
Endotracheal tube for relocating dislocated airway stent: a case report
Introduction
Malignant central airway stenosis (CAO) is a life-threatening condition which may lead to emergency intubation and mechanical ventilation to manage severe respiratory failure. Airway stenting may facilitate extubation, and preserve stable airway for further cancer specific treatments (1-4). Herein, we reported an unconventional life-saving strategy using endotracheal tube (ETT) to relocate a displaced airway stent in a patient with critical CAO. We present the following case in accordance with the CARE reporting checklist (available at https://shc.amegroups.com/article/view/10.21037/shc-22-6/rc).
Case presentation
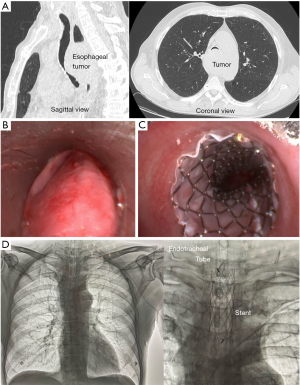
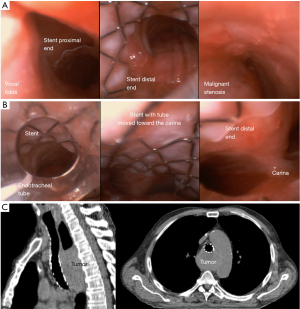
A 69-year-old man with critical extrinsic CAO due to advanced esophageal cancer, starting in the mid-trachea and extending to the carina (diameter 5 mm; length 55 mm; Figure 1A,1B) was referred to our hospital. Due to acute respiratory failure, he underwent an emergent intubation and mechanical ventilation. Airway stenting was identified by multidisciplinary team as the best strategy to wean the patient from mechanical ventilation and preserve stable airway for further cancer specific treatments. The procedure was performed in operating room. The ETT was removed, a 14 mm rigid bronchoscope was inserted in the trachea and a covered Self-Expandable Metallic Stent (SEMS) (18 mm × 60 mm Silmet; Novatech, La Ciotat, France) was placed to obtain the airway patency (Figure 1C). Patient was not extubated, but he moved to Intensive Care Unit (ICU) with a 6.0 mm ETT in situ. The day after, a chest X-Ray confirmed the prompt position of the stent and the airway patency (Figure 1D). The patient was successfully weaning from ventilator, and he was extubated without using the fiber bronchoscope, but soon after extubation, he developed severe breathing difficulty. An emergent fiber bronchoscope showed that the stent was dislocated above the stenosis (Figure 2A). The operating room was not available for an emergent rigid bronchoscope. Thus, a 7.5 mm ETT loaded on a fiber-bronchoscope was placed within the stent; the balloon was inflated, and under direct vision the ETT with the stent was gently moved toward the carina, until the stent forced the stenosis and its distal end was relocated above the carina (Figure 2B). The balloon was then deflated, and ETT removed. Dyspnea disappeared and chest CT scan confirmed the prompt stent position and the stable airway patency (Figure 2C). The procedure was summarized in Video 1. The patient was discharged 5 days later, and underwent chemoradiotherapy with tumor response. Thus, the stent was removed three months later.
All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Discussion
CAO is a life-threatening condition which can cause severe respiratory failure, leading to urgent intubation. However, mechanical ventilation remains a temporary treatment, and further interventions are necessary for permanent relief of symptoms. Several studies reported that airway stenting helped in weaning from mechanical ventilation patients with benign (1) and/or malignant CAO (2-4). Yet, a stable airway facilitated the administration of specific cancer therapies, such as chemo and radiation therapy, with potential survival benefits especially in naïve patients (5).
However, the complications of incorrect airway manipulation in patients with airway stent in situ may be catastrophic, as in this case. The blind extubation was the reason for the dislodgement of the stent, resulting in life-threatening respiratory failure. There was a high possibility that the tip of the tracheal tube was caught in the tracheal stent and dislocated the stent during extubation.
To face this complication, the first choice was an emergent rigid bronchoscopy, but the operating room was not readily available in this case. Thus, we used a life-saving method, not been reported before, to relocate the stent using a cuffed ETT and fiber bronchoscopy. Stent migration, stent fracture, stent breakage, and mucosal tear (6) were all potential complications related to our strategy. Thus, this strategy should be performed under direct vision to ensure the position of ETT into the stent, to prevent airway lesions during the stent mobilization, and assure the prompt relocation of the stent. In case of failure, the ETT assured the ventilation of the patient till the operating room was available for rigid bronchoscopy.
The main lesson to be learned from this case was to not extubate a patient with a high-risk airway unless physicians are prepared to deal with the potential complications. This was an elective extubation and could have been deferred until back-up rigid bronchoscopy was available. Yet, it was mandatory to observe the position of the stent when removing the ETT to prevent its dislocation. Second, our method was not the first choice, but it should be considered as a life-saving treatment to perform in emergent situation when all conventional treatments were not readily available. Fortunately, this method worked successfully in this case. It was because the airway stent used was a covered type, thus there was less resistance between the stent and the tracheal mucosa. However, there is no guarantee that it will be valid in another case.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at https://shc.amegroups.com/article/view/10.21037/shc-22-6/rc
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://shc.amegroups.com/article/view/10.21037/shc-22-6/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Noppen M, Stratakos G, Amjadi K, et al. Stenting allows weaning and extubation in ventilator- or tracheostomy dependency secondary to benign airway disease. Respir Med 2007;101:139-45. [Crossref] [PubMed]
- Oki M, Saka H, Hori K. Airway stenting in patients requiring intubation due to malignant airway stenosis: a 10-year experience. J Thorac Dis 2017;9:3154-60. [Crossref] [PubMed]
- Davis N, Madden BP, Sheth A, et al. Airway management of patients with tracheobronchial stents. Br J Anaesth 2006;96:132-5. [Crossref] [PubMed]
- Chen Y, Zhou ZQ, Feng JX, et al. Hybrid stenting with silicone Y stents and metallic stents in the management of severe malignant airway stenosis and fistulas. Transl Lung Cancer Res 2021;10:2218-28. [Crossref] [PubMed]
- Paganin F, Schouler L, Cuissard L, et al. Airway and esophageal stenting in patients with advanced esophageal cancer and pulmonary involvement. PLoS One 2008;3:e3101. [Crossref] [PubMed]
- Chang HY, Man KM, Liao KH, et al. Rescue patient from tracheal obstruction by dislocated bronchial stent during tracheostomy surgery with readily available tools: A case report. Medicine (Baltimore) 2017;96:e7841. [Crossref] [PubMed]
Cite this article as: Fiorelli A, Messina G, Fiorito R, Martone M, Ferraro F, Santini M. Endotracheal tube for relocating dislocated airway stent: a case report. Shanghai Chest 2022;6:13.


