinical symptoms
Structural attributes of airway foreign bodies along with patient co-morbidities impact initially presenting symptoms. Irrespective of the object’s features or location, the most common symptom (up to 90%) noted in several case series is cough, followed by dyspnea (1,3,7,11). In retrospective studies, objects obstructing distal airways were more likely to cause chest pain, wheezing, hemoptysis, and pneumonia. However, these symptoms were generally far less common than isolated cough (4,12). Patients with items localized in the upper airway and proximal lower airways including the trachea, and main bronchi, were more likely to complain of choking sensation, stridor, and change in voice or hoarseness (13,14). When comparing case series between children and adults, children are far more likely to have recollection of the precipitating aspiration events with onset of choking symptoms. In fact, fewer than half of adults recall an aspiration event and many do not correlate current symptoms with prior aspiration events (4,7). The delayed recognition of aspiration events and often non-specific symptoms may lead to complications related to foreign objects injuring the airways and lung parenchyma (15). These include but are not limited to granulation tissue, post-obstructive pneumonias, lung abscesses, bronchiectasis, cystic changes, pneumothorax and hemoptysis (16). Adult patients with pulmonary co-morbidities, such as chronic obstructive lung disease, are often more symptomatic in regard to common symptoms such as cough and dyspnea. Nonetheless, in most case series, preexisting pulmonary conditions did not seem to impact overall respiratory morbidity and mortality after foreign body removal (17).
Diagnostic imaging
Plain chest radiography (CXR) offers rapid and affordable evaluation for possible airway foreign bodies. However, only objects composed of radiopaque material are detectable. The majority of retrospective studies looking at imaging detection for foreign bodies found that CXR detected only about 20% to 50% of aspirated foreign bodies (18,19). Similarly, plain CXR can detect complications related to foreign airway bodies such as atelectasis, pneumonia, pneumothorax, and hyperinflation, but at a relatively low detection rate of 3% to 20% (20). Chest computed tomography (CT) has become the standard imaging modality used for the detection of foreign bodies in the respiratory tract. Several observational studies note sensitivities of nearly 100% and specificity ranging from 70–90% (21,22). Beyond identifying the presence and location of aspirated foreign bodies, chest CT scans provide crucial information regarding their orientation in the airway which is crucial to planning the therapeutic approach. Additionally, CT imaging provide more details regarding associated anatomic consequences from foreign bodies, such as lobar collapse, post-obstructive consolidation, early tree in bud opacification, parenchymal hemorrhage and mucous plugging (23). Advancement in post imaging processing and 3-D modeling, such as two dimensional multi-planar reformatted reconstructions, provide more detailed imaging and modeling of subtle airway abnormalities (24). However, further studies are warranted for determining the clinical implications of these adjunctive imaging techniques.
Objectives prior to object retrieval
Anticipatory guidance and pre-procedural planning are critical prior to any decision to perform therapeutic bronchoscopy for removing foreign bodies. Clinical presentation, imaging findings, type of object, and location of the object will influence the methods and tools to remove an item from the respiratory tract. Although pulmonologists are the primary providers in almost all observational studies involving retrieving aspirated objects, consultation with other airway specialists such anesthesiologists, otolaryngologists, and thoracic surgeons should be strongly considered depending on the clinical scenario. The bronchoscopy team should prepare multiple methods and expect to utilize multiple tools in anticipation to changes in the object’s morphology, the object’s location, and the patient’s clinical status during the retrieval process.
Rigid versus flexible bronchoscopy
Bronchoscopy remains the method of choice in nearly every published observational study regarding foreign body removal from the airway (7,25,26). Although flexible bronchoscopy is more widely used than rigid bronchoscopy, there are several benefits offered by the rigid bronchoscope in this setting (26). The solid steel barrel of the rigid bronchoscope protects and reinforces the trachea, larynx, and vocal cords, shielding such structures from injury when removing sharp or irregularly shaped objects. The large bore lumen of the rigid bronchoscope is also beneficial in allowing adequate ventilation even when moving large objects with the potential to obstruct conventional endotracheal tubes. Additionally, the greater luminal dimension allows for the use of larger, rigid forceps and multiple tools simultaneously (27,28). Flexible bronchoscopes are typically passed through the lumen of the rigid bronchoscope when angled manipulation is required. Rigid bronchoscopy is the therapeutic approach of choice for foreign body aspiration cases in the pediatric population. Due to the smaller respiratory tract anatomy in children, objects that have limited potential for oropharyngeal or tracheal obstruction in adults are a major source of critical airway obstruction in pediatric counterparts. Additionally, the smaller working channel and size of pediatric flexible bronchoscopes limits the use of many therapeutic tools (29). There are, however, several recent retrospective studies attesting to the success of foreign body removal through flexible bronchoscopy alone in children though a small number have required conversion to rigid bronchoscopy (30,31).
There are several considerations unique to rigid bronchoscopy which must be considered when deciding on the optimal therapeutic approach. First, it typically requires general anesthesia and an anesthesia team familiar with ventilation through the rigid barrel. The rigid bronchoscope does present additional risk of injury to the oropharynx, vocal cords, trachea though these risks are overall low. Overall, however the rate of airway-related complications in retrospective series of rigid bronchoscopy for foreign body retrieval are as low as 5% which may be attributed to increased training in the growing subspecialty field of interventional pulmonology (32,33). Generally, the need for specialized equipment and training amongst auxiliary staff and the need for experienced anesthesiologists limits the availability of rigid bronchoscopy to more specialized tertiary care centers.
The widespread availability of flexible bronchoscopy confers some benefits over rigid bronchoscopy. The procedure can be performed under moderate sedation. The small size and maneuverability have led to flexible bronchoscopy becoming the method of choice for retrieving foreign bodies found in peripheral airways. Newly developed ultrathin bronchoscopes allow operators to reach even further out in the periphery of the lung (34).
Anesthetic considerations
The approach to anesthesia for therapeutic bronchoscopy, including the need for general anesthesia and invasive airway management is impacted by the clinical presentation of the patient, the type of object aspirated and the radiographic findings. In retrospective studies containing children and adults with foreign airway body findings without severe dyspnea or central airway obstruction, topical anesthetics and agents for moderate sedation (diazepam, midazolam, fentanyl) were sufficient for the flexible bronchoscopy approach (35,36). For patients with both clinical or radiographic suggestion of central airway obstruction, or where there was potential for risk of airway injury, the use of general anesthesia and invasive airway management (laryngeal mask airway or endotracheal tube) was generally more common (35,37,38).
The presence of the cough and gag reflex during spontaneous ventilation can assist the repulsion of foreign airway bodies but can also hinder manipulation of the target. A retrospective study by Littman et al assessing the impact of spontaneous ventilation versus the use of neuromuscular blockade in 94 cases found no impact upon overall morbidity and mortality (39). For patients undergoing rigid bronchoscopy, observational studies have demonstrated that the use of manual jet ventilation directly through the rigid bronchoscope decreases the duration of intraoperative hypoxemia.
Bronchoscopy tools
There are several commercially available tools compatible with flexible bronchoscopes available for use during foreign body extraction, each with advantages in specific clinical scenarios and with particular types of aspirated materials (Table 1). Essentially all of these tools require removal with the tool, foreign body and bronchoscope en bloc as most foreign bodies requiring bronchoscopic removal are too large to be suctioned through the working channel of the flexible bronchoscope.
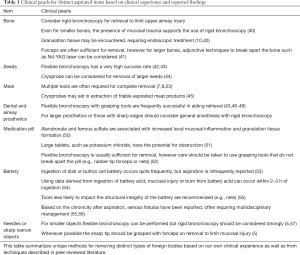
Full table
Grasping forceps
Both smooth forceps and forceps with teeth are commonly used to secure the edge of foreign bodies for removal. Smooth forceps are available with bare metallic forceps or forceps coated with rubber for additional grip. They are designed to grasp and maneuver smooth, narrow, and nonmalleable objects. Most major manufacturers recommend use for narrow and sharp items such as needles and pins. Forceps lined with teeth come in three variants: “alligator”, “rat tooth”, and combined rat tooth with alligator jaw. The use of rat-tooth forceps is particularly useful for solid objects which can be at least partly encompassed between the hinge and the teeth of the forceps. In nearly every large retrospective study where the type of tool was documented the majority of items were retrieved using some type of grasping forceps (35,58-60).
Baskets
Baskets are composed of four or more metallic wires that open when extended to allow positioning around objects then narrow when pulled back into the deployment sheath. They are designed to be placed around smooth, spherical, or spheroid objects that are too large to grasp and maneuver with forceps. In a retrospective study with 20 patients, Kim et al. described removing various inorganic and organic objects, mostly comprising of spherical features, at a 90% success rate (61).
Nets
Nets used during bronchoscopy are typically deployed through a deployment sheath and close when the distal end of the net is partly retracted into the sheath. They are designed for large, irregular objects. They require significant amount of maneuvering and thus are relegated to objects in the central airway.
Snares
Snares are comprised of a thin flexible wire that can tighten around the mid-section of foreign bodies for removal. They can use used for irregularly shaped objects though generally work best on more solid objects. They need some room for manipulation and thus are better suited for objects in the central airways. Several retrospective studies attest to successful object retrieval with snares, mainly in the central airway (49,59).
Fogarty balloon
The Fogarty balloon catheter is a small bore catheter with an inflatable tip of varying size which can be passed through the working channel of most flexible bronchoscopes. In the context of foreign body removal, it is often used to move objects from distal to central airways while preventing the object from moving distally into the airway. The catheter is first placed just distal to the object; the balloon is then inflated and the catheter is pulled proximally, pulling the object along with it. This technique was recently described by Hegde et al. in a retrospective series (62). The use of the Fogarty balloon catheter can help position a very distal foreign body in a more central airway where additional tools can be used for more definitive removal.
Cryoprobe
The flexible cryoprobe consists of a catheter that conducts nitrous oxide gas and rapidly freezes at the tip on contact. The thermodynamic mechanism utilizes the Joule-Thomson effect, in which a liquid in transitory phase drastically cools from change in high pressure to low pressure. The cryoprobe catheter is insulated to prevent temperature equilibration, except at the very tip. Consequently, items touching the tip of the cryoprobe freeze almost immediately (63). The freezing effect is mostly effective on water-rich materials and is therefore ideally suited for organic foreign bodies including aspirated vegetables and meat. The rapid freezing causes immediate cell injury to organic tissue, by causing the formation of intracellular and extracellular crystals (64). Due to the need for water content within the target of the cryoprobe, the cryoprobe has limited effect on cartilage, providing some protective benefit to central airway structures. Once the object freezes and attaches to the probe, both are retracted in tandem and the object is removed from the probe by re-warming the cryoprobe tip. There are several recent retrospective studies describing the use of cryoprobe in removing foreign bodies (65,66).
Post-operative care after foreign body removal from airway
Much of the published data on post-operative management after foreign body removal comes from the pediatric population. In the majority of retrospective studies for foreign body removal, patients were admitted to the hospital post procedure for monitoring with pulse oximetry and supportive care (7,38,59). In retrospective studies, there is discrepancy as to whether the type of object impacts pulmonary symptoms and time to recovery. Some retrospective studies found organic items were associated with prolonged pulmonary symptoms and recovery (defined by more than one week), while others found no difference in outcomes based on the type of aspirated material (16,67). The presence of lung parenchymal changes prior to the procedure, from infiltrate to nonspecific inflammatory changes, were found to be predictive of prolonged symptoms and hospitalization in most studies (16,67,68). Similarly patients with persistently abnormal lung radiography post-procedure had prolonged symptoms and hospitalization, highlighting the importance of obtaining imaging post procedure to identify at-risk patients (67,69). Patients with post-obstructive bronchiectasis related to foreign bodies also had prolonged hospitalization and frequently warrant anti-inflammatory medications, bronchodilators, chest physical therapy and in rare circumstances antibiotic therapy (16). However, there are no standardized data regarding pharmacologic therapy. Patients with difficult to remove, friable foreign bodies, or procedural complications frequently have prolonged symptoms. Moreover, in patients with friable objects and persistent symptoms or new radiographic findings, residual material or associated complications such as mucous plugging or fibrotic material were found on repeat bronchoscopy (7,70). Repeating bronchoscopy thus should be considered, especially in aspirated material which is more difficult to remove in a single setting. Beyond common respiratory symptoms, a high-risk adverse event noted in most large retrospective analyses in the pediatric population is laryngospasm, reported in anywhere from 10–60 percent of subjects (68,69,71). Careful post-operative monitoring is therefore critical to minimize morbidity after removal of airway foreign bodies.
Conclusions
Incidents of foreign body aspiration into the airway are less common in adults but remain a complex condition to manage. Clinical symptoms are often vague, especially in the adult population. Pre procedural planning and collaboration between airway specialists play central role in object extraction. Moreover, familiarity with the different types of bronchoscopy methods and tools are warranted for the most effective foreign body retrieval.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editors (Kyle Hogarth and Jonathan Kurman) for the series “Interventional pulmonology and advanced bronchoscopy” published in Shanghai Chest. The article was sent for external peer review organized by the Guest Editors and the editorial office.
Conflicts of Interest: Both authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/shc-20-38). The series “Interventional pulmonology and advanced bronchoscopy” was commissioned by the editorial office without any funding or sponsorship. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work and in ensuring that questions related to the accuracy or integrity of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Hanba C, Cox S, Bobian M, et al. Consumer product ingestion and aspiration in children: A 15-year review. Laryngoscope 2017;127:1202-7. [Crossref] [PubMed]
- Harris CS, Baker SP, Smith GA, et al. Childhood asphyxiation by food. A national analysis and overview. JAMA 1984;251:2231-5. [Crossref] [PubMed]
- Limper AH, Prakash UB. Tracheobronchial foreign bodies in adults. Ann Intern Med 1990;112:604-9. [Crossref] [PubMed]
- Baharloo F, Veyckemans F, Francis C, et al. Tracheobronchial foreign bodies: presentation and management in children and adults. Chest 1999;115:1357-62. [Crossref] [PubMed]
- Rafanan AL, Mehta AC. Adult airway foreign body removal. What's new? Clin Chest Med 2001;22:319-30. [Crossref] [PubMed]
- Mittleman RE, Wetli CV. The fatal cafe coronary. Foreign-body airway obstruction. JAMA 1982;247:1285-8. [Crossref] [PubMed]
- Chen CH, Lai CL, Tsai TT, et al. Foreign body aspiration into the lower airway in Chinese adults. Chest 1997;112:129-33. [Crossref] [PubMed]
- Skoulakis CE, Doxas PG, Papadakis CE, et al. Bronchoscopy for foreign body removal in children. A review and analysis of 210 cases. Int J Pediatr Otorhinolaryngol 2000;53:143-8. [Crossref] [PubMed]
- Yadav SP, Singh J, Aggarwal N, et al. Airway foreign bodies in children: experience of 132 cases. Singapore Med J 2007;48:850-3. [PubMed]
- Ramos MB, Fernandez-Villar A, Rivo JE, et al. Extraction of airway foreign bodies in adults: experience from 1987-2008. Interact Cardiovasc Thorac Surg 2009;9:402-5. [Crossref] [PubMed]
- Foltran F, Ballali S, Rodriguez H, et al. Inhaled foreign bodies in children: a global perspective on their epidemiological, clinical, and preventive aspects. Pediatr Pulmonol 2013;48:344-51. [Crossref] [PubMed]
- al-Majed SA, Ashour M, al-Mobeireek AF, et al. Overlooked inhaled foreign bodies: late sequelae and the likelihood of recovery. Respir Med 1997;91:293-6. [Crossref] [PubMed]
- Singh B, Kantu M, Har-El G, et al. Complications associated with 327 foreign bodies of the pharynx, larynx, and esophagus. Ann Otol Rhinol Laryngol 1997;106:301-4. [Crossref] [PubMed]
- Metrangelo S. Eight years' experience with foreign-body aspiration in children: what is really important for a timely diagnosis? J Pediatr Surg 1999;34:1229-31. [Crossref] [PubMed]
- Qureshi A, Behzadi A. Foreign-body aspiration in an adult. Can J Surg 2008;51:E69-70. [PubMed]
- Karakoç F, Karadag B, Akbenlioglu C, et al. Foreign body aspiration: what is the outcome? Pediatr Pulmonol 2002;34:30-6. [Crossref] [PubMed]
- Ng J, Kim S, Chang B, et al. Clinical features and treatment outcomes of airway foreign body aspiration in adults. J Thorac Dis 2019;11:1056-64. [Crossref] [PubMed]
- Silva AB, Muntz HR, Clary R. Utility of conventional radiography in the diagnosis and management of pediatric airway foreign bodies. Ann Otol Rhinol Laryngol 1998;107:834-8. [Crossref] [PubMed]
- Bai W, Zhou X, Gao X, et al. Value of chest CT in the diagnosis and management of tracheobronchial foreign bodies. Pediatr Int 2011;53:515-8. [Crossref] [PubMed]
- Pinto A, Scaglione M, Pinto F, et al. Tracheobronchial aspiration of foreign bodies: current indications for emergency plain chest radiography. Radiol Med 2006;111:497-506. [Crossref] [PubMed]
- Zissin R, Shapiro-Feinberg M, Rozenman J, et al. CT findings of the chest in adults with aspirated foreign bodies. Eur Radiol 2001;11:606-11. [Crossref] [PubMed]
- Pitiot V, Grall M, Ploin D, et al. The use of CT-scan in foreign body aspiration in children: A 6 years' experience. Int J Pediatr Otorhinolaryngol 2017;102:169-73. [Crossref] [PubMed]
- Yilmaz A, Akkaya E, Damadoglu E, et al. Occult bronchial foreign body aspiration in adults: analysis of four cases. Respirology 2004;9:561-3. [Crossref] [PubMed]
- Hegde SV, Hui PK, Lee EY. Tracheobronchial foreign bodies in children: imaging assessment. Semin Ultrasound CT MR 2015;36:8-20. [Crossref] [PubMed]
- Hsu AA. Endoscopic intervention of lower airway foreign matter in adults-a different perspective. J Thorac Dis 2015;7:1870-7. [PubMed]
- Blanco Ramos M, Botana-Rial M, Garcia-Fontan E, et al. Update in the extraction of airway foreign bodies in adults. J Thorac Dis 2016;8:3452-6. [Crossref] [PubMed]
- Nicastri DG, Weiser TS. Rigid Bronchoscopy: Indications and Techniques. Oper Tech Thorac Cardiovasc Surg 2012;17:44-51. [Crossref]
- Acharya K. Rigid Bronchoscopy in Airway Foreign Bodies: Value of the Clinical and Radiological Signs. Int Arch Otorhinolaryngol 2016;20:196-201. [Crossref] [PubMed]
- Martinot A, Closset M, Marquette CH, et al. Indications for flexible versus rigid bronchoscopy in children with suspected foreign-body aspiration. Am J Respir Crit Care Med 1997;155:1676-9. [Crossref] [PubMed]
- Tang LF, Xu YC, Wang YS, et al. Airway foreign body removal by flexible bronchoscopy: experience with 1027 children during 2000-2008. World J Pediatr 2009;5:191-5. [Crossref] [PubMed]
- Tenenbaum T, Kahler G, Janke C, et al. Management of Foreign Body Removal in Children by Flexible Bronchoscopy. J Bronchology Interv Pulmonol 2017;24:21-8. [Crossref] [PubMed]
- Lukomsky GI, Ovchinnikov AA, Bilal A. Complications of bronchoscopy: comparison of rigid bronchoscopy under general anesthesia and flexible fiberoptic bronchoscopy under topical anesthesia. Chest 1981;79:316-21. [Crossref] [PubMed]
- Diaz-Mendoza J, Peralta AR, Debiane L, et al. Rigid Bronchoscopy. Semin Respir Crit Care Med 2018;39:674-84. [Crossref] [PubMed]
- Hirai Y, Oura S, Yoshimasu T, et al. Removal of an endobronchial foreign body using an ultrathin flexible bronchoscope and a novel suction system. J Bronchology Interv Pulmonol 2013;20:363-4. [Crossref] [PubMed]
- Mise K, Jurcev Savicevic A, Pavlov N, et al. Removal of tracheobronchial foreign bodies in adults using flexible bronchoscopy: experience 1995-2006. Surg Endosc 2009;23:1360-4. [Crossref] [PubMed]
- Rodrigues AJ, Oliveira EQ, Scordamaglio PR, et al. Flexible bronchoscopy as the first-choice method of removing foreign bodies from the airways of adults. J Bras Pneumol 2012;38:315-20. [Crossref] [PubMed]
- Tan HK, Brown K, McGill T, et al. Airway foreign bodies (FB): a 10-year review. Int J Pediatr Otorhinolaryngol 2000;56:91-9. [Crossref] [PubMed]
- Nguyen LH, Nguyen DH, Tran TN, et al. Endobronchial foreign bodies in Vietnamese adults are related to eating habits. Respirology 2010;15:491-4. [Crossref] [PubMed]
- Litman RS, Ponnuri J, Trogan I. Anesthesia for tracheal or bronchial foreign body removal in children: an analysis of ninety-four cases. Anesth Analg 2000;91:1389-91. TOC. [Crossref] [PubMed]
- Fang YF, Hsieh MH, Chung FT, et al. Flexible bronchoscopy with multiple modalities for foreign body removal in adults. PLoS One 2015;10:e0118993 [Crossref] [PubMed]
- Mahajan AK, Khandhar SJ. Successful Bronchoscopic Removal of a Chicken Bone Lodged in the Airway for 4 Years. Am J Respir Crit Care Med 2016;194:e8-e9. [Crossref] [PubMed]
- Ramírez-Figueroa JL, Gochicoa-Rangel LG, Ramirez-San Juan DH, et al. Foreign body removal by flexible fiberoptic bronchoscopy in infants and children. Pediatr Pulmonol 2005;40:392-7. [Crossref] [PubMed]
- Swanson KL, Prakash UB, Midthun DE, et al. Flexible bronchoscopic management of airway foreign bodies in children. Chest 2002;121:1695-700. [Crossref] [PubMed]
- Sehgal IS, Dhooria S, Behera D, et al. Use of cryoprobe for removal of a large tracheobronchial foreign body during flexible bronchoscopy. Lung India 2016;33:543-5. [Crossref] [PubMed]
- Rubio E, Gupta P, Ie S, et al. Cryoextraction: A novel approach to remove aspirated chewing gum. Ann Thorac Med 2013;8:58-9. [Crossref] [PubMed]
- Conte SC, De Nardi E, Conte F, et al. Aspiration of tracheoesophageal prosthesis in a laryngectomized patient. Multidiscip Respir Med 2012;7:25. [Crossref] [PubMed]
- Mahmoud M, Imam S, Patel H, et al. Foreign body aspiration of a dental bridge in the left main stem bronchus. Case Rep Med 2012;2012:798163 [Crossref] [PubMed]
- Fidkowski CW, Zheng H, Firth PG. The anesthetic considerations of tracheobronchial foreign bodies in children: a literature review of 12,979 cases. Anesth Analg 2010;111:1016-25. [Crossref] [PubMed]
- Ichimura H, Maeda M, Kikuchi S, et al. Endobronchial dental prosthesis retrieval by a snare technique using a flexible bronchoscope and fluoroscopy: Two case reports and technical tips. Respir Med Case Rep 2016;19:187-9. [Crossref] [PubMed]
- Lee P, Culver DA, Farver C, et al. Syndrome of iron pill aspiration. Chest 2002;121:1355-7. [Crossref] [PubMed]
- Mehta AC, Khemasuwan D. A foreign body of a different kind: Pill aspiration. Ann Thorac Med 2014;9:1-2. [Crossref] [PubMed]
- Küpeli E, Khemasuwan D, Lee P, et al. "Pills" and the air passages. Chest 2013;144:651-60. [Crossref] [PubMed]
- McLarty JD, Krishnan M, Rowe MR. Disk battery aspiration in a young child: a scarcely reported phenomenon. Arch Otolaryngol Head Neck Surg 2012;138:680-2. [Crossref] [PubMed]
- Leinwand K, Brumbaugh DE, Kramer RE. Button Battery Ingestion in Children: A Paradigm for Management of Severe Pediatric Foreign Body Ingestions. Gastrointest Endosc Clin N Am 2016;26:99-118. [Crossref] [PubMed]
- Wurzel DF, Masters IB, Choo KL, et al. A case for early bronchoscopic airway assessment after disc battery ingestion. Pediatr Pulmonol 2014;49:E72-4. [Crossref] [PubMed]
- Krom H, Visser M, Hulst JM, et al. Serious complications after button battery ingestion in children. Eur J Pediatr 2018;177:1063-70. [Crossref] [PubMed]
- Hasdiraz L, Bicer C, Bilgin M, et al. Turban pin aspiration: non-asphyxiating tracheobronchial foreign body in young islamic women. Thorac Cardiovasc Surg 2006;54:273-5. [Crossref] [PubMed]
- Debeljak A, Sorli J, Music E, et al. Bronchoscopic removal of foreign bodies in adults: experience with 62 patients from 1974-1998. Eur Respir J 1999;14:792-5. [Crossref] [PubMed]
- Dong YC, Zhou GW, Bai C, et al. Removal of tracheobronchial foreign bodies in adults using a flexible bronchoscope: experience with 200 cases in China. Intern Med 2012;51:2515-9. [Crossref] [PubMed]
- Goyal R, Nayar S, Gogia P, et al. Extraction of tracheobronchial foreign bodies in children and adults with rigid and flexible bronchoscopy. J Bronchology Interv Pulmonol 2012;19:35-43. [Crossref] [PubMed]
- Kim K, Lee HJ, Yang EA, et al. Foreign body removal by flexible bronchoscopy using retrieval basket in children. Ann Thorac Med 2018;13:82-5. [Crossref] [PubMed]
- Hegde S, Bahadur U, Kanojia RP, et al. Bronchoscopic Airway Foreign Body Extraction without Using Optical Forceps. J Indian Assoc Pediatr Surg 2018;23:87-9. [Crossref] [PubMed]
- Amoils SP. The Joule Thomson cryoprobe. Arch Ophthalmol 1967;78:201-7. [Crossref] [PubMed]
- DiBardino DM, Lanfranco AR, Haas AR. Bronchoscopic Cryotherapy. Clinical Applications of the Cryoprobe, Cryospray, and Cryoadhesion. Ann Am Thorac Soc 2016;13:1405-15. [Crossref] [PubMed]
- Sriratanaviriyakul N, Lam F, Morrissey BM, et al. Safety and Clinical Utility of Flexible Bronchoscopic Cryoextraction in Patients With Non-neoplasm Tracheobronchial Obstruction: A Retrospective Chart Review. J Bronchology Interv Pulmonol 2015;22:288-93. [Crossref] [PubMed]
- David AP, Xu MJ, Rosbe KW, et al. Cryoprobe retrieval of an airway foreign body: A case report and literature review. Int J Pediatr Otorhinolaryngol 2019;125:79-81. [Crossref] [PubMed]
- Chung MK, Jeong HS, Ahn KM, et al. Pulmonary recovery after rigid bronchoscopic retrieval of airway foreign body. Laryngoscope 2007;117:303-7. [Crossref] [PubMed]
- Roh JL, Hong SJ. Lung recovery after rigid bronchoscopic removal of tracheobronchial foreign bodies in children. Int J Pediatr Otorhinolaryngol 2008;72:635-41. [Crossref] [PubMed]
- Sjogren PP, Mills TJ, Pollak AD, et al. Predictors of complicated airway foreign body extraction. Laryngoscope 2018;128:490-5. [Crossref] [PubMed]
- Xu B, Wu L, Jin Z, et al. Residual airway foreign bodies in children who underwent rigid bronchoscopy. Int J Pediatr Otorhinolaryngol 2019;118:170-6. [Crossref] [PubMed]
- Zhang X, Li W, Chen Y. Postoperative adverse respiratory events in preschool patients with inhaled foreign bodies: an analysis of 505 cases. Paediatr Anaesth 2011;21:1003-8. [Crossref] [PubMed]
Cite this article as: Sarkar A, Murthy V. Foreign body aspiration: a review of current strategies for management. Shanghai Chest 2021;5:25.


