A case report of uniportal video-assisted thoracic surgery left lower lobe wedge resection: guided by negative fluorography based on pre-block of watershed pulmonary arteries
Introduction
More and more early lung cancers with dominant ground glass opacity (GGO) were detected by increasing computed tomography (CT) screening. The results of JCOG0804 (WJOG4507L) and JCOG0802 (WJOG4607L) have suggested that sub-lobectomy (wedge resection and segmentectomy) was recommended to the surgical treatment of GGO-predominant peripheral pulmonary nodules less than 2 cm (1,2), as the postoperative 5-year survival rate of these patients was almost 100% (3).
Accurate intraoperative localization of the nodules was the key point of oncological safety and parenchyma-sparing strategy of lung resection (4). Percutaneous CT-guided hook-wire was the most widely used method to locate pulmonary nodules, however, it was associated with 33.7% of pneumothorax and 22.5% mild parenchymal hemorrhage according to a recent study (5). In recent years, surgeons were continuously seeking innovative approaches to cover the limitations of CT-guided hook-wire, such as three-dimensional (3D) printing (6), newly designed hook-wire (7), electromagnetic navigation combined fluorescence thoracoscope (8). In this article, we introduced an innovative approach that based on topographic anatomy of pulmonary segments, with the aim to develop a safe and flexible alternative method for nodules localization in video-assisted thoracic surgery (VATS). We present the following article in accordance with the CARE reporting checklist (available at https://shc.amegroups.com/article/view/10.21037/shc-22-3/rc).
Case presentation
The patient was a 46-year-old lady, non-smoker, a small ground-glass nodule (GGN) in her left lower lobe (about 0.4 cm in diameter) was detected by CT scan two years ago. Recent CT scan revealed that the nodule was 0.7 cm in diameter and presented as mix-GGN with 3D substructure measurement.
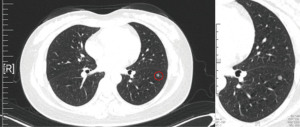
The CT images demonstrated that the enlarged nodule was in the anterior basal segment of left lower lobe (LS8), but close to the superior segment of left lower lobe (LS6), as showed in Figure 1, the consolidation-to-tumor ratio (C/T ratio) of the nodule was about 24%.
No abnormal was found by echocardiography and lung function [forced expiratory volume in 1 s (FEV1) =2.46 L; FEV1/forced vital capacity (FVC) =84%].Regarding the size, C/T ratio and location of the nodule, wedge resection with safe margin would be an appropriate approach. The CT images revealed the nodule was not close to visceral pleura, indicating the nodule would be invisible and impalpable during operation.
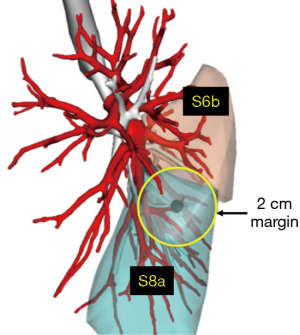
3D reconstruction based on the CT image was made by a software (Vitaworks, China) (Figure 2). the 2 cm margin involved the subsegment a of LS8 (LS8a) and subsegment b of LS6 (LS6b). So, the nodule would be definite resected with safe margin by wedge resection along the border of LS8a and LS6b.
A double lumen endotracheal tube was applied for intubation. The patient was placed in the lateral decubitus position, intercostal nerve blocks were utilized before operation. One-lung ventilation was maintained during the whole operation. The patient was cared according to the enhanced recovery after surgery (ERAS) protocols for anesthesia management.
A 4 cm incision for uniportal VATS was made in the 5th intercostal space at anterior axillary line. A 10-mm 30° fluorescence thoracoscope was fixed on the posterior side of the incision during the operation.
The principle of fluorescence image: after intravenous injection of indocyanine green (ICG) fluorescence, ICG binds to plasma protein. If near infrared light (805 nm) is absorbed by the ICG in plasma, it will emit a fluorescence wavelength of 830 nm that can be seen using infrared thoracoscopy.
The steps of the operation were shown below (Video 1):
- Dissection of oblique fissure to exposure the pulmonary arteries of left lower lobe.
- Dividing the branches of arteries of LS8 and LS6.
- Identifying the artery of LS8a (A8a) and LS6b (A6b) according to the 3D reconstruction.
- Pre-block the A8a and A6b by clamps.
- 25 mg ICG was injected via peripheral vein.
- The fluorescence was invisible in the watershed of A8a and A6b under the fluorescence mode.
- Making markers along the border of fluorescence which was also the border of S8a and S6b.
- Wedge resection along the markers by using staplers.
- After irrigation, a 20-Fr chest tube was placed through the incision.
The patient underwent a routine postoperative X-ray on the operation day. A modified ERAS protocol was applied, including early ambulation, pain control, exercise rehabilitation. The patient discharged at day 3 after removing chest tube. The pathological diagnosis was adenocarcinoma in situ.
All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Discussion
Localization is critical step of sub-lobectomy for pulmonary nodules. For nodules that are not suitable for CT-guided localization or are in the middle zone of lung, segmentectomy or combined sub-segmentectomy, in a sense, is another anatomic localization approach for nodules that meet the criteria for wedge resection.
During segmentectomy, inflation-deflation method is commonly used to display the inter-segment plane, which is based on the physiological principle of alveolar gas exchange. However, this procedure is always time consuming, but in this case, the fluorescence emerged in seconds after the injection of ICG without considering situations in that the inter-segment plane might not be distinct, such as cases with chronic obstructive pulmonary disease or extensive adhesion.
In this case, we only exposed and pre-blocked the target segmental pulmonary arteries without dividing the segmental bronchus and veins, the procedure was much more simplified than a standard segmentectomy. The safety and feasibility of this method were reported by a similar pilot study (4). However, this method for localization can only be used in selected cases in that the target arteries are easy to be exposed. Furthermore, if the fluorescent devices are not available, traditional inflation-deflation method is also an alternative. The key for the pre-block of watershed pulmonary arteries is to accurately identify the target arteries preoperatively. A 3D reconstruction can provide a more visualized mode for determining the spatial stereoscopic relationship between nodules and target arteries than CT images.
Conclusions
Negative fluorography based on pre-block of watershed pulmonary arteries is an innovative localization method for selected peripheral pulmonary nodules with the advantages of time-saving and precise resection.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at https://shc.amegroups.com/article/view/10.21037/shc-22-3/rc
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://shc.amegroups.com/article/view/10.21037/shc-22-3/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Suzuki K, Watanabe SI, Wakabayashi M, et al. A single-arm study of sublobar resection for ground-glass opacity dominant peripheral lung cancer. J Thorac Cardiovasc Surg 2022;163:289-301.e2. [Crossref] [PubMed]
- Suzuki K, Saji H, Aokage K, et al. Comparison of pulmonary segmentectomy and lobectomy: Safety results of a randomized trial. J Thorac Cardiovasc Surg 2019;158:895-907. [Crossref] [PubMed]
- Asamura H, Hishida T, Suzuki K, et al. Radiographically determined noninvasive adenocarcinoma of the lung: survival outcomes of Japan Clinical Oncology Group 0201. J Thorac Cardiovasc Surg 2013;146:24-30. [Crossref] [PubMed]
- Chu XP, Chen ZH, Lin SM, et al. Watershed analysis of the target pulmonary artery for real-time localization of non-palpable pulmonary nodules. Transl Lung Cancer Res 2021;10:1711-9. [Crossref] [PubMed]
- Zhang H, Li Y, Yimin N, et al. CT-guided hook-wire localization of malignant pulmonary nodules for video assisted thoracoscopic surgery. J Cardiothorac Surg 2020;15:307. [Crossref] [PubMed]
- Zhang L, Li M, Li Z, et al. Three-dimensional printing of navigational template in localization of pulmonary nodule: A pilot study. J Thorac Cardiovasc Surg 2017;154:2113-2119.e7. [Crossref] [PubMed]
- Fan L, Yang H, Yu L, et al. Multicenter, prospective, observational study of a novel technique for preoperative pulmonary nodule localization. J Thorac Cardiovasc Surg 2020;160:532-539.e2. [Crossref] [PubMed]
- Anayama T, Qiu J, Chan H, et al. Localization of pulmonary nodules using navigation bronchoscope and a near-infrared fluorescence thoracoscope. Ann Thorac Surg 2015;99:224-30. [Crossref] [PubMed]
Cite this article as: Han D, Yang X, Zhu L, Li H. A case report of uniportal video-assisted thoracic surgery left lower lobe wedge resection: guided by negative fluorography based on pre-block of watershed pulmonary arteries. Shanghai Chest 2022;6:28.