Simultaneous minimally invasive uniportal atrial septal defect repair and pulmonary lobectomy: a case report
Introduction
Combined surgical pathology in the same patient is common entity. When present, these combinations open an opportunity for simultaneous surgical intervention. Authors previously reported a combination of lung cancer with other processes (1). However, combination of non-oncological respiratory and cardiac conditions may also occur, calling for simultaneous treatment. We describe the first case of successful simultaneous thoracoscopic uniportal procedure with cardiopulmonary bypass (CPB) in the treatment of multiple congenital heart defects and pulmonary complications of bronchiectasis. We present the following case in accordance with the CARE reporting checklist (available at https://shc.amegroups.com/article/view/10.21037/shc-22-36/rc).
Case presentation
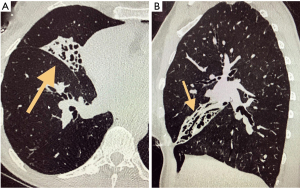
A 49-year-old male with past medical history significant for bronchiectasis, complicated by fibrosis of the middle lobe, presented with dyspnea, recurrent hemoptysis, and nonproductive cough. Conservative management was ineffective. The patient noted a progressive decrease in physical endurance and deterioration of the quality of life. A computerized tomography (CT) scan of the chest showed fibroatelectasis of the right middle lobe (RML) (Figure 1). Echocardiography revealed a large atrial septal defect (ASD), biventricular enlargement with severe mitral and tricuspid regurgitation, mitral prolapse and moderate pulmonary artery hypertension. After multidisciplinary evaluation, simultaneous procedure was proposed with thoracoscopic uniportal cardiac intervention and lobectomy. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
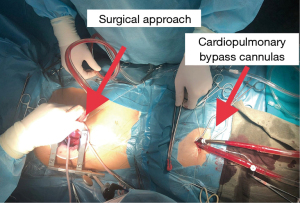
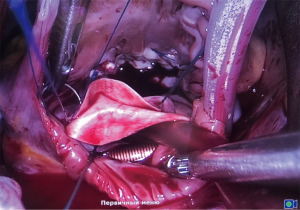
Single 4 cm thoracoport was placed in the right 4th intercostal space at the mid-axillary line. The surgeon and assistant were positioned in the back. Simultaneously, femoral artery and vein cannulation was performed for the CPB (Figure 2). Position of the venous cannula was confirmed with transesophageal echocardiography. Cross-clamping of the aorta was achieved with Chitwood clamp through separate incision in 5th intercostal space along the posterior axillary line with subsequent antegrade cardioplegia. Approach to the right atrium and interatrial septum was performed through the right atriotomy parallel to the interatrial sulcus (Figure 3). The large size of the ASD allowed ring annuloplasty of the mitral valve through the defect without additional left atriotomy. Mitral valve ring annuloplasty, De Vega annuloplasty of the tricuspid valve and closure of the interatrial septal defect with a bovine pericardial patch was completed during this part of the procedure. After completion of the cardiac stage and heparin reversal, attention was shifted to the thoracic part of the procedure. The middle lobe vein was isolated from the adhesions, tied, clipped, and transected. The middle lobe bronchus and artery as well as parenchymal bridge between the middle and upper lobes were divided with an endoscopic gastrointestinal anastomosis (endo GIA) stapler.
The total duration of surgery was 332 min, with 100 min of CPB time, and cross-clamp time of 79 min. Estimated blood loss was 800 mL. Patient was extubated 3 h postoperatively and transferred from the intensive care unit on the next day. Chest tube was removed on postoperative day 4. Patient was discharged home on postoperative day 8 without postoperative complications. At 10 months follow-up patient was doing well with significantly improved exercise tolerance and resolution of hemoptysis. Normalization of the cardiac chamber dimensions with absence of regurgitation were observed on echocardiography.
Discussion
Combined pathologies pose a difficult situation to clinicians—radically address all problems in one setting or take traditional staged approach. Even with the traditional strategy, sometimes it is difficult to decide which is the dominant condition, requiring attention first, either due to more urgent nature or potential negative impact on the safety of the whole procedure. Multiple publications in the literature address the success of cardiothoracic simultaneous operations for combined conditions, however almost all these operations are performed with open approach (2). The combination of cardiovascular and pulmonary septic pathology is specifically challenging in this regard. On the one hand, increased risk of the simultaneous procedure is real, especially in the settings of anticoagulation and CPB. On the other—careful planning is required for staged operations due to increased risk of septic complications from either persistent source or deterioration of uncorrected cardiac defect. The cornerstone of any such simultaneous operation is surgical access, that has greatly been facilitated with the development of thoracoscopic access for minimally invasive cardiac surgery and with peripheral CPB canulation (3,4). Although technically more challenging, cardiac interventions via mini-thoracotomy have numerous advantages, including preservation of the sternum integrity, enhanced postoperative recovery with lower complications rate and shorter hospital stay and excellent cosmetic results (5). As for surgical treatment of bronchiectatic disease, video-assisted thoracic surgery (VATS) is also superior for the same reasons (6). Such, VATS can be safely considered an established standard of care in thoracic surgery and discussions now is focusing on the details of multiportal versus uniportal thoracoscopic operations (7,8).
Conclusions
Presented case demonstrates potential advantage and feasibility of minimally invasive simultaneous procedures in patients with concurrent pulmonary and cardiac conditions. The described approach allowed radical surgical intervention to address both problems in the single setting, while retaining advantage of minimally invasive intervention. This is the first report in the literature of the simultaneous surgical management of septic pulmonary condition and congenital heart defect.
Acknowledgments
Funding: This research was funded in part through the NIH/NCI Cancer Center Support Grant P30 CA006927.
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at https://shc.amegroups.com/article/view/10.21037/shc-22-36/rc
Peer Review File: Available at https://shc.amegroups.com/article/view/10.21037/shc-22-36/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://shc.amegroups.com/article/view/10.21037/shc-22-36/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Davydov MI, Akchurin RS, Gerasimov SS, et al. Simultaneous operations in thoraco-abdominal clinical oncology. Eur J Cardiothorac Surg 2001;20:1020-4. [Crossref] [PubMed]
- Kuniyoshi Y, Koja K, Miyagi K, et al. One-stage operation for descending thoracic aortic aneurysm and left lung cancer: a case report. Ann Thorac Cardiovasc Surg 2001;7:237-40.
- Yu SQ, Cai ZJ, Cheng YG, et al. Video-assisted thoracoscopic surgery for congenital heart disease. Asian Cardiovasc Thorac Ann 2002;10:228-30. [Crossref] [PubMed]
- Arif R, Eichhorn F, Kallenbach K, et al. Resection of thoracic malignancies infiltrating cardiac structures with use of cardiopulmonary bypass. J Cardiothorac Surg 2015;10:87. [Crossref] [PubMed]
- Evseev EP, Balakin EV, Aidamirov YA, et al. Surgical treatment of heart valve disease and cardiac tumors via the right-sided minithoracotomy. Khirurgiia (Mosk) 2021;(6. Vyp. 2):37-44.
- Zhang P, Zhang F, Jiang S, et al. Video-assisted thoracic surgery for bronchiectasis. Ann Thorac Surg 2011;91:239-43. [Crossref] [PubMed]
- Wang L, Liu D, Lu J, et al. The feasibility and advantage of uniportal video-assisted thoracoscopic surgery (VATS) in pulmonary lobectomy. BMC Cancer 2017;17:75. [Crossref] [PubMed]
- Yu PSY, Chan KW, Lau RWH, et al. Uniportal video-assisted thoracic surgery for major lung resection is associated with less immunochemokine disturbances than multiportal approach. Sci Rep 2021;11:10369. [Crossref] [PubMed]
Cite this article as: Bazarov DV, Gritsiuta AI, Evseev EP, Petrov RV. Simultaneous minimally invasive uniportal atrial septal defect repair and pulmonary lobectomy: a case report. Shanghai Chest 2023;7:8.