
The role of haptic feedback in video-assisted thoracic surgery simulation training
Nowadays, minimally invasive techniques have become the standard for patients needing thoracic surgical intervention, especially for early stage lung cancer radical treatment. The first video-assisted thoracic surgery (VATS) lobectomy for cancer was performed in 1991 (1), and its use has significantly increased until it has become the standard according to international guidelines for diagnosis and treatment of lung cancer (2,3).
The VATS approach, either by single or multiple ports, has proven to have several advantages compared with thoracotomy, including less postoperative pain and complications, prompt postoperative recovery and consequently shorter length of hospital stay. Moreover, in oncologic patients VATS is related with an increased tolerance to adjuvant chemotherapy and better quality of life (4).
However, it is important to emphasize that VATS surgery can be challenging and acquiring the skills needed to become competent, such as depth perception and video-hand-eye coordination, requires a long learning curve with an extensive training to learn moving instruments within the operative field safely and effectively. Indeed, for major thoracic procedures as lobectomy, it has been estimated that around 50 VATS procedures are needed to overcome the learning curve (5), over a recommended training period of up to 1 year (6). Experiencing directly at the operating room can be inefficient, time-consuming, and it may cause safety concerns for patients (7).
Surgical practice on animals and/or human cadavers, which is currently in use in specialized centres, has been facing increasing logistic, ethical and financial obstacles in the most advanced nations (8,9).
Thus, new laboratory training models, that can provide a similar situation during surgery in a similar human anatomy, have been introduced in general surgery first and, recently, in thoracic surgery. These tools, by simulating tactile and visual sensations, allow the virtual execution and the repetition of surgical manoeuvres until the trainee reaches satisfactory results. So, development of surgical simulators should be considered essential to improve trainees’ capacities.
The “simulation”, as defined by Desender, is a “technique to replace or amplify a real-patience experience with guided experience, artificially contrived, that evokes or replicates substantial aspects of the real world in a fully interactive manner” (10). More in detail, a medical simulator is a physical object that reproduces a real clinical scenario, without the presence of an actual patient (11).
Simulation training has progressed from simple bench-top exercises to complex full procedural training on high fidelity immersive virtual reality (VR) simulators. In general, simulators are classified as low- and high-fidelity, but both have been proved to be useful in helping trainees to acquire basic surgical skills. Low-fidelity simulators, such as box trainers (Figure 1A), help trainees to acquire psychomotor skills, and in general, are cheap and require the use of real instruments; however, their use makes the record of any performance measurements arduous (12).
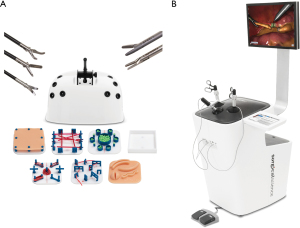
VR platform is a high-fidelity simulator (Figure 1B), that uses a computer and physical interfaces representing surgical instruments and ports to simulate a virtual surgical environment with which the trainee can interact. Traditional box trainers are low-fidelity simulators, that lack of any form of objective assessment and which can be considered unrealistic in presented exercises. However, despite most VR simulators do offer several advantages such as constant availability of training, immediate and quantitative feedback, and catered training conditions, they lack haptic feedback.
“Haptics” is generally defined as the process of recognizing objects through touch, and, in medicine, a science concerned with the sense of touch; in surgery haptics may be referred to the science of applying tactile sensation and control to the interaction with the environment (13). Despite the haptic sensations are weaker in thoracoscopy compared to open surgery, the surgeon can still perceive haptic sensations through the instruments as they touch the trocars, the thoracic wall, the tissues, and any other physical element within the surgical environment (13).
Video-assisted surgery is characterized by a brain adaptation to the predominant use of the visual versus the tactile cues, and the tactile sensation perceived by the operator is an unequal combination of multiple forces. On the contrary, in open surgery haptic feedback is a direct measure of the interaction forces between hands or surgical instruments and tissues. These are represented by the interaction of the instrument with the intra-thoracic organs, the friction between surgical tool and trocar port, the resistance of the thoracic wall during the instrument tilting movements, the effects of operator on the instrument, and the effect of activation of the pincer mechanism of surgical instrument (14).
The introduction of haptic feedback in training systems had been demonstrated to improve robot-assisted knot-tying with fine suture (15), reduce overall forces applied and number of accidental incursions into sensitive structures, shorten task completion time and make suturing straighter (16).
Trainer box based on a complete porcine heart-lung complex has demonstrated that the natural haptic sensation is maintained despite differences with human anatomy. In contrast, VR simulators lack natural haptic feedback as well as any operational step outside the thorax, so the transfer of VR training experience to the operating room is challenging (9).
Some minimally invasive VR simulators have been developed with simulated force feedback, adding approximately $20,000 to $30,000 to the price (17,18).
In the literature, no studies have been focused on the benefits of haptic systems for VATS training, but it is reported that haptic feedback is very important in laparoscopic simulation and can shorten the first part of the performance curve. Thereby, the benefits of a shorter time to the first performance plateau should be balanced with the cost of implementing haptic feedback in training simulators (19).
Because no VR simulator for VATS training was commercially available in early 2010, a VR simulator was compared to the box trainer to investigate whether training on a laparoscopic simulator enables trainees to perform a thoracoscopic lobectomy (20). Results showed that the training on a laparoscopic VR simulator in a nephrectomy (task chosen because similar to the thoracoscopic lobectomy that was not included in the VR simulator software) did not have any advantage over the box training in any of the measured points. The authors believed that this result was due to the lack of haptic feedback in the VR simulator (20).
Tai and collaborators recently reported that the innovative augmented reality simulator has more realistic surgical training environments compared to VR training systems, with a visuo-haptic experience closer to that of human factors engineering, and a more natural immersive interactive perception, but the haptic perception was lower compared to the box trainer simulator (21).
The benefits of haptic feedback in the VATS lobectomy simulation are still unclear and further studies are required to better understand its role in thoracic surgery training. In theory, after basic surgical skills development, trainees and junior thoracic surgeons need to improve video-assisted knot-tying, especially in the management of urgent situation to obtain control of bleeding with effective suture.
Moreover, besides the identification of the most suitable simulator, it is fundamental to develop an appropriate thoracic surgical training program including the use of simulators and to test their utility in this context.
In addition, since few data are available about how the haptic feedback influences skills acquisition and transfer to the operation room, future research should focus on how VR simulators could implement haptic feedback to best enhance VATS skills training and on improving quality and haptic feedback type to be incorporated into the latest generation VR simulators.
In conclusion, technological advances on haptic devices, together with further studies focused on haptic feedback, will be useful to develop efficient and effective training curricula and to establish the value of simulators with haptic feedback in training and assessing thoracic surgical skills.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the editorial office, Shanghai Chest. The article did not undergo external peer review.
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://shc.amegroups.com/article/view/10.21037/shc-22-18/coif). AI serves as an unpaid editorial board member of Shanghai Chest. The other authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Roviaro GC, Varoli F, Vergani C, et al. State of the art in thoracospic surgery: a personal experience of 2000 videothoracoscopic procedures and an overview of the literature. Surg Endosc 2002;16:881-92. [Crossref] [PubMed]
- Postmus PE, Kerr KM, Oudkerk M, et al. Early and locally advanced non-small-cell lung cancer (NSCLC): ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol 2017;28:iv1-21. [Crossref] [PubMed]
- Ettinger DS, Wood DE, Aisner DL, et al. NCCN Guidelines Insights: Non-Small Cell Lung Cancer, Version 2.2021. J Natl Compr Canc Netw 2021;19:254-66. [Crossref] [PubMed]
- Falcoz PE, Puyraveau M, Thomas PA, et al. Video-assisted thoracoscopic surgery versus open lobectomy for primary non-small-cell lung cancer: a propensity-matched analysis of outcome from the European Society of Thoracic Surgeon database. Eur J Cardiothorac Surg 2016;49:602-9. [Crossref] [PubMed]
- McKenna RJ Jr. Complications and learning curves for video-assisted thoracic surgery lobectomy. Thorac Surg Clin 2008;18:275-80. [Crossref] [PubMed]
- Petersen RH, Hansen HJ. Learning thoracoscopic lobectomy. Eur J Cardiothorac Surg 2010;37:516-20. [Crossref] [PubMed]
- Gallagher AG, Ritter EM, Champion H, et al. Virtual reality simulation for the operating room: proficiency-based training as a paradigm shift in surgical skills training. Ann Surg 2005;241:364-72. [Crossref] [PubMed]
- Dell'Amore A, Boscolo-Berto R, Schiavon M, et al. Human corpse model for video-assisted thoracoscopic lobectomy simulation and training. Interact Cardiovasc Thorac Surg 2020;31:632-7. [Crossref] [PubMed]
- Domhan L, Johannink J, Miller J, et al. TuThor: an innovative new training model for video-assisted thoracic surgery. Interact Cardiovasc Thorac Surg 2020;30:477-82. [Crossref] [PubMed]
- Desender LM, Van Herzeele I, Aggarwal R, et al. Training with simulation versus operative room attendance. J Cardiovasc Surg (Torino) 2011;52:17-37. [PubMed]
- Abou-Elhamd KE, Al-Sultan AI, Rashad UM. Simulation in ENT medical education. J Laryngol Otol 2010;124:237-41. [Crossref] [PubMed]
- Våpenstad C, Hofstad EF, Langø T, et al. Perceiving haptic feedback in virtual reality simulators. Surg Endosc 2013;27:2391-7. [Crossref] [PubMed]
- Bholat OS, Haluck RS, Murray WB, et al. Tactile feedback is present during minimally invasive surgery. J Am Coll Surg 1999;189:349-55. [Crossref] [PubMed]
- Picod G, Jambon AC, Vinatier D, et al. What can the operator actually feel when performing a laparoscopy? Surg Endosc 2005;19:95-100. [Crossref] [PubMed]
- Kitagawa M, Dokko D, Okamura AM, et al. Effect of sensory substitution on suture-manipulation forces for robotic surgical systems. J Thorac Cardiovasc Surg 2005;129:151-8. [Crossref] [PubMed]
- Moody L, Baber C, Arvanitis TN. Objective surgical performance evaluation based on haptic feedback. Stud Health Technol Inform 2002;85:304-10. [PubMed]
- Salkini MW, Doarn CR, Kiehl N, et al. The role of haptic feedback in laparoscopic training using the LapMentor II. J Endourol 2010;24:99-102. [Crossref] [PubMed]
- Panait L, Akkary E, Bell RL, et al. The role of haptic feedback in laparoscopic simulation training. J Surg Res 2009;156:312-6. [Crossref] [PubMed]
- Zhou M, Tse S, Derevianko A, et al. Effect of haptic feedback in laparoscopic surgery skill acquisition. Surg Endosc 2012;26:1128-34. [Crossref] [PubMed]
- Jensen K, Ringsted C, Hansen HJ, et al. Simulation-based training for thoracoscopic lobectomy: a randomized controlled trial: virtual-reality versus black-box simulation. Surg Endosc 2014;28:1821-9. [Crossref] [PubMed]
- Tai Y, Shi J, Pan J, et al. Augmented reality-based visual-haptic modeling for thoracoscopic surgery training systems. Virtual Reality & Intelligent Hardware 2021;3:274-86. [Crossref]
Cite this article as: Imperatori A, Grossi S, Cattoni M, Rotolo N. The role of haptic feedback in video-assisted thoracic surgery simulation training. Shanghai Chest 2022;6:11.


