
Optimisation of the high-risk thoracic surgical patient: a narrative review
Introduction
Thoracic surgical procedures are associated with significant postoperative morbidity. In particular, this review will focus on patients undergoing lung resection, which has been demonstrated to have a postoperative complication rate of 18.97% in the United Kingdom (UK) (1). The risk of complications has been shown to correlate with a patient’s existing co-morbidity, with the majority of postoperative morbidity and mortality concentrated within a subgroup of high-risk patients (2). This article defines high-risk as a patient with a preoperative comorbidity or behaviour which has been demonstrated to increase postoperative morbidity and/or mortality.
Several publications have examined the predictive ability of preoperative patient characteristics to estimate risk of postoperative complications and mortality. The RESECT model (3) was one such publication which examined the relation between preoperative characteristics and 90-day postoperative mortality. The variables included in the predictive model are age, sex, performance status, percentage predicted diffusion capacity of the lung for carbon monoxide (% DLCO), anaemia, serum creatinine, preoperative arrhythmia, right-sided resection, number of resected bronchopulmonary segments, open approach and malignant diagnosis. Whilst it is clear that some of these factors are not modifiable (age, sex, side of resection and malignant diagnosis), the remaining factors may be optimised with preoperative intervention. Further studies have also demonstrated that body mass index (BMI), nutritional status, smoking status and low socioeconomic status (4) are also independent predictors of postoperative morbidity (5-8). Optimisation of co-morbidities such as hypertension, cardiac ischaemia and diabetes play a key role in the work-up of the high-risk patient group, however evidence to demonstrate risk-reduction following these interventions is lacking.
The majority of lung resections are performed for the management of non-small cell lung cancer (NSCLC). This historically has been associated with relatively low resection rates in the UK, with evidence that increased resection rates are associated with better overall survival rates for lung cancer on a national scale (9). With this knowledge in-hand, the thoracic surgical community continue to strive to increase resection rates, which effectively equates to operating on patients with a higher rate of preoperative co-morbidity. This, in conjunction with the widespread role out of screening programmes, means that now, more than ever, it is essential for thoracic surgical teams to effectively and efficiently optimise high-risk patients.
The duration of preoperative optimisation is crucial in this cohort of patients. Concern regarding stage progression in primary lung cancer is a key factor, which concerns both patient and surgeon alike. It is therefore key that optimisation is performed over an appropriate timeframe based upon individual patient and tumour characteristics. The Enhanced Recovery After Surgery (ERAS) guidelines published in 2019, contain a number of recommendations for the optimisation and management of thoracic surgical patients in the perioperative period (10). Here we focus on optimising the high-risk surgical patient preoperatively. This review examines the current literature to summarise the key interventions that have a meaningful impact on the optimisation off the high-risk thoracic surgical patient. We present the following article in accordance with the Narrative Review reporting checklist (available at https://shc.amegroups.com/article/view/10.21037/shc-22-31/rc).
Methods
Between January and June 2022, the PubMed and BMJ database were used to search relevant subject headings including ‘thoracic surgery’, ‘lung cancer surgery/resection’, ‘high-risk’, ‘optimisation’, ‘smoking’, ‘BMI’, ‘nutrition’, ‘anaemia’, ‘iron deficiency’, ‘exercise’, ‘prehabilitation’, ‘hypertension’, ‘ischaemic heart disease’, ‘valvular heart disease’, ‘heart failure’, ‘myocardial infarction’, ‘chronic obstructive pulmonary disease (COPD)’, ‘diabetes’, ‘alcohol’ for research published between 1966–2022. As well as the database search, key articles relevant to the subject area known to the authors were included and their reference lists examined to identify relevant studies. Titles and abstracts were screened by all authors to identify those which represented the most up-to-date research pertinent to the topic under discussion.
Each study retrieved for inclusion was independently assessed by all three authors. The inclusion criteria included: (I) studies including randomised controlled trials, retrospective, cohort, or case-control studies, (II) reports on the correlation between lung resection postoperative outcomes and preoperative co-morbidities such as smoking, vaping, BMI, exercise, nutrition, cardiovascular disease, anaemia and alcohol, (III) study population in any country, (IV) full-text publication, and (V) research published in the English language. Exclusion criteria included: (I) case reports and series that infer a conclusion, and (II) articles with insufficient detailed data and irrelevant outcomes. More details of the methods are shown in Table 1.
Table 1
| Items | Specification |
|---|---|
| Date of search | 05.01.2022–20.06.2022 |
| Databases and other sources searched | PubMed, BMJ |
| Search terms used | “thoracic surgery” [MeSH] |
| “lung cancer surgery” [MeSH] | |
| “high-risk” [MeSH] | |
| “optimisation” [MeSH] | |
| (“smoking” [MeSH]) AND “lung cancer surgery” [MeSH] | |
| (“smoking” [MeSH]) AND “lung cancer resection” [MeSH] | |
| (“vaping” [MeSH]) AND “lung cancer” [MeSH] | |
| (“BMI” [MeSH]) AND “lung cancer surgery” [MeSH] | |
| (“BMI” [MeSH]) AND “lung cancer resection” [MeSH] | |
| (“nutrition” [MeSH]) AND “lung cancer surgery” [MeSH] | |
| (“nutrition” [MeSH]) AND “lung cancer resection” [MeSH] | |
| (“anaemia” [MeSH]) AND “lung cancer surgery” [MeSH] | |
| (“anaemia” [MeSH]) AND “lung cancer resection” [MeSH] | |
| (“iron deficiency” [MeSH]) AND “lung cancer surgery” [MeSH] | |
| (“iron deficiency” [MeSH]) AND “lung cancer resection” [MeSH] | |
| (“exercise” [MeSH]) AND “lung cancer surgery” [MeSH] | |
| (“exercise” [MeSH]) AND “lung cancer resection” [MeSH] | |
| (“prehabilitation” [MeSH]) AND “lung cancer surgery” [MeSH] | |
| (“prehabilitation” [MeSH]) AND “lung cancer resection” [MeSH] | |
| (“hypertension” [MeSH]) AND “lung cancer surgery” [MeSH] | |
| (“hypertension” [MeSH]) AND “lung cancer resection” [MeSH] | |
| (“ischaemic heart disease” [MeSH]) AND “lung cancer surgery” [MeSH] | |
| (“ischaemic heart disease” [MeSH]) AND “lung cancer resection” [MeSH] | |
| (“valvular heart disease” [MeSH]) AND “lung cancer surgery” [MeSH] | |
| (“valvular heart disease” [MeSH]) AND “lung cancer resection” [MeSH] | |
| (“heart failure” [MeSH]) AND “lung cancer surgery” [MeSH] | |
| (“heart failure” [MeSH]) AND “lung cancer resection” [MeSH] | |
| (“myocardial infarction” [MeSH]) AND “lung cancer surgery” [MeSH] | |
| (“myocardial infarction” [MeSH]) AND “lung cancer resection” [MeSH] | |
| (“myocardial ischaemia” [MeSH]) AND “lung cancer surgery” [MeSH] | |
| (“myocardial ischaemia” [MeSH]) AND “lung cancer resection” [MeSH] | |
| (“COPD” [MeSH]) AND “lung cancer surgery” [MeSH] | |
| (“COPD” [MeSH]) AND “lung cancer resection” [MeSH] | |
| (“diabetes” [MeSH]) AND “surgery” [MeSH] | |
| (“diabetes” [MeSH]) AND “lung cancer resection” [MeSH] | |
| (“alcohol” [MeSH]) AND “surgery” [MeSH] | |
| (“alcohol” [MeSH]) AND “lung resection” [MeSH] | |
| Timeframe | 1966–2022 |
| Inclusion and exclusion criteria | Inclusion criteria: research articles and reviews in English about themes such as lung resection surgery and high-risk patients, population studied in any country, full-text articles only, publications in English |
| Exclusion criteria: some papers which we considered with low reliability, articles that had no information on postoperative outcomes in relation to the preoperative variables identified | |
| Selection process | All authors independently conducted the search and combined search results |
| And additional considerations, if applicable | Some papers were identified by reviewing reference lists of relevant publications |
Discussion
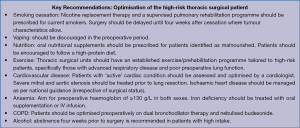
The key recommendations for the optimisation of the high-risk thoracic surgical patients as concluded from the literature review detailed below are summarised in Figure 1.
Smoking
Seventy-two percent of lung cancer cases are attributable to smoking (11) with approximately one-third of patients being current smokers at the time of diagnosis (12). Smoking prior to lung cancer surgery is one of the strongest predictors of postoperative complications (13-15), specifically postoperative pulmonary complications (PPCs) (13,16) including atelectasis, lower respiratory tract infection, prolonged air-leak, pneumothorax, respiratory failure, bronchospasm, aspiration pneumonitis, acute respiratory distress syndrome (ARDS) and pleural effusion. PPCs have been demonstrated to correlate with a higher mortality rate at six months (14), highlighting the importance of reducing these events not only to benefit short-term recovery but also long-term survival. Smoking cessation is therefore one of the key interventions that may be utilised for optimisation of this high-risk cohort of patients.
Whilst the majority of authors have demonstrated a reduction in rates of postoperative complications with cessation, controversy does exist, with some authors suggesting that short-term cessation may in fact increase risk (17). In the thoracic surgical cohort, the required time delay from cessation to surgery is key and once again is a point of contention. Both patient and surgeon alike fear prolonged waits prior to surgery due to possible tumour progression, however, wish to minimise postoperative complications. Existing literature, ranges from studies who find no difference in complications based on time from cessation to surgery (18), to those advising a two-month period to be optimal (19).
The Society of Thoracic Surgeons (STS) database study demonstrated that with increasing time from cessation to surgery the risk of in-hospital mortality and PPCs decreased and beyond one month the risk was no longer significant (15). Furthermore, a systematic review of the literature including six randomised trials and 15 observational studies suggested that every subsequent week from cessation lowered the risk of complications, the authors were also in favour of a four-week transition point to lower risk (20). The weight of evidence therefore suggests four weeks to be the optimal time from cessation to surgery, and this is reflected in the European Society of Thoracic Surgeons (ESTS) and ERAS Society guidelines (10). However, this delay must be considered in context with the individual patient and cancer characteristics in mind.
The timeframe available for cessation is an important consideration when deciding which smoking cessation techniques to utilise. Options vary from nicotine replacement therapy, cognitive behavioural therapy, Varenicline, Bupropion Hydrochloride to multimodal therapies (21). Randomised control trials have demonstrated Varenicline to be the most effective method of long-term cessation (22,23). However, Varenicline has currently been withdrawn from the market, therefore nicotine replacement therapy alone is the mainstay of pharmacological treatment. In the general population, the measurement of smoking cessation success is based on quit rate and longevity, however in a surgical cohort the most important factor is the speed of cessation given the time-limiting factor of cancer progression. Smoking cessation rates and prolonged abstinence increase when undergoing a supervised pulmonary rehabilitation program compared to medication alone (24) and smoking cessation incorporated into the surgical pathway is preferred by patients (25). Therefore, supervised/supported smoking cessation in conjunction with nicotine replacement therapy plays an essential role in the preoperative optimisation in this high-risk group.
Recommendation: Nicotine replacement therapy and a supervised pulmonary rehabilitation programme should be prescribed for current smokers. Surgery should be delayed until 4 weeks after cessation where tumour characteristics allow.
‘Vaping’ or the use of ‘e-cigarettes’ has been proposed as an alternative to cigarettes in current smokers prior to resection. However, evidence in this field in limited and data exists with regards to long-term effects and cancer risk. Multiple retrospective series have demonstrated lung injury and respiratory disease associated with the use of e-cigarettes, with reports of ARDS and mortality linked to their use (26). Although e-cigarettes were initially advertised as an aid to promote smoking cessation, there is no evidence-based research to support this supposition (27-29). One randomised trial found a similar quit rate when comparing nicotine containing e-cigarettes versus nicotine patches (30). The widely held belief amongst the general populous that e-cigarettes are less harmful than conventional cigarettes due to the absence of tobacco and tar in the products has been disproven (31,32). Vaping products have a similar level of harmful effects as conventional cigarettes due to the toxins used to carry the nicotine-containing products (31,32). Reports advise that each 5% cartridge in an e-cigarette is approximately equivalent to smoking one pack of cigarettes (33). With regards to the perioperative and postoperative period, the data is also limited. Research has shown that e-cigarette use is associated with increased postoperative complications (34,35) and currently no research exists regarding e-cigarette use prior to lung resection surgery. We therefore recommend that e-cigarettes are not advised prior to lung resection and that patients should be prescribed traditional nicotine replacement therapy.
Recommendation: vaping should be discouraged in the preoperative period.
Obesity and malnutrition
Obesity is putatively associated with worse outcomes due to more technically challenging surgery, with associated longer operative times (36) and a theoretical increase in pulmonary complications such as atelectasis caused by diaphragmatic splinting (37,38). However, the literature does not support this assumption. In keeping with our own institutional data, Ferguson et al. (39) showed that a BMI >25 kg/m2 was not associated with more PPCs or any other complication. In fact, some authors have found that a raised BMI is protective and associated with a significantly greater survival (40). Conversely a BMI <18 kg/m2 is associated with poorer postoperative outcomes, including an increased rate of PPCs and mortality (39) and the ERAS guidelines identify a BMI of <18.5 kg/m2 is an indicator for nutritional supplementation. It is therefore the optimisation of the malnourished patient which is key to reduce risk following thoracic surgery.
We must be wary when using BMI alone as a tool for assessing the health and nutritional status of a patient. Although BMI is simplistic and easy to use in clinical practice, it does not consider muscle mass, body composition or visceral fat (41). The Thoracic ERAS guidelines recommend the use of nutritional scoring systems beyond a simple BMI (10). Two of which they recommend are Malnutrition Universal Screening Tool (MUST) and Nutritional Risk Screening (NRS) (10). More complex measures of nutrition such as Indexed Total Muscle mass have also demonstrated a predictive ability of postoperative outcomes, however, are not routinely used in clinical practice due to their complexity (42).
Malnutrition may also be identified by measuring albumin levels. Bagan et al. (43) have shown a correlation between low preoperative albumin level and a low BMI (43). The team used an albumin level of <35 g/L as a marker for malnutrition and an indicator of hypercatabolism (43). Both the ERAS and ESPEN (European Society for Clinical Nutrition and Metabolism) guidelines also use low preoperative albumin levels as an indicator of malnutrition. In these guidelines an albumin below 30 g/L with no evidence of hepatic or renal dysfunction is an indicator for preoperative enteral nutrition (10). Nutritional supplementation can increase albumin level and alter protein metabolism from a catabolic to anabolic state. This has been demonstrated in patients with COPD following the addition of branched-chain amino acids (common in whey protein isolate) to a standard protein meal (42,44). A number of authors recommend a daily intake of 1.5 g/kg/day of protein (45,46). A preoperative 10-day diet with an immune modulating formula, containing arginine, omega-3 fatty acids and nucleotides was also found to significantly improve postoperative albumin levels with resultant lower PPC rates (mainly air-leak and length of chest tube drainage time) in patients undergoing lung cancer resection (6,45). This suggests that improving the protein intake and albumin level in this high-risk cohort reduces the risk of developing postoperative complications.
The duration of optimisation is once again controversial. While the ERAS guidelines suggest 5–7 days of preoperative nutrition in those that are deplete (along with the routine use of preoperative oral carbohydrate drinks) (10), prehabilitation studies in other surgical specialties use at least four-week protocols (47,48). In contrast to the ERAS guidelines, the ESPEN guidelines recommend 7–14 days of preoperative nutrition in patients who are undernourished (49). ESPEN also recommend that approximately seven days of preoperative parenteral nutrition should be given to those who are at severe nutritional risk (49).
In conclusion, a number of methods may be used to identify this high-risk cohort of patients with nutritional depletion, a combination of low albumin level, low BMI or abnormal nutritional scores [MUST >2/nutrition risk index (NRI) <83.5] (10) may be employed depending on resource. Nutritional supplementation, a high-protein and an immune modulating diet have all demonstrated a reduction in postoperative complications in the nutritionally deplete following lung resection, however, there is still some debate regarding the duration of administration. In the context of lung cancer, it is imperative that nutritional supplementation is started as soon as possible due to the short window between diagnosis and surgical intervention.
Recommendation: Patients identified as malnourished should be started on nutritional supplementation and encouraged to follow a high protein diet.
Frailty or physical inactivity
Preoperative exercise tolerance has been shown to predict survival and morbidity in patients undergoing surgery for lung cancer resection or lung volume reduction (50). Peak oxygen utilisation (VO2 max) as measured by cardiopulmonary exercise testing correlates well with complication rate (51). Exercise rehabilitation has therefore been recommended by current clinical practice guidelines for high-risk patients undergoing thoracic surgery procedures (48,52). Multiple preoperative exercise studies in patients with operable lung cancer have shown a significant improvement in VO2 max (53-57). Meta-analyses and systematic review of the effectiveness of exercise training also reported significant improvements in lung function and exercise capacity (FEV1, VO2 max and/or 6-minute walk test), as well as significant reductions in length of hospital stay and frequency of PPCs (58). The effect on reduction of PPCs was more marked in high-risk patients with poor lung function, patients with severe COPD confer the greatest benefit from exercise training (54,59). Measurable improvements have also been demonstrated in the frail and elderly (60,61). Importantly, pulmonary rehabilitation and exercise training can improve medically inoperable patients’ fitness parameters to a level where surgery can be offered at a reasonable level of risk (52,55).
The duration of exercise training required is a more challenging question, Benzo et al. (62) trialled an intensive one week of training prior to lung resection for cancer but were unable to show significant postoperative improvement and the trial was stopped early as patients and their surgeons were unwilling to wait the four-week recommended training period of the trial. A recent review of preoperative exercise trials found the majority had an exercise period of around four weeks but with a high degree of heterogeneity (63). In practice this will be a highly individualised decision based on oncological characteristics and patient motivation/adherence to the programme. Medically inoperable patients who became operable after an exercise regime required differing lengths of time to meet surgical parameters.
There is no consensus regarding the recommended type of exercise regimen, the large heterogeneity between trials in terms of duration, types of exercise included and even inclusion of smoking cessation and nutrition make it difficult to tease out the exact exercises that can be recommended (63). Trialled exercise regimes can vary but broadly fit into three groups: aerobic exercise, muscle strengthening and respiratory muscle exercises. There is a large degree of overlap, and no single study has proven its superiority over another. Trials which combine multiple types of training show beneficial results (46) as do those using specific breathing exercises (64). Most trials and good programmes now provide a combination of all three to some extent. Putatively muscle strengthening exercise with correct nutrition aids an anabolic state, aerobic exercise improves VO2 max and oxygen utilisation and respiratory muscle exercises improves perioperative cough strength.
Crucially, given the recent COVID restrictions and cost limitations of many economies, providing a hospital or gym-based service with expert physiotherapists is expensive and difficult to access for patients. The advent of fitness watches and app-based training provides an opportunity to reach patients at home and increase the intensity of their training providing that incentives, motivation and remote supervision is offered (65).
In conclusion, the existing literature strongly supports all forms of exercise rehabilitation in the preoperative setting, which equates to reduce post-operative morbidity. Thoracic surgical units should have formulated exercise programme to optimise patients, specifically those who suffer with severe respiratory disease or frailty, who will confer the greatest benefit.
Recommendation: Thoracic surgical units should have an established exercise/prehabilitation programme tailored to high-risk patients, specifically those with advanced respiratory disease and poor preoperative lung function.
Optimisation of co-morbidities
Anaemia and low iron states
Preoperative anaemia is common in lung cancer surgery patients with a reported prevalence of 26% (66). Preoperative anaemia is associated with postoperative morbidity and mortality (67), not only in lung resection surgery (46) but also in other surgical specialties (68,69). A number of authors postulate that the anaemia-associated postoperative morbidity is due to the increased rate of perioperative red cell transfusion rather than the actual anaemia itself (70), as blood transfusion has been linked to unfavourable outcomes (67,71,72). Regardless, treating preoperative anaemia will reduce the likelihood of receiving the blood transfusion and thus whether the postoperative morbidity and mortality is due to the anaemia or blood transfusion is inconsequential. Evidence has shown that correcting anaemia prior to surgery results in improved surgical outcomes (68,69). Perioperative blood transfusion to treat preoperative anaemia has no sound evidence base and has been shown to have no benefit with regards to postoperative outcomes. Further, perioperative blood transfusion has not reduced the need for intra- or postoperative transfusion (10).
The cause of the anaemia can be multi-factorial but is most commonly related to iron-deficiency (73)—whether this is independent of the cancer or due to the cancer (i.e., iron sequestration due to the cancer-related inflammatory state) is unclear (74). Iron-deficiency anaemia can be easily managed with iron therapy and nutritional advice. Oral iron supplementation is commonly used, however, there are some limitations to this option including time to effect and absorption variability (75). Additionally, the duration of treatment will vary depending on the patient’s initial haemoglobin and time taken to reach an acceptable value. Muñoz et al. (74) have reported that the international consensus regarding target haemoglobin levels should be ≥130 g/L in both sexes. Intravenous iron treatment has been recommended if a patient has persistent iron-deficiency within six weeks of the scheduled surgery, if treatment with oral iron has had no effect or a patient cannot tolerate the treatment (68). Research has shown that preoperative intravenous iron infusion reduces the need for blood transfusion, risk of acute kidney injury, postoperative infections and length of stay in cardiac and orthopaedic surgery (76,77). However, in a randomised controlled study investigating intravenous iron administration in elective major abdominal surgery, researchers found that there was no significant difference in the need for blood transfusion (78). Again, dosage of intravenous iron will vary with each patient depending on the patient’s weight and haemoglobin and ferritin values.
Low iron states without anaemia can also exist in patients. If the iron-deficiency does not lead to a resultant anaemic state, serious underlying pathology should be considered, including chronic hypoxaemia, myeloproliferative disease, gastrointestinal disorders or any other cause of increased red blood cell production (73). These conditions must be ruled out first, as treating the low iron state with supplements could induce hyperviscosity (73).
In conclusion, the cause for the low iron state or iron-deficiency anaemia should be identified as soon as possible preoperatively. Management with iron supplementation or treatment of the underlying cause should be commenced as soon as possible prior to lung resection surgery for at least four weeks. However, as with the other aforementioned preoperative co-morbidities, each patient will have to be assessed on a case-by-case basis. The time to effect is important particularly in lung resection surgery to minimise delay.
Recommendation: Aim for preoperative haemoglobin of ≥130 g/L in both sexes. Iron deficiency should be treated with oral supplementation or IV infusion.
Cardiovascular disease
The majority of thoracic surgical patients also suffer with cardiovascular disease, ranging from isolated hypertension to severe ischaemic and valvular heart disease. Hypertension only presents increased perioperative risk when severe (79). Guidelines for the management of hypertension before elective surgery suggest that if preoperative blood pressure is less than 180 mmHg systolic or 110 mmHg diastolic, surgery should proceed without further delay (80). Where hypertension is severe, a balance should be sought between the risks of significant perioperative hypertension against that of delaying surgery (81).
Patients with significant ischaemic heart disease (IHD) or valvular lesions are at high-risk of complications, including myocardial infarction (MI) and mortality (82). The British Thoracic Society Guidelines (83) recommend that all patients with an ‘active cardiac condition’ are evaluated and optimised by a cardiologist. Active conditions include unstable coronary syndromes, decompensated heart failure (HF), significant arrhythmias and severe valvular disease. Specifically severe aortic and mitral stenosis typically require intervention prior to lung resection, due to the prohibitive risk of perioperative events (84). There are no trials to guide the interval from valvular intervention to lung cancer resection, but case reports have reported a short duration (six weeks) between successful transcatheter interventions and lung cancer surgery (85).
Coronary artery disease should be treated as per guidance for myocardial ischaemia patients with no difference recommended for patients needing elective surgery or not (84,86). Routine angiography even in high-risk patients is not recommended unless they have evidence of myocardial ischaemia. Patients undergoing non-cardiac surgery in the first six months after coronary stenting are at increased risk of death and MI (87) and prophylactic coronary stenting for patients undergoing vascular limb surgery showed no benefit in either postoperative MI or mortality rate (88). There is no specific reliable data for the management of IHD in patients undergoing lung cancer resection, but extrapolating this, in conjunction with guidelines for non-cardiac surgery suggests that delineating risk is useful when counselling patients to enable them to make decisions regarding surgery versus alternative treatments but adds little benefit with regards to preoperative optimisation. Clinicians should ensure that all patients with identified IHD have appropriate secondary prophylactic medications prescribed, which should be continued throughout the perioperative period.
Patients with HF represent a very high-risk surgical cohort. Little data exists pertaining to thoracic surgery alone, however multiple trials have grouped together the ‘non-cardiac’ surgical specialties to examine the outcome of surgery in patients with HF. A 50-100% increase in postoperative mortality and readmission rates, has been reported in patients with HF undergoing non-cardiac surgery when compared with control groups without cardiac disease (89,90). One large study demonstrated significantly higher postoperative mortality rates in patients with HF (9.3%) when compared those with IHD alone (2.6%) (91). A further study examining non-cardiac surgery in patients with HF, demonstrated a sharp increase in morbidity and mortality rates in patients with low ejection fractions (EF), those who had an EF <30% had a 14.3% mortality rate and 53.6% incidence of major cardiac event (death, MI or HF exacerbation) at 30 days (92). Despite significant data for non-cardiac surgery in this cohort demonstrating a substantial risk of morbidity and mortality, no guidelines exist with regards to preoperative optimisation. Optimisation in this patient group is primarily in the domain of HF specialist teams. The role of the thoracic surgical team is essentially to identify those at risk and ensure specialist optimisation has occurred. Preoperative brain naturistic peptide (BNP) and echocardiogram are the key investigations performed to identify and quantity HF (86).
For patients without an active condition but existing cardiac risk factors, the Revised Cardiac Risk Index (RCRI) is a useful screening tool and has been validated across-surgical specialties to identify patients at increased risk of perioperative cardiac events and mortality (91,93). The RCRI is a risk score comprising of six equally weighted factors: history of IHD, congestive HF, cerebrovascular disease, insulin-dependent diabetes, serum creatinine level >177 mmol/L, and high-risk surgery. Those with >3 risk factors have a 11% risk of major cardiac complications including acute MI, pulmonary oedema, ventricular fibrillation, complete heart block, and cardiac-related death (94). This index has been adapted specifically for thoracic surgical patients and identified four of the original variables to accurately predict risk of complication [cerebrovascular disease, cardiac ischaemia, renal disease and high-risk surgery (specifically pneumonectomy)]. This new index was coined the Thoracic Revised Cardiac Risk Index (95). Either model may be used to identify this high-risk patient cohort, in order to initiate appropriate investigation and management.
Recommendation: Patients with ‘active’ cardiac condition should be assessed and optimised by a cardiologist. Severe mitral and aortic stenosis should be treated prior to lung resection. IHD should be managed as per national guidance (irrespective of surgical status).
COPD
A significant proportion of patients undergoing thoracic surgery suffer from chronic obstructive pulmonary disease. These patients are at high-risk of postoperative complications, specifically PPCs and optimisation of this disease forms a key component in reducing perioperative risk. Takegahara et al. (96) found in a retrospective comparison of patients undergoing lung cancer surgery, that those on preoperative inhalers were less likely to have PPCs. Adding inhaled budesonide to a regime of inhaled tiotropium and formoterol, along with smoking cessation and chest physiotherapy in newly diagnosed COPD patients undergoing lung cancer surgery significantly reduced the PPC rate after one week of therapy compared to patients who were on a regime of tiotropium and formoterol (11.1% vs. 42.9%, P=0.04) (97). Increasing the treatment duration does not improve outcomes when comparing treatment duration of less than or greater than two weeks (98). Ju et al. also investigated the effect of perioperative nebulised budesonide on outcomes following lobectomy. The authors report a reduction in both peak and plateau ventilatory pressures and improved lung compliance in the collapsed and ventilated lung during surgery. Additionally, a reduction in the inflammatory cytokines (TNF-α, IL-1b, IL-6, IL-8), but an increase in the anti-inflammatory cytokine IL-10, was found in the in the bronchoalveolar lavage fluid in the budesonide group (99). Inflammatory cytokines (IL-6 and IL-8) have been shown to be increased in patients who developed postoperative complications following lung cancer surgery (100). These results indicated that preoperative nebulised budesonide both improves respiratory and ventilatory mechanics, as well as modulate the inflammatory response perioperatively.
Aerosolised salbutamol was investigated by Licker et al. The authors demonstrated that perioperative nebulised salbutamol (5 mg) in lung resection surgery patients led to improved haemodynamics, blood oxygenation and an acceleration in the resolution lung oedema in acute postoperative period (101). Manocha et al. also investigated the effect of low-dose (2.2 mg) vs. high-dose (≥2.2 mg) salbutamol in mechanically ventilated patients with acute lung injury. They found that a higher dose of salbutamol resulted in a shorter duration and lower severity of acute lung injury (102). These results support the conclusion reached by Licker et al. that preoperative nebulised salbutamol reduced PPCs (101).
Shin et al. (103) examined the impact of perioperative combination bronchodilator therapy in COPD patients undergoing lung cancer surgery. Five groups were examined: those taking long-acting muscarinic antagonist (LAMA) only vs. long-acting beta-2 agonist (LABA) with inhaled corticosteroid (ICS) vs. LAMA with LABA vs. LAMA and LABA with ICS vs. patients not taking bronchodilator therapy. LAMA or LABA +/− ICS was classified as monotherapy as ICS was not classified as a bronchodilator and LAMA and LABA +/− ICS was classified as dual therapy. The study found an improvement in lung function with all types of bronchodilator therapy persisting at 12 months postoperatively when compared to those not taking any bronchodilator therapy, a greater benefit was demonstrated in the dual bronchodilator group. The findings by Kobayashi et al. (104) corroborate these results—a two-week treatment with tiotropium (LABA) significantly improved lung function postoperatively in COPD patients receiving lung cancer resection surgery. This again is supported by Makino et al. (105) who found that lung function and PPCs (specifically pneumonia) was improved with dual LAMA/LABA therapy when compared to LAMA monotherapy in COPD patients receiving lung resection surgery. Interestingly, the research by Shin et al. (103) showed that the frequency of overall PPC did not significantly differ with perioperative bronchodilator therapy. The authors suggested that other variables such as the older age and lower baseline FEV1 and DLCO found in the bronchodilator group may have impacted the PPC occurrence rate.
In conclusion, perioperative dual bronchodilator therapy is optimal for the optimisation of patients with COPD undergoing lung resection, the addition of nebulised budesonide in particular seems to play a crucial role in improving lung function postoperatively and reducing PPCs. However, the duration of bronchodilator therapy prior to surgery has not yet been assessed and requires a randomised controlled study to see if a longer duration of treatment improves postoperative outcomes. Furthermore, a direct comparison between the effect of perioperative nebulisers and inhaled bronchodilator therapy requires research. Interestingly, despite the clear benefits of bronchodilator therapy prior to lung resection surgery as demonstrated in the aforementioned research, the ERAS and ESTS guidelines (10) do not include bronchodilator therapies as a recommendation in the perioperative management of thoracic patients.
Recommendation: Patients should be optimised preoperatively on dual bronchodilator therapy and nebulised budesonide.
Diabetes
Diabetes is considered a perioperative risk factor for poor wound healing, infection and mortality following surgery. In 468 lung cancer resection patients’ data analysed retrospectively, Motoishi et al. (106) suggested that high preoperative HbA1c levels was an independent poor prognostic factor for survival at five years in the elderly cohort. However, there was no increase in postoperative complication rate, no difference in the non-elderly cohort and the excess deaths in the elderly high HbA1c group were all non-cancer related. Interestingly, a systematic review by Buchleitner et al. (107) of patients undergoing cardiac, abdominal, and major limb surgery was unable to elicit an advantage of perioperative glucose control. This conclusion was supported by a further systematic review by Rollins et al. (108) of 20 studies across surgical specialties which concluded that preoperative glycaemic control measured by HbA1c had no impact on postoperative morbidity or mortality.
However, a subsequent systematic review by Wang et al. (109) of 5,053 patients undergoing major surgery, comparing tight postoperative glycaemic control and conventional glycaemic control, did show significant reduction in postoperative infection rate (9.4% vs. 15.8%, P<0.001) and short-term mortality (3.8% vs. 5.4%, P=0.008). This suggests that while glucose control perioperatively is important, diabetes per se is less so. In fact, a retrospective analysis of 40,836 postoperative abdominal, vascular and spinal surgery patients suggested that diabetes may be protective for patients with hyperglycaemia. They found that non-diabetic patients with postoperative hyperglycaemia had a significantly higher risk of complications but that diabetics with hyperglycaemia did not (110).
While it is prudent to recommend patients optimise their glycaemic control anyway to prevent long-term diabetic complications, there is no indication for delaying surgery to attain better glycaemic control or achieve specific HbA1c targets. Perioperative glycaemic control maybe important in all patients, not just those with diabetes, although there is no evidence to support this in our group of interest i.e., high-risk lung cancer resection patients.
Recommendation: Thoracic surgery should not be delayed to attain glycaemic control.
Alcohol dependency
The World Health Organization report that excessive alcohol intake is a major burden on disease (111). A heavy alcohol intake correlates well with an increased complication rate in patients undergoing elective surgery (112,113). Research has shown that in a cohort of 177 patients undergoing lung resection surgery between 1997 and 1998, there was an approximately 20% increase in 30-day postoperative mortality in patients who were classified as ‘heavy’ alcohol users. They also showed that the rate of major complications was significantly increased amongst the heavy drinker group (114). This data suggests that reducing or even stopping alcohol consumption prior to surgery will reduce postoperative morbidity and mortality following thoracic surgery.
Egholm et al. (113) conducted a meta-analysis of preoperative intervention in orthopaedic and colorectal surgery for risky drinkers, which includes three randomised unblinded trials of intervention including combination pharmacological and psychotherapy techniques. All trials employed a combination of Disulfiram (dose varied from 400 mg to 1.6 g/week), Chlordiazepoxide (as required), B Vitamins and regular psychological support through counselling and interviews, the length of intention varied from 4 to 12 weeks. All complication rates including PPCs were significantly reduced in the alcohol cessation intervention group but there was no effect on hospital length of stay or mortality. The authors suggest that the reduction in the postoperative complications in the alcohol cessation group is likely due to the intervention being offered for 4-8 weeks to achieve complete alcohol cessation prior to surgery (114).
There is currently no data available with regards to the effect of alcohol cessation on lung resection surgery. However, the data from the above Cochrane Review suggests that the interventions can be transposed and applied to lung resection surgery. An intervention of at least four weeks should be implemented [as supported by the ERAS guidelines (10)] with disulfiram at a dosage of at least 400 mg/week, B vitamins, chlordiazepoxide given prophylactically or as required and psychological support to encourage alcohol cessation prior to lung resection surgery (115). The exact effect of each of these factors and the preoperative intervention period should be a basis for future research.
A significantly greater proportion of patients who abuse alcohol are also smokers, when compared to the general population. The authors showed that unhealthy alcohol use with smoking was associated with an increased risk of postoperative complications when compared to patients who did not smoke (116). This points to the synergistic role of alcohol and smoking. Indeed, there is a putative link between smoking, excess alcohol, malnutrition and sarcopenia creating the “perfect storm” for postoperative complications in the setting of lung cancer surgery (117). These patients carry a significant risk of morbidity and mortality and require multi-modal therapy to address each risk-factor.
Recommendation: Abstinence from alcohol should be supported with a combination of pharmacological and psychotherapy techniques in those with a history of alcohol abuse.
Conclusions
High rates of postoperative morbidity and mortality exist following thoracic surgery in the high-risk patient cohort. These must be optimised where able to reduce individual suffering and overall resource utilization of healthcare systems. In the context of lung cancer, the duration of optimisation is key and needs to be decided on a case-by-case basis dependent on patient and tumour characteristics. The majority of interventions detailed above can be completed within a 4-week timeframe, which is usually acceptable to both patient and surgeon. Investing time and money into the modalities that maximise risk reduction is crucial. We have a duty to particularly focus on high-risk surgical patients as often it is the most vulnerable patients with the least opportunity for healthcare intervention that are at highest risk. Many of the interventions that optimise patients are both low cost and relatively easy to provide. As resection rates increase and lung cancer screening roles out, now, more than ever, the thoracic surgical community must become experts in the optimisation of high-risk patients in order to best utilise available resources and meet increasing demand.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editors (Marcus Taylor and Felice Granato) for the series “Thoracic Surgery in High Risk Patients” published in Shanghai Chest. The article has undergone external peer review.
Reporting Checklist: The authors have completed the Narrative Review reporting checklist. Available at https://shc.amegroups.com/article/view/10.21037/shc-22-31/rc
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://shc.amegroups.com/article/view/10.21037/shc-22-31/coif). The series “Thoracic Surgery in High Risk Patients” was commissioned by the editorial office without any funding or sponsorship. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Getting it right first time. Cardiothoracic Surgery. GIRFT Programme National Specialty Report. 2018. Accessed June 16, 2022. Available online: https://gettingitrightfirsttime.co.uk/wp-content/uploads/2018/04/GIRFT-Cardiothoracic-Report-1.pdf
- Pearse RM, Harrison DA, James P, et al. Identification and characterisation of the high-risk surgical population in the United Kingdom. Crit Care 2006;10:R81. [Crossref] [PubMed]
- Taylor M, Martin GP, Abah U, et al. Development and internal validation of a clinical prediction model for 90-day mortality after lung resection: the RESECT-90 score. Interact Cardiovasc Thorac Surg 2021;33:921-7. [Crossref] [PubMed]
- Wan YI, McGuckin D, Fowler AJ, et al. Socioeconomic deprivation and long-term outcomes after elective surgery: analysis of prospective data from two observational studies. Br J Anaesth 2021;126:642-51. [Crossref] [PubMed]
- Tjeertes EK, Hoeks SE, Beks SB, et al. Obesity--a risk factor for postoperative complications in general surgery? BMC Anesthesiol 2015;15:112. Erratum in: BMC Anesthesiol 2015;15:155. [Crossref] [PubMed]
- Kaya SO, Akcam TI, Ceylan KC, et al. Is preoperative protein-rich nutrition effective on postoperative outcome in non-small cell lung cancer surgery? A prospective randomized study. J Cardiothorac Surg 2016;11:14. [Crossref] [PubMed]
- Grønkjær M, Eliasen M, Skov-Ettrup LS, et al. Preoperative smoking status and postoperative complications: a systematic review and meta-analysis. Ann Surg 2014;259:52-71. [Crossref] [PubMed]
- Agabiti N, Cesaroni G, Picciotto S, et al. The association of socioeconomic disadvantage with postoperative complications after major elective cardiovascular surgery. J Epidemiol Community Health 2008;62:882-9. [Crossref] [PubMed]
- Riaz SP, Lüchtenborg M, Jack RH, et al. Variation in surgical resection for lung cancer in relation to survival: population-based study in England 2004-2006. Eur J Cancer 2012;48:54-60. [Crossref] [PubMed]
- Batchelor TJP, Rasburn NJ, Abdelnour-Berchtold E, et al. Guidelines for enhanced recovery after lung surgery: recommendations of the Enhanced Recovery After Surgery (ERAS®) Society and the European Society of Thoracic Surgeons (ESTS). Eur J Cardiothorac Surg 2019;55:91-115. [Crossref] [PubMed]
- Brown KF, Rumgay H, Dunlop C, et al. The fraction of cancer attributable to modifiable risk factors in England, Wales, Scotland, Northern Ireland, and the United Kingdom in 2015. Br J Cancer 2018;118:1130-41. [Crossref] [PubMed]
- Garces YI, Yang P, Parkinson J, et al. The relationship between cigarette smoking and quality of life after lung cancer diagnosis. Chest 2004;126:1733-41. [Crossref] [PubMed]
- Agostini P, Cieslik H, Rathinam S, et al. Postoperative pulmonary complications following thoracic surgery: are there any modifiable risk factors? Thorax 2010;65:815-8. [Crossref] [PubMed]
- Lugg ST, Agostini PJ, Tikka T, et al. Long-term impact of developing a postoperative pulmonary complication after lung surgery. Thorax 2016;71:171-6. [Crossref] [PubMed]
- Mason DP, Subramanian S, Nowicki ER, et al. Impact of smoking cessation before resection of lung cancer: a Society of Thoracic Surgeons General Thoracic Surgery Database study. Ann Thorac Surg 2009;88:362-70; discussion 370-1. [Crossref] [PubMed]
- Sekine Y, Suzuki H, Yamada Y, et al. Severity of chronic obstructive pulmonary disease and its relationship to lung cancer prognosis after surgical resection. Thorac Cardiovasc Surg 2013;61:124-30. [Crossref] [PubMed]
- World Health Organization. Tobacco and postsurgical outcomes. Accessed June 16, 2022. Available online: https://apps.who.int/iris/bitstream/handle/10665/330485/9789240000360-eng.pdf
- Matsuoka K, Yamada T, Matsuoka T, et al. Preoperative Smoking Cessation Period Is Not Related to Postoperative Respiratory Complications in Patients Undergoing Lung Cancer Surgery. Ann Thorac Cardiovasc Surg 2019;25:304-10. [Crossref] [PubMed]
- Moores LK. Smoking and postoperative pulmonary complications. An evidence-based review of the recent literature. Clin Chest Med 2000;21:139-46. ix-x. [Crossref] [PubMed]
- Mills E, Eyawo O, Lockhart I, et al. Smoking cessation reduces postoperative complications: a systematic review and meta-analysis. Am J Med 2011;124:144-154.e8. [Crossref] [PubMed]
- National Institute for Health and Care Excellence. Smoking Cessation. Accessed June 14, 2022. Available online: https://bnf.nice.org.uk/treatment-summaries/smoking-cessation/
- Wong J, Abrishami A, Yang Y, et al. A perioperative smoking cessation intervention with varenicline: a double-blind, randomized, placebo-controlled trial. Anesthesiology 2012;117:755-64. [Crossref] [PubMed]
- Anthenelli RM, Benowitz NL, West R, et al. Neuropsychiatric safety and efficacy of varenicline, bupropion, and nicotine patch in smokers with and without psychiatric disorders (EAGLES): a double-blind, randomised, placebo-controlled clinical trial. Lancet 2016;387:2507-20. [Crossref] [PubMed]
- Postolache P, Nemeş RM, Petrescu O, et al. Smoking cessation, pulmonary rehabilitation and quality of life at smokers with COPD. Rev Med Chir Soc Med Nat Iasi 2015;119:77-80.
- Farley A, Aveyard P, Kerr A, et al. Surgical lung cancer patients' views about smoking and support to quit after diagnosis: a qualitative study. J Cancer Surviv 2016;10:312-9. [Crossref] [PubMed]
- Gotts JE, Jordt SE, McConnell R, et al. What are the respiratory effects of e-cigarettes? BMJ 2019;366:l5275. [Crossref] [PubMed]
- Dutra LM, Glantz SA. Electronic cigarettes and conventional cigarette use among U.S. adolescents: a cross-sectional study. JAMA Pediatr 2014;168:610-7. Erratum in: JAMA Pediatr 2014;168:684. [Crossref] [PubMed]
- Grana RA, Popova L, Ling PM. A longitudinal analysis of electronic cigarette use and smoking cessation. JAMA Intern Med 2014;174:812-3. [Crossref] [PubMed]
- Fracol M, Dorfman R, Janes L, et al. The Surgical Impact of E-Cigarettes: A Case Report and Review of the Current Literature. Arch Plast Surg 2017;44:477-81. [Crossref] [PubMed]
- Bullen C, Howe C, Laugesen M, et al. Electronic cigarettes for smoking cessation: a randomised controlled trial. Lancet 2013;382:1629-37. [Crossref] [PubMed]
- Etter JF. Levels of saliva cotinine in electronic cigarette users. Addiction 2014;109:825-9. [Crossref] [PubMed]
- Walley SC, Jenssen BP. Section on Tobacco Control. Electronic Nicotine Delivery Systems. Pediatrics 2015;136:1018-26. [Crossref] [PubMed]
- Prochaska JJ, Vogel EA, Benowitz N. Nicotine delivery and cigarette equivalents from vaping a JUULpod. Tob Control 2022;31:e88-93. [Crossref] [PubMed]
- Sadr Azodi O, Bellocco R, Eriksson K, et al. The impact of tobacco use and body mass index on the length of stay in hospital and the risk of post-operative complications among patients undergoing total hip replacement. J Bone Joint Surg Br 2006;88:1316-20. [Crossref] [PubMed]
- De la Garza Ramos R, Goodwin CR, Qadi M, et al. Impact of Smoking on 30-day Morbidity and Mortality in Adult Spinal Deformity Surgery. Spine (Phila Pa 1976) 2017;42:465-70. [Crossref] [PubMed]
- St Julien JB, Aldrich MC, Sheng S, et al. Obesity increases operating room time for lobectomy in the society of thoracic surgeons database. Ann Thorac Surg 2012;94:1841-7. [Crossref] [PubMed]
- Kelkar KV. Post-operative pulmonary complications after non-cardiothoracic surgery. Indian J Anaesth 2015;59:599-605. [Crossref] [PubMed]
- Sprung J, Whalley DG, Falcone T, et al. The effects of tidal volume and respiratory rate on oxygenation and respiratory mechanics during laparoscopy in morbidly obese patients. Anesth Analg 2003;97:268-74. table of contents. [Crossref] [PubMed]
- Ferguson MK, Im HK, Watson S, et al. Association of body mass index and outcomes after major lung resection. Eur J Cardiothorac Surg 2014;45:e94-9; discussion e99. [Crossref] [PubMed]
- Wang C, Guo M, Zhang N, et al. Association of body mass index and outcomes following lobectomy for non-small-cell lung cancer. World J Surg Oncol 2018;16:90. [Crossref] [PubMed]
- Kok P, Seidell JC, Meinders AE. The value and limitations of the body mass index (BMI) in the assessment of the health risks of overweight and obesity. Ned Tijdschr Geneeskd 2004;148:2379-82.
- Icard P, Schussler O, Loi M, et al. Pre-Disease and Pre-Surgery BMI, Weight Loss and Sarcopenia Impact Survival of Resected Lung Cancer Independently of Tumor Stage. Cancers (Basel) 2020.
- Bagan P, Berna P, De Dominicis F, et al. Nutritional status and postoperative outcome after pneumonectomy for lung cancer. Ann Thorac Surg 2013;95:392-6. [Crossref] [PubMed]
- Engelen MP, Rutten EP, De Castro CL, et al. Supplementation of soy protein with branched-chain amino acids alters protein metabolism in healthy elderly and even more in patients with chronic obstructive pulmonary disease. Am J Clin Nutr 2007;85:431-9. [Crossref] [PubMed]
- McClave SA, Kozar R, Martindale RG, et al. Summary points and consensus recommendations from the North American Surgical Nutrition Summit. JPEN J Parenter Enteral Nutr 2013;37:99S-105S. [Crossref] [PubMed]
- Liu Z, Qiu T, Pei L, et al. Two-Week Multimodal Prehabilitation Program Improves Perioperative Functional Capability in Patients Undergoing Thoracoscopic Lobectomy for Lung Cancer: A Randomized Controlled Trial. Anesth Analg 2020;131:840-9. [Crossref] [PubMed]
- Borloni B, Huettner H, Schuerholz T. Preoperative Nutritional Conditioning: Why, When and How. Visc Med 2019;35:299-304. [Crossref] [PubMed]
- Ferreira V, Minnella EM, Awasthi R, et al. Multimodal Prehabilitation for Lung Cancer Surgery: A Randomized Controlled Trial. Ann Thorac Surg 2021;112:1600-8. [Crossref] [PubMed]
- Weimann A, Braga M, Carli F, et al. ESPEN guideline: Clinical nutrition in surgery. Clin Nutr 2017;36:623-50. [Crossref] [PubMed]
- Bolliger CT, Jordan P, Solèr M, et al. Pulmonary function and exercise capacity after lung resection. Eur Respir J 1996;9:415-21. [Crossref] [PubMed]
- Pehlivan E, Turna A, Gurses A, et al. The effects of preoperative short-term intense physical therapy in lung cancer patients: a randomized controlled trial. Ann Thorac Cardiovasc Surg 2011;17:461-8. [Crossref] [PubMed]
- Nici L, Donner C, Wouters E, et al. American Thoracic Society/European Respiratory Society statement on pulmonary rehabilitation. Am J Respir Crit Care Med 2006;173:1390-413. [Crossref] [PubMed]
- Benzo R, Kelley GA, Recchi L, et al. Complications of lung resection and exercise capacity: a meta-analysis. Respir Med 2007;101:1790-7. [Crossref] [PubMed]
- Brutsche MH, Spiliopoulos A, Bolliger CT, et al. Exercise capacity and extent of resection as predictors of surgical risk in lung cancer. Eur Respir J 2000;15:828-32. [Crossref] [PubMed]
- Fang Y, Zhao Q, Huang D. The impact of exercise training on surgery tolerability in lung cancer patients with impaired pulmonary function. Chinese Journal of Rehabilitation Medicine 2013;28:619-23.
- Divisi D, Di Francesco C, Di Leonardo G, et al. Preoperative pulmonary rehabilitation in patients with lung cancer and chronic obstructive pulmonary disease. Eur J Cardiothorac Surg 2013;43:293-6. [Crossref] [PubMed]
- Bagan P, Oltean V, Ben Abdesselam A, et al. Pulmonary rehabilitation and non-invasive ventilation before lung surgery in very high-risk patients. Rev Mal Respir 2013;30:414-9. [Crossref] [PubMed]
- Crandall K, Maguire R, Campbell A, et al. Exercise intervention for patients surgically treated for Non-Small Cell Lung Cancer (NSCLC): a systematic review. Surg Oncol 2014;23:17-30. [Crossref] [PubMed]
- Sahin H, Varol Y, Naz I, et al. The effect of pulmonary rehabilitation on COPD exacerbation frequency per year. Clin Respir J 2018;12:165-74. [Crossref] [PubMed]
- Naunheim KS, Wood DE, Krasna MJ, et al. Predictors of operative mortality and cardiopulmonary morbidity in the National Emphysema Treatment Trial. J Thorac Cardiovasc Surg 2006;131:43-53. [Crossref] [PubMed]
- Salvi R, Meoli I, Cennamo A, et al. Preoperative high-intensity training in frail old patients undergoing pulmonary resection for NSCLC. Open Med (Wars) 2016;11:443-8. [Crossref] [PubMed]
- Benzo R, Wigle D, Novotny P, et al. Preoperative pulmonary rehabilitation before lung cancer resection: results from two randomized studies. Lung Cancer 2011;74:441-5. [Crossref] [PubMed]
- Mahendran K, Naidu B. The key questions in rehabilitation in thoracic surgery. J Thorac Dis 2018;10:S924-30. [Crossref] [PubMed]
- Laurent H, Aubreton S, Galvaing G, et al. Preoperative respiratory muscle endurance training improves ventilatory capacity and prevents pulmonary postoperative complications after lung surgery. Eur J Phys Rehabil Med 2020;56:73-81. [Crossref] [PubMed]
- Kadiri SB, Kerr AP, Oswald NK, et al. Fit 4 surgery, a bespoke app with biofeedback delivers rehabilitation at home before and after elective lung resection. J Cardiothorac Surg 2019;14:132. [Crossref] [PubMed]
- Chamogeorgakis T, Anagnostopoulos C, Kostopanagiotou G, et al. Does anemia affect outcome after lobectomy or pneumonectomy in early stage lung cancer patients who have not received neo-adjuvant treatment? The Journal of Thoracic and Cardiovascular Surgery. 2008;56:148-153.
- Jean RA, DeLuzio MR, Kraev AI, et al. Analyzing Risk Factors for Morbidity and Mortality after Lung Resection for Lung Cancer Using the NSQIP Database. J Am Coll Surg 2016;222:992-1000.e1. [Crossref] [PubMed]
- Steuber TD, Howard ML, Nisly SA. Strategies for the Management of Postoperative Anemia in Elective Orthopedic Surgery. Ann Pharmacother 2016;50:578-85. [Crossref] [PubMed]
- Calleja JL, Delgado S, del Val A, et al. Ferric carboxymaltose reduces transfusions and hospital stay in patients with colon cancer and anemia. Int J Colorectal Dis 2016;31:543-51. [Crossref] [PubMed]
- Anile M, Venuta F, Diso D, et al. Preoperative anaemia does not affect the early postoperative outcome in patients with lung cancer. Minerva Chir 2007;62:431-5.
- Amato A, Pescatori M. Perioperative blood transfusions for the recurrence of colorectal cancer. Cochrane Database Syst Rev 2006;2006:CD005033. [Crossref] [PubMed]
- Tonia T, Mettler A, Robert N, et al. Erythropoietin or darbepoetin for patients with cancer. Cochrane Database Syst Rev 2012;12:CD003407. [Crossref] [PubMed]
- Gagné S, McIsaac DI. Modifiable risk factors for patients undergoing lung cancer surgery and their optimization: a review. J Thorac Dis 2018;10:S3761-72. [Crossref] [PubMed]
- Muñoz M, Acheson AG, Auerbach M, et al. International consensus statement on the peri-operative management of anaemia and iron deficiency. Anaesthesia 2017;72:233-47. [Crossref] [PubMed]
- Pratt JJ, Khan KS. Non-anaemic iron deficiency - a disease looking for recognition of diagnosis: a systematic review. Eur J Haematol 2016;96:618-28. [Crossref] [PubMed]
- Yoo YC, Shim JK, Kim JC, et al. Effect of single recombinant human erythropoietin injection on transfusion requirements in preoperatively anemic patients undergoing valvular heart surgery. Anesthesiology 2011;115:929-37. [Crossref] [PubMed]
- Muñoz M, Gómez-Ramírez S, Cuenca J, et al. Very-short-term perioperative intravenous iron administration and postoperative outcome in major orthopedic surgery: a pooled analysis of observational data from 2547 patients. Transfusion 2014;54:289-99. [Crossref] [PubMed]
- Richards T, Baikady RR, Clevenger B, et al. Preoperative intravenous iron to treat anaemia before major abdominal surgery (PREVENTT): a randomised, double-blind, controlled trial. Lancet 2020;396:1353-61. [Crossref] [PubMed]
- Tait A, Howell SJ. Preoperative hypertension: perioperative implications and management. BJA Educ 2021;21:426-32. [Crossref] [PubMed]
- Hartle A, McCormack T, Carlisle J, et al. The measurement of adult blood pressure and management of hypertension before elective surgery: Joint Guidelines from the Association of Anaesthetists of Great Britain and Ireland and the British Hypertension Society. Anaesthesia 2016;71:326-37. [Crossref] [PubMed]
- Poldermans D, Bax JJ, Boersma E, et al. Guidelines for pre-operative cardiac risk assessment and perioperative cardiac management in non-cardiac surgery: the Task Force for Preoperative Cardiac Risk Assessment and Perioperative Cardiac Management in Non-cardiac Surgery of the European Society of Cardiology (ESC) and endorsed by the European Society of Anaesthesiology (ESA). Eur J Anaesthesiol 2010;27:92-137. [Crossref] [PubMed]
- Hwang JW, Kim EK, Yang JH, et al. Assessment of perioperative cardiac risk of patients undergoing noncardiac surgery using coronary computed tomographic angiography. Circ Cardiovasc Imaging 2015;8:e002582. [Crossref] [PubMed]
- Lim E, Baldwin D, Beckles M, et al. Guidelines on the radical management of patients with lung cancer. Thorax 2010;65:iii1-27. [Crossref] [PubMed]
- Kristensen SD, Knuuti J, Saraste A, et al. 2014 ESC/ESA Guidelines on non-cardiac surgery: cardiovascular assessment and management: The Joint Task Force on non-cardiac surgery: cardiovascular assessment and management of the European Society of Cardiology (ESC) and the European Society of Anaesthesiology (ESA). Eur Heart J 2014;35:2383-431. [Crossref] [PubMed]
- Sakai T, Yahagi K, Miura S, et al. Transcatheter aortic valve implantation for patients with lung cancer and aortic valve stenosis. J Thorac Dis 2018;10:E387-90. [Crossref] [PubMed]
- Fleisher LA, Fleischmann KE, Auerbach AD, et al. 2014 ACC/AHA guideline on perioperative cardiovascular evaluation and management of patients undergoing noncardiac surgery: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation 2014;130:2215-45. [Crossref] [PubMed]
- Smilowitz NR, Lorin J, Berger JS. Risks of noncardiac surgery early after percutaneous coronary intervention. Am Heart J 2019;217:64-71. [Crossref] [PubMed]
- McFalls EO, Ward HB, Moritz TE, et al. Coronary-artery revascularization before elective major vascular surgery. N Engl J Med 2004;351:2795-804. [Crossref] [PubMed]
- Hernandez AF, Whellan DJ, Stroud S, et al. Outcomes in heart failure patients after major noncardiac surgery. J Am Coll Cardiol 2004;44:1446-53. [Crossref] [PubMed]
- van Diepen S, Bakal JA, McAlister FA, et al. Mortality and readmission of patients with heart failure, atrial fibrillation, or coronary artery disease undergoing noncardiac surgery: an analysis of 38 047 patients. Circulation 2011;124:289-96. [Crossref] [PubMed]
- Brunelli A, Ferguson MK, Salati M, et al. Thoracic Revised Cardiac Risk Index Is Associated With Prognosis After Resection for Stage I Lung Cancer. Ann Thorac Surg 2015;100:195-200. [Crossref] [PubMed]
- Healy KO, Waksmonski CA, Altman RK, et al. Perioperative outcome and long-term mortality for heart failure patients undergoing intermediate- and high-risk noncardiac surgery: impact of left ventricular ejection fraction. Congest Heart Fail 2010;16:45-9. [Crossref] [PubMed]
- Thomas DC, Blasberg JD, Arnold BN, et al. Validating the Thoracic Revised Cardiac Risk Index Following Lung Resection. Ann Thorac Surg 2017;104:389-94. [Crossref] [PubMed]
- Lee TH, Marcantonio ER, Mangione CM, et al. Derivation and prospective validation of a simple index for prediction of cardiac risk of major noncardiac surgery. Circulation 1999;100:1043-9. [Crossref] [PubMed]
- Brunelli A, Varela G, Salati M, et al. Recalibration of the revised cardiac risk index in lung resection candidates. Ann Thorac Surg 2010;90:199-203. [Crossref] [PubMed]
- Takegahara K, Usuda J, Inoue T, et al. Preoperative management using inhalation therapy for pulmonary complications in lung cancer patients with chronic obstructive pulmonary disease. Gen Thorac Cardiovasc Surg 2017;65:388-91. [Crossref] [PubMed]
- Bölükbas S, Eberlein M, Eckhoff J, et al. Short-term effects of inhalative tiotropium/formoterol/budenoside versus tiotropium/formoterol in patients with newly diagnosed chronic obstructive pulmonary disease requiring surgery for lung cancer: a prospective randomized trial. Eur J Cardiothorac Surg 2011;39:995-1000. [Crossref] [PubMed]
- Mizuno Y, Shirahashi K, Yamamoto H, et al. Efficacy of preoperative inhaled LAMA/LABA combinations in patients with lung cancer and untreated COPD. Minerva Surg 2021;76:592-7. [Crossref] [PubMed]
- Ju NY, Gao H, Huang W, et al. Therapeutic effect of inhaled budesonide (Pulmicort® Turbuhaler) on the inflammatory response to one-lung ventilation. Anaesthesia 2014;69:14-23. [Crossref] [PubMed]
- Kaufmann KB, Heinrich S, Staehle HF, et al. Perioperative cytokine profile during lung surgery predicts patients at risk for postoperative complications-A prospective, clinical study. PLoS One 2018;13:e0199807. [Crossref] [PubMed]
- Licker M, Tschopp JM, Robert J, et al. Aerosolized salbutamol accelerates the resolution of pulmonary edema after lung resection. Chest 2008;133:845-52. [Crossref] [PubMed]
- Manocha S, Gordon AC, Salehifar E, et al. Inhaled beta-2 agonist salbutamol and acute lung injury: an association with improvement in acute lung injury. Crit Care 2006;10:R12. [Crossref] [PubMed]
- Shin SH, Shin S, Im Y, et al. Effect of perioperative bronchodilator therapy on postoperative pulmonary function among lung cancer patients with COPD. Sci Rep 2021;11:8359. [Crossref] [PubMed]
- Kobayashi S, Suzuki S, Niikawa H, et al. Preoperative use of inhaled tiotropium in lung cancer patients with untreated COPD. Respirology 2009;14:675-9. [Crossref] [PubMed]
- Makino T, Otsuka H, Hata Y, et al. Long-acting muscarinic antagonist and long-acting β2-agonist therapy to optimize chronic obstructive pulmonary disease prior to lung cancer surgery. Mol Clin Oncol 2018;8:647-52. [Crossref] [PubMed]
- Motoishi M, Sawai S, Hori T, et al. The preoperative HbA1c level is an independent prognostic factor for the postoperative survival after resection of non-small cell lung cancer in elderly patients. Surg Today 2018;48:517-24. [Crossref] [PubMed]
- Buchleitner AM, Martínez-Alonso M, Hernández M, et al. Perioperative glycaemic control for diabetic patients undergoing surgery. Cochrane Database Syst Rev 2012;CD007315. [Crossref] [PubMed]
- Rollins KE, Varadhan KK, Dhatariya K, et al. Systematic review of the impact of HbA1c on outcomes following surgery in patients with diabetes mellitus. Clin Nutr 2016;35:308-16. [Crossref] [PubMed]
- Wang YY, Hu SF, Ying HM, et al. Postoperative tight glycemic control significantly reduces postoperative infection rates in patients undergoing surgery: a meta-analysis. BMC Endocr Disord 2018;18:42. [Crossref] [PubMed]
- Kotagal M, Symons RG, Hirsch IB, et al. Perioperative hyperglycemia and risk of adverse events among patients with and without diabetes. Ann Surg 2015;261:97-103. [Crossref] [PubMed]
- World Health Organization. Alcohol. Accessed 17 June, 2022. Available online: https://www.who.int/news-room/fact-sheets/detail/alcohol
- Tønnesen H, Nielsen PR, Lauritzen JB, et al. Smoking and alcohol intervention before surgery: evidence for best practice. Br J Anaesth 2009;102:297-306. [Crossref] [PubMed]
- Egholm JW, Pedersen B, Møller AM, et al. Perioperative alcohol cessation intervention for postoperative complications. Cochrane Database Syst Rev 2018;11:CD008343. [Crossref] [PubMed]
- Neuenschwander AU, Pedersen JH, Krasnik M, et al. Impaired postoperative outcome in chronic alcohol abusers after curative resection for lung cancer. Eur J Cardiothorac Surg 2002;22:287-91. [Crossref] [PubMed]
- Jørgensen CH, Pedersen B, Tønnesen H. The efficacy of disulfiram for the treatment of alcohol use disorder. Alcohol Clin Exp Res 2011;35:1749-58. [Crossref] [PubMed]
- Graf SA, Zeliadt SB, Rise PJ, et al. Unhealthy alcohol use is associated with postoperative complications in veterans undergoing lung resection. J Thorac Dis 2018;10:1648-56. [Crossref] [PubMed]
- Prokopidis K, Witard OC. Understanding the role of smoking and chronic excess alcohol consumption on reduced caloric intake and the development of sarcopenia. Nutr Res Rev 2022;35:197-206. [Crossref] [PubMed]
Cite this article as: Ahmed-Issap A, Mahendran K, Abah U. Optimisation of the high-risk thoracic surgical patient: a narrative review. Shanghai Chest 2023;7:5.


