Annual report of thoracic surgery service at Shanghai Chest Hospital in 2019
Introduction
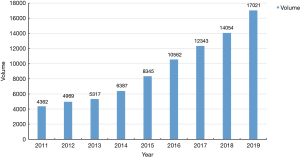
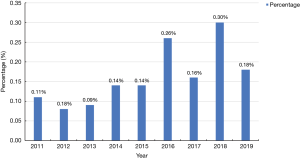
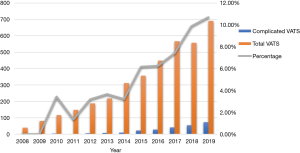
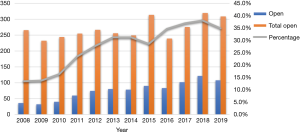
In running one of the largest thoracic surgery centers in China, the thoracic surgery team of the Shanghai Chest Hospital has exerted continuous effort in the surgical treatment of thoracic diseases. In 2019, a total 17,021 patients received thoracic surgeries at the hospital, including 14,591 pulmonary resections, 1,017 esophageal procedures, 1,089 mediastinal procedures, 59 tracheal procedures, and 9 lung transplantations. The total case volume increased by 21.1% compared to that of the year before, while the percentage of minimally invasive surgery (MIS) was as high as 89.8%, and included both video-assisted thoracic surgery (VATS) and robotic-assisted thoracic surgery (RATS) (Figure 1). The indication for minimally invasive surgery was no longer reserved solely for early-stage thoracic diseases, but was extended to those patients with locally advanced tumors, those who had received neoadjuvant therapy, and those needing complex reconstructions after extensive resection. Furthermore, the rate of major complications has remained low over the past years, with the in-hospital mortality rate being only 0.18% in 2019 (Figure 2). This report presents our surgery volume, the quality of our service, and our efforts to move thoracic surgery forward so as to better help our patients.
Methods
Patients
The data of patients receiving thoracic surgeries at the Department of Thoracic Surgery and the Department of Oncological Surgery of Shanghai Chest Hospital from January 2019 to December 2019 were retrospectively collected. These patients were classified into pulmonary, esophageal, mediastinal, tracheal, and lung transplantation divisions according to different diseases and surgical treatments they received. Additionally, data on the volume of surgical resections, the surgical types and approaches, the pathological subtypes, the perioperative outcomes, and other characteristics were collected.
Statistical analysis
Categorical and continuous variables are presented as frequencies (percentages) and mean ± standard deviation (SD). Bar, line, and pie graphs were plotted to visually represent the information. Statistical analysis was performed using SPSS v. 22.0 (IBM Corp., Armonk, NY, USA).
Results
Pulmonary surgeries
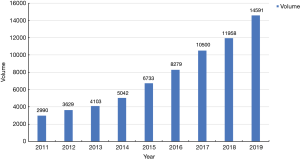
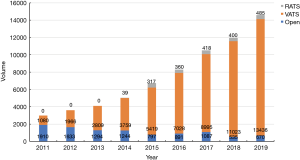
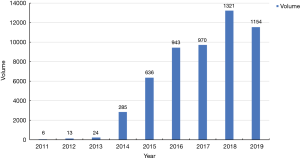
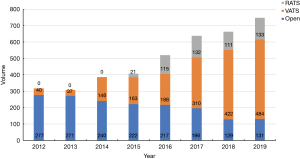
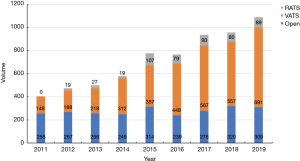
In 2019, a total of 14,591 patients with pulmonary diseases underwent surgical resections at the Shanghai Chest Hospital. This number represents a 22.0% increase from the year prior (Figure 3). Among these patients, 13,436 received VATS resection (92.1%), 485 patients received RATS resection (3.3%), and 670 patients received open thoracotomy (4.6%) (Figure 4).
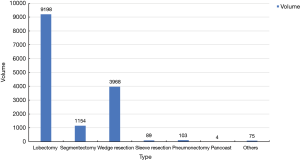
Of the 14,591 pulmonary patients, 12,886 (88.3%) were confirmed as having malignant diseases and 1,705 cases (11.7%) had benign diseases. The rate of malignancy among all pulmonary patients was as high as 88.3%. The most common surgical procedure was lobectomy (n=7,626, 63.0%), followed by wedge resection (n=3,968, 27.2%), segmentectomy (n=1,154, 7.9%), pneumonectomy (n=103, 0.7%), sleeve resection (n=89, 0.6%), Pancoast tumor resection (n=4, 0.02%), and others (n=75, 0.5%) (Figure 5). The volume of sublobar resections has been continuingly increasing over the past few years, owing to the increase in screening-detected small, early-stage lung cancers, especially those appearing as ground-glass opacities (GGO) on computed tomography (CT) scans. In 2019, the number of segmentectomies exceeded 1,100 cases, almost all of which were completed via minimally invasive approaches (Figure 6).
The thoracic surgery team at the Shanghai Chest Hospital has long been known for its expertise in complex pulmonary surgeries including Pancoast tumor resection, extended lobectomy, resection of stage T4 lung cancer, extrapleural pneumonectomy, etc. In addition to surgery for early-staged lung cancers, MIS also constituted a significant part of complicated pulmonary procedures for locally advanced disease. Among a total of 89 sleeve resections in 2019, 8 cases (9.0%) were successfully accomplished via MIS. In addition, VATS was successfully performed in 34 (33.0%) cases of the 103 pneumonectomies, 2 were conducted by RATS resection. Excellent perioperative results in these cases indicated that MIS is safe and feasible for complicated procedures, and more patients can be expected to benefit from similar advances in surgical techniques in the future.
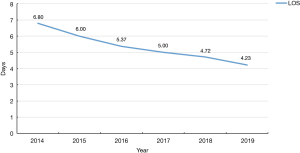
For the postoperative outcomes, the average length of hospital stays (LOS) after surgery was 4.23 days, and thus LOS has been successively reduced in each of the past 6 years as a consequence of the wider application of enhanced recovery after surgery (ERAS) concepts (Figure 7). The rate of major postoperative complications for pulmonary surgeries was only 9.2%, with in-hospital mortality being 0.048%.
In summary, the thoracic surgery team at Shanghai Chest Hospital made significant progress both in service volume and quality of pulmonary surgery in 2019. This is evidenced by the shortened LOS via the application of ERAS, and the increased use of MIS for complicated lung cancer surgeries in the treatment of locally advanced diseases.
Esophageal surgeries
The year 2019 was the first to see the total number of esophageal procedures exceed 1,000, reaching a historical height of 1,017. A total of 834 esophageal cancer patients and 183 patients with benign esophageal diseases received surgical treatment at the Shanghai Chest Hospital (Figure 8). Among the 748 esophagectomies, only 131 (17.5%) were open cases, while minimally invasive esophagectomies (MIE) accounted for the other 82.5% cases, including 484 (64.7%) video-assisted esophagectomies and 133 (17.8%) robotic-assisted esophagectomies (Figure 9).
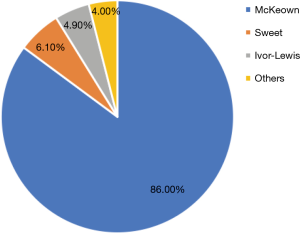
Similar to other populations in China, the vast majority of our esophageal cancer patients had tumors located in the thoracic esophagus, with 59 (7.9%) tumors in the esophageal-gastric junction (EGJ) and 24 (3.2%) in the cervical esophagus. The most common histology was squamous cell carcinoma (680, 90.9%), followed by adenocarcinoma (54, 7.2%), neuroendocrine carcinoma (12, 1.6%), and other types of malignant tumors (2, 0.3%). Accordingly, McKeown is still the most preferred procedure, being applied in 643 (86.0%) patients, followed by left-thoracic Sweet procedure in 46 (6.1%) patients, Ivor-Lewis procedure in 29 (4.9%) patients, and laryngo-pharyngo-esophagectomy or transhiatal esophagectomy in another 30 (4.0%) patients with cervical or EGJ lesions (Figure 10).
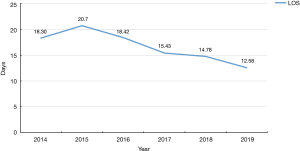
The 30-day mortality rate was a mere 0.4%, with a mean length of postoperative hospital stay of 12.58 days, representing a reduced LOS compared with the previous 6 years as consequence of ERAS adherence (Figure 11). The postoperative complication rate was 36.4%, and 27 (3.6%) patients experienced Clavien-Dindo grade III–IV complications.
Endoscopic submucosal dissection (ESD) has been increasingly used in patients with early (mucosal and superficial submucosal) esophageal cancers. Ninety-three cases of ESD were successfully completed in 2019, which represents an increase of 43.1% compared to 2018 (Figure 12). Only a single patient (1.1%) needed to undergo conversion to esophagectomy due to perforation during ESD. The mean LOS was 3.5±2.6 days, and no other major complications were observed. In addition, 7 patients with synchronous esophageal–hypopharyngeal cancers received ESD for their superficial hypopharyngeal lesion in combination with esophagectomy for esophageal cancer.
Notably, the number of patients with benign esophageal diseases increased by 31.7% compared to 2018. Among the 183 cases of benign esophageal disease, 39 (21.3%) had benign esophageal tumors, 14 (7.7%) had gastroesophageal reflux disease, 25 (13.7%) had hiatus hernias, 8 (4.4%) had diverticula, 8 (4.4%) had achalasia, 13 (7.1%) had tracheal-esophageal fistulae, 20 (10.9%) had benign esophageal stenoses, and 56 (30.6%) had other pathologies. Again, most of benign esophageal diseases were treated via minimally invasive approaches, including 58 (31.7%) endoscopic therapies, 61 (33.3%) thoracoscopic/laparoscopic-assisted surgeries, and 6 (3.3%) robotic-assisted surgeries.
Over the past year, the esophageal surgery division at the Shanghai Chest Hospital has constantly improved the minimally invasive techniques and endoscopic therapies for malignant and benign esophageal diseases. In the meantime, complex procedures like colonic and free-jejunum interposition for esophageal substitution, total laryngo-pharyngo-esophagectomy, and others, have also been attended to with persistent effort, particularly when treating difficult cases.
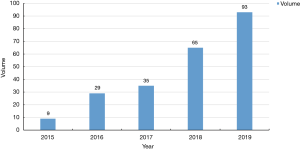
Mediastinal surgeries
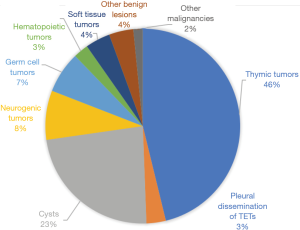
The total case volume of mediastinal procedures was also remarkable, and reached a historical peak of 1,089 in 2019. Again, MIS was the main approach, with 691 VATS procedures (63.5%) and 89 RATS procedures (8.2%). Open thoracotomy or median sternotomy was still needed in 309 patients, and thus 28.3% of our cases were challenging procedures for locally advanced diseases (Figure 13). Consistent with the increasing number of complicated surgeries (Figure 14), 2019 saw more patients receiving preoperative induction therapies (56 cases, 30.8% of stage III–IV patients) than the year before.
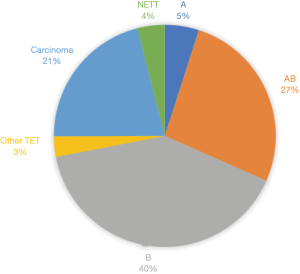
Among the 1,089 patients, 538 had thymic epithelial tumors (TET, including 35 cases with recurrent diseases), 254 had mediastinal cysts, 89 had neurogenic tumors, 75 had germ cell tumors, and 27 had hematopoietic tumors (Figure 15). Among the 503 primary TETs, 377 were thymomas (25 type A, 134 type AB, 203 type B, 15 other thymomas), 106 were thymic carcinomas, and 20 were neuroendocrine thymic tumors (NETT) (Figure 16). Of the 35 recurrent cases, 91% were type B thymomas presenting as pleural dissemination. Among the 75 germ cell tumors, 47 were teratomas, 5 were seminomas, 7 were yolk sac tumors, and 16 were mixed type non-seminomatous germ cell tumors.
Importantly, the number of complicated anterior mediastinum surgeries performed with VATS for TETs [TNM staging II–III according to the Union for International Cancer Control (UICC) 8th edition] continued to increase in 2019 (Figure 17). In addition, the number of complicated anterior mediastinum surgeries by open procedures for TETs (UICC 8th TNM staging II–IV) decreased when compared to last year, with open procedures being performed in 108 patients in 2019 (35.0% of all open surgeries) (Figure 18).
Overall, only 21 (1.93%) patients suffered major post-operative complications, with 2 (0.18%) patients succumbing during the postoperative period. With the help of ERAS, the post-operative LOS decreased from 5.8 days in 2018 to 4.95 days in 2019. These results are extremely promising, especially in simple and straightforward minimally invasive mediastinal surgeries. No severe complications or readmissions were needed for ERAS-treated patients in 2019.
The mediastinal surgery division of Shanghai Chest Hospital has continually pushed the application of MIS in the surgical treatment of mediastinal diseases. This is evidenced by the high percentage of RATS and VATS performed for locally invasive lesions as well as for early-stage tumors, and by the implementation of novel techniques such as subxiphoid VATS, uniportal VATS, bilateral VATS, and others. Meanwhile, complex mediastinal surgeries for extensive resections of locally advanced diseases have not been compromised. Intentional and salvage surgeries after neoadjuvant therapies, resection and reconstruction of great vessels, and re-resection and pleurectomy for recurrent diseases were routinely carried out on a daily base, representing our unrelenting effort in helping those patients with refractory diseases.
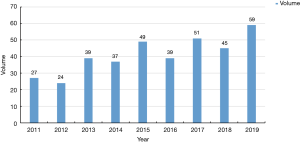
Tracheal surgeries
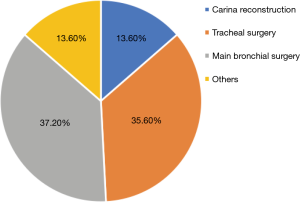
As one of the leading centers in tracheal surgery in China, the Shanghai Chest Hospital completed 59 tracheal procedures in 2019, representing a 31.1% increase from 2018 (Figure 19). These included 21 cases (37.2%) of tracheal surgeries, 22 cases (37.2%) of main bronchial surgeries, and 9 cases (13.6) of carina resection and reconstruction (Figure 20). The average LOS was 10.5±8.2 days, the major postoperative complication rate was 32.2%, and the rate of in-hospital mortality was 1.7%.
Improvements made in complicated surgery for tracheal and bronchial diseases by our tracheal team in the year of 2019 included laryngotracheal reconstruction, VATS thoracic tracheal reconstruction under non-intubated anesthesia, VATS carina reconstruction, and others. More patients are thus expected to benefit from these advances in surgical techniques.
Lung transplantations
In 2019, 9 patients registered on the waiting list to receive lung transplantation, including 3 cases of sequential double-lung transplantation, 3 cases of left single-lung transplantation, and 3 cases of right single-lung transplantation. More efforts are needed to find donors, while research in improving the quality of donor organs is also underway.
Discussion
The thoracic surgery team of Shanghai Chest Hospital has been publishing our annual reports to the public since 2017. Summarized in these reports are the major achievements made in past year, in addition to the increasing need for services at the Shanghai Chest Hospital. As one of the largest thoracic surgery centers in China, the annual volume of thoracic surgery at the Shanghai Chest Hospital has exceeded 10,000 cases for 4 consecutive years and reached a new high of more than 17,000 in 2019. Minimally invasive thoracic surgery is playing an increasingly important role in our daily practice, with nearly 90% of all procedures being completed by MIS approaches. This is in line with the rapid increase in the screening and early detection of lesions, and the rising demand for faster recovery and better quality of life from our patients. Notably, the volume of RATS has also been steadily increasing over the past years, making our hospital one the largest RATS centers in the world.
Being one of the most historic cardiothoracic centers in China, the Shanghai Chest Hospital has long been known for its ability and experience in the management of complex, difficult, and refractory chest diseases. In recent years, one of our focal areas has been the use of MIS for patients with locally advanced diseases and those needing complex procedures, including various reconstructions after resection. We are happy to see that our attempts in MIS after neoadjuvant therapies or for those patients with locally advanced diseases have been successful. In the management of lung cancer, esophageal cancer, mediastinal tumors, and tracheal diseases, similar or superior outcomes to open surgery were observed in major postoperative complication rates, in-hospital mortality rates, and rates of unplanned reoperation or readmission to ICU, while oncological results such as complete resection or lymph node dissection were not compromised. These encouraging results suggest that we have improved our service to patients by providing them state-of-the-art healthcare. We truly hope that this year’s annual report from the thoracic surgery team of Shanghai Chest Hospital can again serve as a useful reference for our colleagues. We will continue to spare no effort in providing high-level medical care and dedicated service.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the editorial office, Shanghai Chest. The article did not undergo external peer review.
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/shc-2021-01). QL serves as an unpaid Associate Editors-in-Chief of Shanghai Chest. WF serves as an unpaid Executive Editor-in-Chief of Shanghai Chest. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
(English Language Editor: J. Gray)
Cite this article as: Wang Y, Gu Z, Yao F, Mao T, Wang R, Sun Y, Li Z, Yang J, Tan Q, Luo Q, Fang W. Annual report of thoracic surgery service at Shanghai Chest Hospital in 2019. Shanghai Chest 2021;5:13.