
Stapler stuck to the lung tissue during thoracoscopic lobectomy: a case report
Introduction
Staplers play a crucial role in video-assisted thoracoscopic surgery lobectomy (VATSL), simplifying the procedure, and reducing surgeon skill-driven variability, but their malfunction may be associated with post-operative morbidity and/or mortality (1-4). Herein, we reported a case of stapler trouble during VATSL of left lower lobe (LLL) that was successfully recovered by the use of additional stapler. We present the following case in accordance with the CARE reporting checklist (available at https://shc.amegroups.com/article/view/10.21037/shc-21-32/rc).
Case presentation
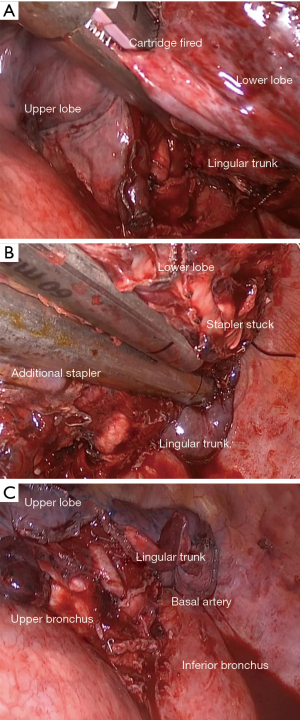
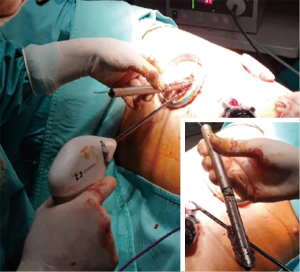
A 51-year-old smoker man underwent VATSL using a standard three-port anterior approach for management of early-stage adenocarcinoma (T1bN0M0) of the LLL. He was asymptomatic, and his past medical history was unremarkable. A fissureless approach was performed and the interlobar fissure was divided at last using a stapler with 60 mm purple (3.5 mm) cartridge (Endo GIA Tri-stapleTM Technology, Medtronic, Minneapolis, USA). Before using the stapler, both the scrub nurse and surgeon ensured that the cartridge was correctly inserted into the stapling device with no residual staples left from previous firings. According to the manufacturer’s instructions, the jaws were closed on the lung tissue without forcing them, the green safety button was pushed, the handle was gently squeezed until the cartridge was fully fired. The black retraction was then pulled back, but the jaws did not open, remaining stuck to the lung tissue (Figure 1A). All secondary maneuvers recommended from the manufacturer for opening the jaws were performed, but without success. An additional stapler with 60 mm purple (3.5 mm) cartridge (Echelon Powered Stapler, Ethicon, Inc., Cincinnati, OH, USA) was inserted through the anterior incision, and divided the tissue between the stuck stapler and the pulmonary artery (Figure 1B,1C). The tissue with the locked stapler was divided from the specimen using energy device (LigasureTM Technology, Medtronic, Minneapolis, USA, and taken out of the patient through the anterior incision (Figure 2). The specimen was then inserted within the endo-bag and retrieved through the anterior incision in a standard manner. Extended lymphadenectomy completed the procedure, and intraoperative sealing test revealed no air leakage. Video 1 summarized the procedure. The operation time and intraoperative blood loss were 195 minutes and 150 mL, respectively. The postoperative course was unremarkable, and patient was discharged five days later. The actual follow-up showed no sign of recurrence.
All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Discussion
Staplers have been used in thoracic surgery for over 20 years, and have an essential role for the widespread application of VATSL. However, in the last years an increased number of adverse events (AEs) associated with staplers have been reported. From January 2011 to March 2018, the Food and Drug Administration received more than 11,500 reports including 366 deaths, and over 9,000 serious injuries (1). The AEs mainly occurred during lung surgery, and included massive bleeding, air leakage and oozing due to misfiring when staplers were used for vascular (2) and bronchial closure (3) and/or for division of the parenchyma (4). However, stapler stuck on lung tissue, as in the present, has not been reported before.
To deal this trouble, we used another stapler to restaple along the locked stapler. The tissue with the locked stapler was divided from the specimen using LigasureTM, and taken out of the patient. The specimen was then inserted into the endo-bag and retrieved. This strategy was relatively easy since all vessels and bronchus were already closed, and there was enough space left adjacent to the bronchus and vessels. In case of no room to place an additional stapler, the locked stapler may be dissected from the remaining lobe using energy device, despite this procedure is associated with an increased risk of air-leaks and/or oozing. However, if the stuck stapler is close to the pulmonary artery, there is the risk of vascular injury during dissection. To deal this situation, we suggest to clamp the main pulmonary artery first, and then to start dissection. This strategy prevents catastrophic bleeding and facilitates the repair of pulmonary artery via a running suture in case of injury. The plastic of pulmonary artery preserves the vascularization of the remaining lobe and avoids performing pneumonectomy. The decision whether to continue with VATS or to convert to thoracotomy depends on ability and experience of surgeon with VATS. The reconstruction of pulmonary artery by suture may be more complicated in VATS due to relatively limited space and operative angle, but several studies reported the feasibility and safety of the VATS to perform vascular plastic procedures in expert hands (5-8).
Incorrected loading of cartridge to staple gun, stapler-tissue thickness mismatch, inadequate position of stapler tip, excessive traction on the tissue, and firing over a previous staple line were the main causes of stapling failure resulting from improper use (9). However, none of these events occurred in our case. (I) The stapling cartridge was well loaded, as the staple gun correctly fired. (II) The cartridge size was appropriate for the tissue thickness as no resistance was felt during grasping tissue and firing, and the grasp motion was not stopped before completion of firing. (III) There was no firing over a previous staple line as it was the first stapling. (IV) Our patient did not have underlying lung diseases as emphysema or fibrosis, affecting the stapler functions. (V) We were unable to pull the knife back manually when it was taken out of the patient. Endo GIA did not have a manual override lever to retract the knife and release the jaws. This AE was reported to our hospital, and the stuck cartridge was returned to manufacture for evaluation, but we did not receive any report from manufacture to explain this problem. Thus, we did not have any proof to clarify whether this AE was due to stapler malfunction or our improper use.
Despite all, we believe that our strategy may be useful for surgeons to deal an unpredicted similar situation that may occur either for stapler malfunction or for improper use. Many surgeons may consider the same recovery to complete the planned resection without further consequences.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at https://shc.amegroups.com/article/view/10.21037/shc-21-32/rc
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://shc.amegroups.com/article/view/10.21037/shc-21-32/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Available online: https://www.fda.gov/medical-devices/letters-health-care-providers/safe-use-surgical-staplers-and-staples-letter-health-care-providers
- Craig SR, Walker WS. Potential complications of vascular stapling in thoracoscopic pulmonary resection. Ann Thorac Surg 1995;59:736-7; discussion 737-8. [Crossref] [PubMed]
- Yano M, Yokoi K, Numanami H, et al. Complications of bronchial stapling in thoracic surgery. World J Surg 2014;38:341-6. [Crossref] [PubMed]
- Yano M, Iwata H, Hashizume M, et al. Adverse events of lung tissue stapling in thoracic surgery. Ann Thorac Cardiovasc Surg 2014;20:370-7. [Crossref] [PubMed]
- Liu C, Yang Z, Guo C, et al. Lobectomy with pulmonary artery angioplasty for lung cancer using video-assisted thoracic surgery versus open thoracotomy: a retrospective propensity matched analysis. Transl Lung Cancer Res 2021;10:3943-56. [Crossref] [PubMed]
- Huang J, Li J, Qiu Y, et al. Thoracoscopic double sleeve lobectomy in 13 patients: a series report from multi-centers. J Thorac Dis 2015;7:834-42. [PubMed]
- Liu L, Mei J, Pu Q, et al. Thoracoscopic bronchovascular double sleeve lobectomy for non-small-cell lung cancer. Eur J Cardiothorac Surg 2014;46:493-5. [Crossref] [PubMed]
- Fiorelli A, Forte S, Natale G, et al. Handling benign interlobar lymphadenopathy during thoracoscopic lobectomy. Thorac Cancer 2021;12:1489-92. [Crossref] [PubMed]
- Gossot D, Merlusca G, Tudor A, et al. Pitfalls related to the use of endostaplers during video-assisted thoracic surgery. Surg Endosc 2009;23:189-92. [Crossref] [PubMed]
Cite this article as: Fiorelli A, Natale G, Ferraro F, Fiorito R, Santini M. Stapler stuck to the lung tissue during thoracoscopic lobectomy: a case report. Shanghai Chest 2022;6:14.


